北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (4): 794-798. doi: 10.19723/j.issn.1671-167X.2020.04.036
• 综述 • 上一篇
二次肾盂成形术在复发性肾盂输尿管连接部梗阻中的研究进展
- 北京大学第一医院泌尿外科,北京大学泌尿外科研究所,国家泌尿、男性生殖系肿瘤研究中心,北京 100034
Advance in re-do pyeloplasty for the management of recurrent ureteropelvic junction obstruction after surgery
Sheng-wei XIONG,Jie WANG,Wei-jie ZHU,Si-da CHENG,Lei ZHANG,Xue-song LI( ),Li-qun ZHOU
),Li-qun ZHOU
- Department of Urology, Peking University First Hospital; Institute of Urology, Peking University; National Urological Cancer Center; Beijing 100034, China
中图分类号:
- R691.2
| [1] |
Moon DA, El-Shazly MA, Chang CM, et al. Laparoscopic pyeloplasty: evolution of a new gold standard[J]. Urology, 2006,67(5):932-936.
pmid: 16635516 |
| [2] |
Sukumar S, Sun M, Karakiewicz PI, et al. National trends and disparities in the use of minimally invasive adult pyeloplasty[J]. J Urol, 2012,188(3):913-918.
doi: 10.1016/j.juro.2012.05.013 pmid: 22819404 |
| [3] | Swearingen R, Ambani S, Faerber GJ, et al. Definitive management of failure after pyeloplasty[J]. J Endourol, 2016,30(Suppl 1):S23-27. |
| [4] |
Romao RLP, Koyle MA, Pippi Salle JL, et al. Failed pyeloplasty in children: revisiting the unknown[J]. Urology, 2013,82(5):1145-1147.
doi: 10.1016/j.urology.2013.06.049 pmid: 24035031 |
| [5] |
Shapiro EY, Cho JS, Srinivasan A, et al. Long-term follow-up for salvage laparoscopic pyeloplasty after failed open pyeloplasty[J]. Urology, 2009,73(1):115-118.
doi: 10.1016/j.urology.2008.08.483 pmid: 18950836 |
| [6] |
Braga LH, Lorenzo AJ, Skeldon S, et al. Failed pyeloplasty in children: comparative analysis of retrograde endopyelotomy versus redo pyeloplasty[J]. J Urol, 2007,178(6):2571-2575.
doi: 10.1016/j.juro.2007.08.050 pmid: 17945304 |
| [7] |
Poulakis V, Witzsch U, Schultheiss D, et al. History of ureteropelvic junction obstruction repair (pyeloplasty). From Trendelenburg (1886) to the present[J]. Urologe A, 2004,43(12):1544-1559.
doi: 10.1007/s00120-004-0663-x pmid: 15316607 |
| [8] |
Khan F, Ahmed K, Lee N, et al. Management of ureteropelvic junction obstruction in adults[J]. Nat Rev Urol, 2014,11(11):629-638.
doi: 10.1038/nrurol.2014.240 pmid: 25287785 |
| [9] |
O’Reilly PH, Brooman PJ, Mak S, et al. The long-term results of Anderson-Hynes pyeloplasty[J]. BJU Int, 2001,87(4):287-289.
pmid: 11251517 |
| [10] |
Gogus C, Karamursel T, Tokatli Z, et al. Long-term results of Anderson-Hynes pyeloplasty in 180 adults in the era of endourolo-gic procedures[J]. Urol Int, 2004,73(1):11-14.
doi: 10.1159/000078796 pmid: 15263785 |
| [11] | Inagaki T, Rha KH, Ong AM, et al. Laparoscopic pyeloplasty: current status[J]. BJU Int, 2005,95(Suppl 2):102-105. |
| [12] | Badawy H, Zoaier A, Ghoneim T, et al. Transperitoneal versus retroperitoneal laparoscopic pyeloplasty in children: Randomized clinical trial [J]. J Pediatr Urol, 2015, 11(3): 122.e1-6. |
| [13] |
Yang K, Yao L, Li X, et al. A modified suture technique for transperitoneal laparoscopic dismembered pyeloplasty of pelviu-reteric junction obstruction[J]. Urology, 2015,85(1):263-267.
pmid: 25530399 |
| [14] |
Tan HJ, Ye Z, Roberts WW, et al. Failure after laparoscopic pyeloplasty: prevention and management[J]. J Endourol, 2011,25(9):1457-1462.
doi: 10.1089/end.2010.0647 |
| [15] |
Rassweiler JJ, Subotic S, Feist-Schwenk M, et al. Minimally invasive treatment of ureteropelvic junction obstruction: long-term experience with an algorithm for laser endopyelotomy and laparoscopic retroperitoneal pyeloplasty[J]. J Urol, 2007,177(3):1000-1005.
doi: 10.1016/j.juro.2006.10.049 pmid: 17296396 |
| [16] | Abdrabuh AM, Salih EM, Aboelnasr M, et al. Endopyelotomy versus redo pyeoloplasty for management of failed pyeloplasty in children: A single center experience[J]. J Pediatr Surg, 2018,53(11):2250-2255. |
| [17] | Braga LHP, Lorenzo AJ, Bägli DJ, et al. Risk factors for recurrent ureteropelvic junction obstruction after open pyeloplasty in a large pediatric cohort[J]. J Urol, 2008,180(4 Suppl):1684-1688. |
| [18] |
Vemulakonda VM, Wilcox DT, Crombleholme TM, et al. Factors associated with age at pyeloplasty in children with ureteropelvic junction obstruction[J]. Pediatr Surg Int, 2015,31(9):871-877.
doi: 10.1007/s00383-015-3748-2 pmid: 26143412 |
| [19] |
Zeltser IS, Liu JB, Bagley DH. The incidence of crossing vessels in patients with normal ureteropelvic junction examined with endoluminal ultrasound[J]. J Urol, 2004,172(6 Pt 1):2304-2307.
doi: 10.1097/01.ju.0000145532.48711.f6 pmid: 15538254 |
| [20] |
Boylu U, Oommen M, Lee BR, et al. Ureteropelvic junction obstruction secondary to crossing vessels-to transpose or not? The robotic experience[J]. J Urol, 2009,181(4):1751-1755.
doi: 10.1016/j.juro.2008.11.114 pmid: 19233419 |
| [21] |
Villemagne T, Fourcade L, Camby C, et al. Long-term results with the laparoscopic transposition of renal lower pole crossing vessels[J]. J Pediatr Urol, 2015,11(4):171-174.
doi: 10.1016/j.jpurol.2015.04.012 pmid: 26052003 |
| [22] |
Rehman J, Landman J, Sundaram C, et al. Missed anterior crossing vessels during open retroperitoneal pyeloplasty: laparoscopic transperitoneal discovery and repair[J]. J Urol, 2001,166(2):593-596.
doi: 10.1016/S0022-5347(05)65990-3 |
| [23] |
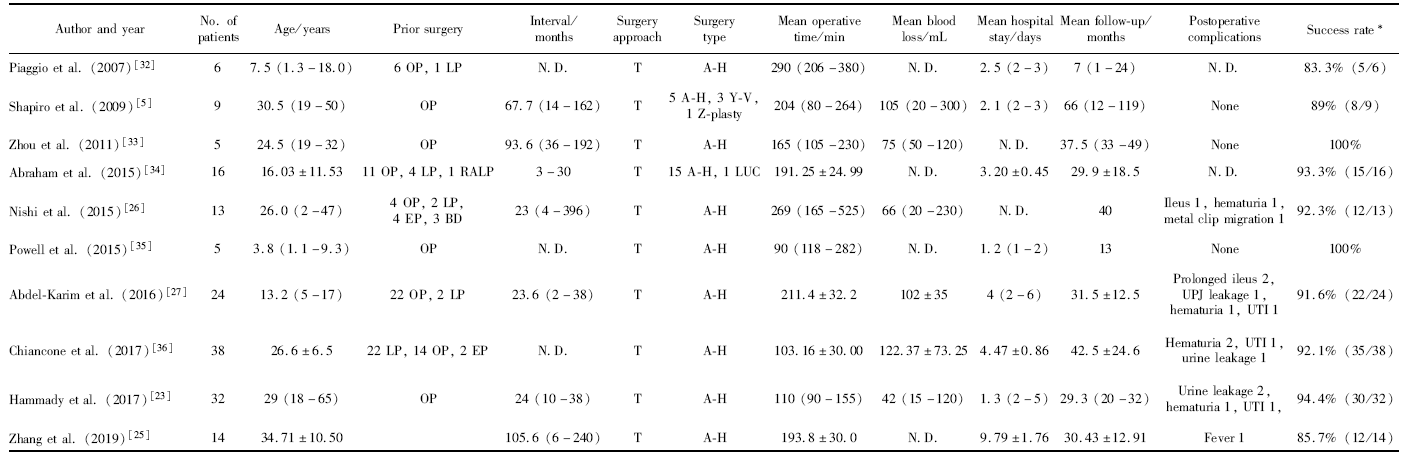
Hammady A, Elbadry MS, Rashed EN, et al. Laparoscopic repyeloplasty after failed open repair of ureteropelvic junction obstruction: a case-matched multi-institutional study[J]. Scand J Urol, 2017,51(5):402-406.
doi: 10.1080/21681805.2017.1347819 pmid: 28784012 |
| [24] |
Sundaram CP, Grubb RR, Rehman J, et al. Laparoscopic pyeloplasty for secondary ureteropelvic junction obstruction[J]. J Urol, 2003,169(6):2037-2040.
doi: 10.1097/01.ju.0000067180.78134.da pmid: 12771713 |
| [25] |
Zhang Y, Ouyang W, Xu H, et al. Secondary management for recurrent ureteropelvic junction obstruction after pyeloplasty: A comparison of re-do robot-assisted laparoscopic pyeloplasty and conventional laparoscopic pyeloplasty[J]. Urol Int, 2019,103(4):466-472.
doi: 10.1159/000503156 pmid: 31537001 |
| [26] |
Nishi M, Tsuchida M, Ikeda M, et al. Laparoscopic pyeloplasty for secondary ureteropelvic junction obstruction: long-term results[J]. Int J Urol, 2015,22(4):368-371.
doi: 10.1111/iju.12686 pmid: 25599801 |
| [27] |
Abdel-Karim AM, Fahmy A, Moussa A, et al. Laparoscopic pyeloplasty versus open pyeloplasty for recurrent ureteropelvic junction obstruction in children[J]. J Pediatr Urol, 2016,12(6):401.
doi: 10.1016/j.jpurol.2016.06.010 pmid: 27614698 |
| [28] |
Alhazmi HH. Redo laparoscopic pyeloplasty among children: A systematic review and meta-analysis[J]. Urol Ann, 2018,10(4):347-353.
doi: 10.4103/UA.UA_100_18 pmid: 30386084 |
| [29] |
Gettman MT, Neururer R, Bartsch G, et al. Anderson-Hynes dismembered pyeloplasty performed using the da Vinci robotic system[J]. Urology, 2002,60(3):509-513.
doi: 10.1016/s0090-4295(02)01761-2 pmid: 12350499 |
| [30] |
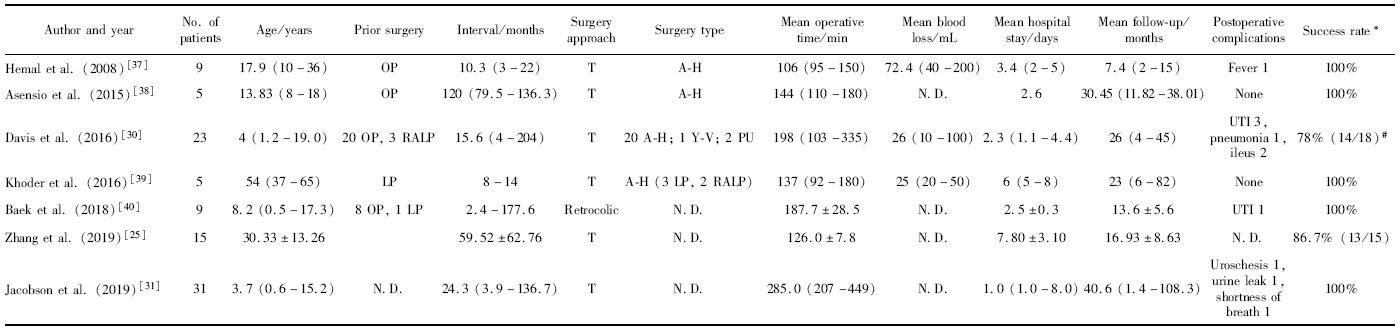
Davis TD, Burns AS, Corbett ST, et al. Reoperative robotic pyeloplasty in children [J]. J Pediatr Urol, 2016, 12(6): 394.e1-394.e7.
pmid: 27687532 |
| [31] |
Jacobson DL, Shannon R, Johnson EK, et al. Robot-assisted laparoscopic reoperative repair for failed pyeloplasty in children: An updated series[J]. J Urol, 2019,201(5):1005-1010.
doi: 10.1016/j.juro.2018.10.021 pmid: 30395839 |
| [32] | Piaggio LA, Noh PH, Gonzalez R. Reoperative laparoscopic pye-loplasty in children: comparison with open surgery[J]. J Urol, 2007,177(5):1878-1882. |
| [33] | 周利群, 张仲一, 李学松, 等. 经腹腹腔镜经肠系膜入路复发性肾盂输尿管连接部狭窄再成型术的可行性分析(附5例报告)[J]. 北京大学学报(医学版), 2011,43(4):540-543. |
| [34] |
Abraham GP, Siddaiah AT, Ramaswami K, et al. Laparoscopic management of recurrent ureteropelvic junction obstruction following pyeloplasty[J]. Urol Ann, 2015,7(2):183-187.
doi: 10.4103/0974-7796.150489 pmid: 25834982 |
| [35] | Powell C, Gatti JM, Juang D, et al. Laparoscopic pyeloplasty for ureteropelvic junction obstruction following open pyeloplasty in children[J]. J Laparoendosc Adv Surg Tech A, 2015,25(10):858-863. |
| [36] |
Chiancone F, Fedelini M, Pucci L, et al. Laparoscopic management of recurrent ureteropelvic junction obstruction following pyeloplasty: a single surgical team experience with 38 cases[J]. Int Braz J Urol, 2017,43(3):512-517.
doi: 10.1590/S1677-5538.IBJU.2016.0198 pmid: 28191792 |
| [37] |
Hemal AK, Mishra S, Mukharjee S, et al. Robot assisted laparoscopic pyeloplasty in patients of ureteropelvic junction obstruction with previously failed open surgical repair[J]. Int J Urol, 2008,15(8):744-746.
doi: 10.1111/j.1442-2042.2008.02091.x pmid: 18786197 |
| [38] |
Asensio M, Gander R, Royo GF, et al. Failed pyeloplasty in children: Is robot-assisted laparoscopic reoperative repair feasible?[J]. J Pediatr Urol, 2015,11(2):61-69.
doi: 10.1016/j.jpurol.2014.10.004 pmid: 25882184 |
| [39] |
Khoder WY, Alghamdi A, Schulz T, et al. An innovative technique of robotic-assisted/laparoscopic re-pyeloplasty in horseshoe kidney in patients with failed previous pyeloplasty for ureteropelvic junction obstruction[J]. Surg Endosc, 2016,30(9):4124-4129.
doi: 10.1007/s00464-015-4678-8 pmid: 26675936 |
| [40] |
Baek M, Silay MS, Au JK, et al. Quantifying the additional difficulty of pediatric robot-assisted laparoscopic re-do pyeloplasty: A comparison of primary and re-do procedures[J]. J Laparoendosc Adv Surg Tech A, 2018,28(5):610-616.
pmid: 29406807 |
| [41] |
Dirie NI, Ahmed MA, Wang S. Is secondary robotic pyeloplasty safe and effective as primary robotic pyeloplasty? A systematic review and meta-analysis[J]. J Robot Surg, 2020,14(2):241-248.
doi: 10.1007/s11701-019-00997-0 pmid: 31280462 |
| [42] |
Tam YH, Pang K, Wong YS, et al. From laparoscopic pyeloplasty to robot-assisted laparoscopic pyeloplasty in primary and reoperative repairs for ureteropelvic junction obstruction in children[J]. J Laparoendosc Adv Surg Tech A, 2018,28(8):1012-1018.
pmid: 29641368 |
| [1] | 姚中强,李常虹,李欣艺,郭苇,翟佳羽,刘蕊,魏慧,穆荣. 抗磷脂酰丝氨酸/凝血酶原抗体与不明原因复发性流产的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 1058-1061. |
| [2] | 安立哲,熊六林,陈亮,王焕瑞,陈伟男,黄晓波. 腹腔镜肾盂成形术联合肾盂镜超声碎石取石术治疗肾盂输尿管连接部梗阻合并肾结石[J]. 北京大学学报(医学版), 2022, 54(4): 746-750. |
| [3] | 郑蒙蒙,丁光璞,朱伟杰,杨昆霖,樊书菠,关豹,李新飞,蔡宇坤,张进生,李学松,周利群. 术前三维影像重建在治疗肾盂输尿管连接部梗阻中的应用[J]. 北京大学学报(医学版), 2020, 52(4): 705-710. |
| [4] | 熊盛炜,杨昆霖,丁光璞,郝瀚,李学松,周利群,郭应禄. 输尿管损伤外科修复治疗的研究进展[J]. 北京大学学报(医学版), 2019, 51(4): 783-789. |
| [5] | 李欣艺,赵金霞,刘湘源. 抗磷脂抗体相关性复发性流产的诊治:附75例抗磷脂综合征患者妊娠期用药和结局分析[J]. 北京大学学报(医学版), 2018, 50(6): 956-961. |
| [6] | 徐杰,庄伟达,李新炜,俞国雨,林院,罗奋棋,肖毓华. 直接前入路和后外侧保留梨状肌入路全髋关节置换术的疗效对比[J]. 北京大学学报(医学版), 2017, 49(2): 214-220. |
| [7] | 张洪,马云青. 直接前入路人工全髋关节置换术[J]. 北京大学学报(医学版), 2017, 49(2): 185-187. |
| [8] | 陈伟男,叶雄俊,刘士军,熊六林,黄晓波,徐涛,王晓峰. 三种手术方式治疗肾盂输尿管连接部梗阻的疗效及并发症比较[J]. 北京大学学报(医学版), 2016, 48(5): 817-821. |
|
||