北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (4): 771-779. doi: 10.19723/j.issn.1671-167X.2020.04.032
机器人辅助腹腔镜上尿路修复手术:单一术者108例经验总结
程嗣达1,李新飞1,熊盛炜1,樊书菠1,王杰1,朱伟杰1,李子奡1,丁光璞1,俞婷2,李万强3,孙永明4,杨昆霖1,张雷1,郝瀚1,△( ),李学松1,△(
),李学松1,△( ),周利群1
),周利群1
- 1.北京大学第一医院泌尿外科,北京大学泌尿外科研究所,国家泌尿、男性生殖系肿瘤研究中心,北京 100034
2.三明市第二医院泌尿外科,福建三明 366000
3.三峡大学第一临床医学院/宜昌市中心人民医院泌尿外科,湖北宜昌 443003
4.南京鼓楼医院集团宿迁市人民医院泌尿外科,江苏宿迁 223800
Robot-assisted laparoscopic upper urinary tract reconstruction surgery: A review of 108 cases by a single surgeon
Si-da CHENG1,Xin-fei LI1,Sheng-wei XIONG1,Shu-bo FAN1,Jie WANG1,Wei-jie ZHU1,Zi-ao LI1,Guang-pu DING1,Ting YU2,Wan-qiang LI3,Yong-ming SUN4,Kun-lin YANG1,Lei ZHANG1,Han HAO1,△( ),Xue-song LI1,△(
),Xue-song LI1,△( ),Li-qun ZHOU1
),Li-qun ZHOU1
- 1. Department of Urology, Peking University First Hospital; Institute of Urology, Peking University; National Urological Cancer Center, Beijing 100034, China
2. Department of Urology, The Second Hospital of Sanming, Sanming 366000, Fujian, China
3. Department of Urology, The First College of Clinical Medical Science, Three Gorges University/Yichang Central People’s Hospital, Yichang 443003, Hubei, China
4. Department of Urology, Suqian People’s Hospital of Nanjing Drum Tower Hospital Group, Suqian 223800, Jiangsu, China
摘要:
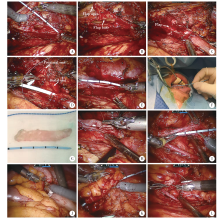
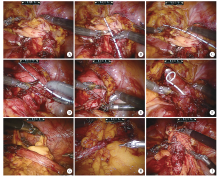
目的: 总结分析单一术者机器人辅助腹腔镜上尿路修复手术的技术经验及治疗效果。方法: 回顾性分析2018年11月至2020年1月由单一术者完成的108例机器人辅助腹腔镜上尿路修复手术的临床资料,包括改良后离断肾盂成形术53例、肾盂瓣成形术11例、输尿管狭窄段切除再吻合术11例、输尿管狭窄切开自体舌黏膜修补术5例、输尿管狭窄切开阑尾补片修复术4例、输尿管膀胱再植术11例、术中精确测量法膀胱悬吊翻瓣术6例和改良回肠代输尿管术7例。手术成功定义为主观症状缓解且泌尿系超声提示肾积水缓解。结果: 108例手术均成功完成,无中转普通腹腔镜及开放手术。改良后离断肾盂成形术,中位手术时间141 min(74~368 min),中位出血量20 mL(10~350 mL),中位术后住院时间4 d(3~19 d),手术成功率为94.3%。肾盂瓣成形术,中位手术时间159 min(110~222 min),中位出血量50 mL(20~150 mL),中位术后住院时间5 d(3~8 d),手术成功率为100%。输尿管狭窄段切除再吻合术,中位手术时间126 min(76~160 min),中位术中出血量20 mL(10~50 mL),中位术后住院时间5 d(4~9 d),手术成功率为100%。输尿管狭窄切开自体舌黏膜补片修补术,中位手术时间204 min(154~250 min),中位出血量30 mL(10~100 mL),中位术后住院时间6 d(4~7 d),手术成功率为100%。输尿管狭窄切开阑尾补片修复术,中位手术时间164 min(135~211 min),中位手术出血量75 mL(50~200 mL),中位术后住院日8.5 d(6~12 d),手术成功率为100%。输尿管膀胱再植术,中位手术时间149 min(100~218 min),中位术中出血量20 mL(10~50 mL),中位术后住院日7 d(5~10 d),手术成功率为90.9%。术中精确测量法膀胱悬吊翻瓣术,中位手术时间166 min(137~205 min),中位手术出血45 mL(20~100 mL),中位术后住院时间5 d(4~41 d),手术成功率为83.3%。改良回肠代输尿管手术,中位手术时间270 min(227~335 min),中位术中出血量100 mL(10~100 mL),中位术后住院时间7 d(5~26 d),手术成功率为85.7%。结论: 本研究中单一术者应用机器人辅助腹腔镜开展并改良了多种复杂上尿路修复手术术式,对进一步形成标准化、程序化上尿路修复手术方式提供了参考。
中图分类号:
- R693.2
| [1] | Stief CG, Jonas U, Petry KU, et al. Ureteric reconstruction[J]. BJU Int, 2003,91(2):138-142. |
| [2] |
Mufarrij PW, Shah OD, Berger AD, et al. Robotic reconstruction of the upper urinary tract[J]. J Urol, 2007,178(5):2002-2005.
pmid: 17869303 |
| [3] | 赵海岳, 叶雄俊, 陈伟男, 等. 腹腔镜肾盂成型术中异位血管的处理方法[J]. 北京大学学报(医学版), 2019,51(4):660-664. |
| [4] | Wang J, Xiong SW, Fan SB, et al. Appendiceal onlay flap ure-teroplasty for the treatment of complex ureteral strictures: Initial experience of nine patients [J/OL]. J Endourol, (2020-04-23)[2020-05-07]. doi: 10.1089/end.2020.0176. |
| [5] |
Yang K, Yao L, Li X, et al. A modified suture technique for transperitoneal laparoscopic dismembered pyeloplasty of pelviureteric junction obstruction[J]. Urology, 2015,85(1):263-267.
pmid: 25530399 |
| [6] | Hong P, Cai Y, Li Z, et al. Modified laparoscopic partial urete-rectomy for adult ureteral fibroepithelial polyp: Technique and initial experience[J]. Urol Int, 2019,102(1):13-19. |
| [7] | Zhong W, Hong P, Ding G, et al. Technical considerations and outcomes for ileal ureter replacement: a retrospective study in China[J]. BMC Surg, 2019,19(1):9. |
| [8] | 丁光璞, 程嗣达, 方冬, 等. 上尿路微创手术的技术改良[J]. 北京大学学报(医学版), 2019,51(4):610-614. |
| [9] |
Autorino R, Eden C, El-Ghoneimi A, et al. Robot-assisted and laparoscopic repair of ureteropelvic junction obstruction: a syste-matic review and meta-analysis[J]. Eur Urol, 2014,65(2):430-452.
doi: 10.1016/j.eururo.2013.06.053 pmid: 23856037 |
| [10] |
Hong P, Li Z, Zhu D, et al. A simple modification for the usage of flexible cystoscope in modified laparoscopic pyeloplasty for ure-teropelvic junction obstruction with renal calculi: A flexible guiding tube[J]. Urol Int, 2019,102(3):262-268.
pmid: 30630187 |
| [11] | 丁光璞, 彭意吉, 杨昆霖, 等. 改良经腹腹腔镜肾盂成形术联合孙氏镜治疗UPJO合并肾结石的初步经验[J]. 中华泌尿外科杂志, 2019,40(9):680-684. |
| [12] | 许小林, 徐月敏, 朱开常, 等. 采用旋转带蒂肾盂瓣输尿管扩大成形术治疗上段输尿管超长段狭窄[J]. 中华临床医师杂志: 电子版, 2011,5(24):7417-7418. |
| [13] | 熊盛炜, 杨昆霖, 丁光璞, 等. 输尿管损伤外科修复治疗的研究进展[J]. 北京大学学报(医学版), 2019,51(4):783-788. |
| [14] |
Sun G, Yan L, Ouyang W, et al. Management for ureteral stenosis: A comparison of robot-assisted laparoscopic ureteroureterostomy and conventional laparoscopic ureteroureterostomy[J]. J Laparoendosc Adv Surg Tech A, 2019,29(9):1111-1115.
pmid: 31314664 |
| [15] |
Lee Z, Simhan J, Parker DC, et al. Novel use of indocyanine green for intraoperative, real-time localization of ureteral stenosis during robot-assisted ureteroureterostomy[J]. Urology, 2013,82(3):729-733.
pmid: 23987169 |
| [16] |
Tang ZY, Chen Z, He Y, et al. Laparoendoscopic single-site ureteroureterostomy with intraoperative retrograde ureteroscopy-assisted technique for benign proximal and middle ureteral strictures: A single-center experience[J]. J Laparoendosc Adv Surg Tech A, 2014,24(7):493-496.
pmid: 24844653 |
| [17] | Eisenberg ML, Lee KL, Zumrutbas AE, et al. Long-term outcomes and late complications of laparoscopic nephrectomy with renal autotransplantation[J]. J Urol, 2008,179(1):240-243. |
| [18] |
Kocot A, Kalogirou C, Vergho D, et al. Long-term results of ileal ureteric replacement: A 25-year single-centre experience[J]. BJU Int, 2017,120(2):273-279.
pmid: 28220579 |
| [19] |
Zhao LC, Weinberg AC, Lee Z, et al. Robotic ureteral reconstruction using buccal mucosa grafts: A multi-institutional expe-rience[J]. Eur Urol, 2018,73(3):419-426.
doi: 10.1016/j.eururo.2017.11.015 pmid: 29239749 |
| [20] |
Dublin N, Stewart LH. Oral complications after buccal mucosal graft harvest for urethroplasty[J]. BJU Int, 2004,94(6):867-869.
pmid: 15476524 |
| [21] |
Li B, Xu Y, Hai B, et al. Laparoscopic onlay lingual mucosal graft ureteroplasty for proximal ureteral stricture: initial experience and 9-month follow-up[J]. Int Urol Nephrol, 2016,48(8):1275-1279.
doi: 10.1007/s11255-016-1289-9 pmid: 27115158 |
| [22] |
Duty BD, Kreshover JE, Richstone L, et al. Review of appendiceal onlay flap in the management of complex ureteric strictures in six patients[J]. BJU Int, 2015,115(2):282-287.
pmid: 24471943 |
| [23] | 王亮, 张国玺, 邹晓峰. 腹腔镜输尿管膀胱再植术的研究进展[J]. 赣南医学院学报, 2019,39(2):195-199. |
| [24] |
Stein R, Rubenwolf P, Ziesel C, et al. Psoas hitch and Boari flap ureteroneocystostomy[J]. BJU Int, 2013,112(1):137-155.
pmid: 23759011 |
| [25] | Zhong W, Du Y, Yang K, et al. Ileal ureter replacement combined with Boari flap-Psoas hitch to treat full-length ureteral defects: Technique and initial experience[J]. Urology, 2017(108):201-206. |
| [26] |
Stein RJ, Turna B, Patel NS, et al. Laparoscopic assisted ileal ureter: technique, outcomes and comparison to the open procedure[J]. J Urol, 2009,182(3):1032-1039.
doi: 10.1016/j.juro.2009.05.013 pmid: 19616806 |
| [27] | Ubrig B, Janusonis J, Paulics L, et al. Functional outcome of completely intracorporeal robotic ileal ureteric replacement[J]. Urology, 2018(114):193-197. |
| [1] | 陈思鹭, 王海菊, 吴宇财, 李志华, 黄燕波, 何宇辉, 许洋洋, 李学松, 贯华. 成人肾积水病因分析:一项单中心横断面研究[J]. 北京大学学报(医学版), 2024, 56(5): 913-918. |
| [2] | 张树栋,谢睿扬. 机器人手术时代的肾癌合并腔静脉瘤栓治疗策略[J]. 北京大学学报(医学版), 2024, 56(4): 562-564. |
| [3] | 应沂岑,杜毅聪,李志华,张一鸣,李新飞,王冰,张鹏,朱宏建,周利群,杨昆霖,李学松. 机器人辅助腹腔镜下颊黏膜补片输尿管成形术治疗复杂输尿管狭窄[J]. 北京大学学报(医学版), 2024, 56(4): 640-645. |
| [4] | 毛海,张帆,张展奕,颜野,郝一昌,黄毅,马潞林,褚红玲,张树栋. 基于MRI前列腺腺体相关参数构建腹腔镜前列腺癌术后尿失禁的预测模型[J]. 北京大学学报(医学版), 2023, 55(5): 818-824. |
| [5] | 邱敏,宗有龙,王滨帅,杨斌,徐楚潇,孙争辉,陆敏,赵磊,卢剑,刘承,田晓军,马潞林. 腹腔镜肾部分切除术治疗中高复杂程度肾肿瘤的效果[J]. 北京大学学报(医学版), 2023, 55(5): 833-837. |
| [6] | 刘慧丽,吕彦函,王晓晓,李民. 老年患者腹腔镜泌尿系肿瘤根治术后慢性疼痛的影响因素[J]. 北京大学学报(医学版), 2023, 55(5): 851-856. |
| [7] | 马建勋,夏有辰,李比,赵红梅,雷玉涛,布希. 乳腺癌改良根治术后即刻乳房重建的方式选择[J]. 北京大学学报(医学版), 2023, 55(4): 612-618. |
| [8] | 张铃福,侯纯升,徐智,王立新,凌晓锋,王港,崔龙,修典荣. 腹腔镜下经胆囊管胆管引流联合胆总管探查取石术治疗复杂胆管结石的临床效果[J]. 北京大学学报(医学版), 2022, 54(6): 1185-1189. |
| [9] | 周利群,徐纯如. 机器人时代中央型肾肿瘤的手术治疗策略[J]. 北京大学学报(医学版), 2022, 54(4): 587-591. |
| [10] | 张崔建,何志嵩,周利群. 上尿路尿路上皮癌的淋巴清扫[J]. 北京大学学报(医学版), 2022, 54(4): 592-594. |
| [11] | 戴翔,王飞,杜依青,宋宇轩,徐涛. 上尿路尿路上皮癌组织中脂肪因子表达与临床病理特征及预后的相关性[J]. 北京大学学报(医学版), 2022, 54(4): 605-614. |
| [12] | 李志华,徐纯如,刘颖,贯华,张萌,车新艳,唐琦,黄燕波,李学松,周利群. 饮水习惯与上尿路尿路上皮癌病理特征的相关性分析[J]. 北京大学学报(医学版), 2022, 54(4): 621-627. |
| [13] | 左炜,高菲,袁昌巍,熊盛炜,李志华,张雷,杨昆霖,李新飞,刘靓,魏来,张鹏,王冰,谷亚明,朱宏建,赵峥,李学松. 基于多中心数据库的10年上尿路修复手术术式及术型变化趋势[J]. 北京大学学报(医学版), 2022, 54(4): 692-698. |
| [14] | 安立哲,熊六林,陈亮,王焕瑞,陈伟男,黄晓波. 腹腔镜肾盂成形术联合肾盂镜超声碎石取石术治疗肾盂输尿管连接部梗阻合并肾结石[J]. 北京大学学报(医学版), 2022, 54(4): 746-750. |
| [15] | 张帆,陈曲,郝一昌,颜野,刘承,黄毅,马潞林. 术前及术后膜性尿道长度与腹腔镜根治性前列腺切除术后控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2022, 54(2): 299-303. |
|
||