北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (3): 465-470. doi: 10.19723/j.issn.1671-167X.2023.03.012
中国中老年人群抑郁症状、缺血性心血管疾病10年风险对心血管疾病的联合影响
- 北京大学公共卫生学院社会医学与健康教育系,北京 100191
Joint association of depression symptoms and 10-year risk of ischemic cardiovascular disease with the cardiovascular disease in middle-aged and elderly people in China
Zi-wei ZHANG,Yu-meng HUA,Ai-ping LIU*( )
)
- Department of Social Medicine and Health Education, Peking University School of Public Health, Beijing 100191, China
摘要:
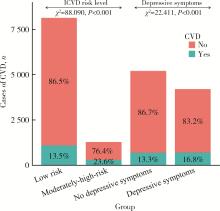
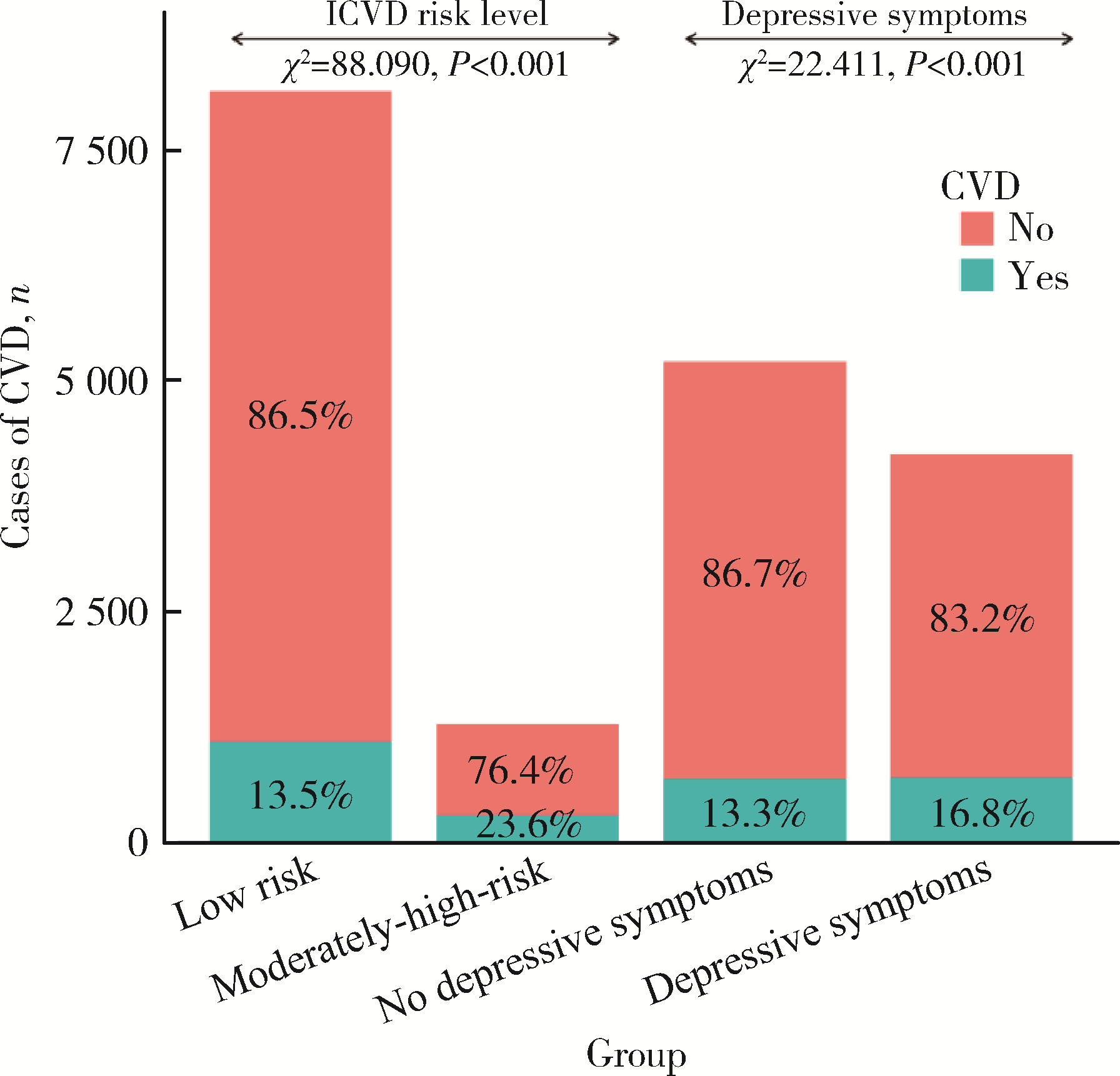
目的: 探讨抑郁症状与缺血性心血管疾病10年风险对心血管疾病(cardiovascular disease, CVD)发生的联合影响。方法: 基于中国健康与养老追踪调查(China Health and Retirement Longitudinal Study, CHARLS)数据库中的2011年基线数据和2013年、2015年、2018年随访队列数据,对2011年基线抑郁症状、缺血性心血管疾病10年风险分布特征进行描述,采用Cox生存分析模型分析抑郁症状和缺血性心血管疾病10年风险对CVD的单独、独立和联合关联。结果: 共纳入研究对象9 412例,基线抑郁症状检出率为44.7%,缺血性心血管疾病10年中高风险比例为13.62%。平均随访6.19(6.19±1.66)年中,总计观察58 258人年,1 401例中老年人发生了心血管疾病,发病密度为24.048/千人年。调整因素后,单独影响中,有抑郁症状者的CVD发生危险高(HR=1.263,95%CI: 1.133~1.408),缺血性心血管疾病10年中高风险者的CVD发生危险高(HR=1.892,95%CI: 1.662~2.154)。独立影响因素中,有抑郁症状者CVD发生危险高(HR=1.269,95%CI: 1.138~1.415),缺血性心血管疾病10年中高风险者的CVD发生危险高(HR=1.898,95%CI: 1.668~2.160)。联合影响结果显示有抑郁症状且缺血性心血管疾病10年低风险、无抑郁症状且缺血性心血管疾病10年中高风险、抑郁症状合并缺血性心血管疾病10年中高风险人群发生CVD分别是无抑郁症状且缺血性心血管疾病10年低风险人群的1.390、2.149、2.339倍(P < 0.001)。结论: 缺血性心血管疾病10年中高风险人群叠加抑郁症状会加剧中老年人心血管疾病发生的风险,结合实际开展生活方式干预和生理指标健康管理的同时,应重视中老年人群的心理健康干预。
中图分类号:
- R193.3
| 1 |
Al-Mallah MH , Sakr S , Al-Qunaibet A .Cardiorespiratory fitness and cardiovascular disease prevention: An update[J].Curr Atheroscler Rep,2018,20(1):1.
doi: 10.1007/s11883-018-0711-4 |
| 2 | 马丽媛, 王增武, 樊静, 等.《中国心血管健康与疾病报告2021》要点解读[J].中国全科医学,2022,25(27):3331-3346. |
| 3 |
Harshfield EL , Pennells L , Schwartz JE , et al.Association between depressive symptoms and incident cardiovascular diseases[J].JAMA,2020,324(23):2396-2405.
doi: 10.1001/jama.2020.23068 |
| 4 | 北京高血压防治协会, 北京糖尿病防治协会, 北京慢性病防治与健康教育研究会, 等.基层心血管病综合管理实践指南2020[J].中国医学前沿杂志(电子版),2020,12(8):1-73. |
| 5 |
Chia CW , Egan JM , Ferrucci L .Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk[J].Circ Res,2018,123(7):886-904.
doi: 10.1161/CIRCRESAHA.118.312806 |
| 6 |
Kondo T , Nakano Y , Adachi S , et al.Effects of tobacco smoking on cardiovascular disease[J].Circ J,2019,83(10):1980-1985.
doi: 10.1253/circj.CJ-19-0323 |
| 7 | 张曾航, 郭晓雷, 殷召雪, 等.血压在体质指数与心血管疾病发生风险间的中介效应[J].中国公共卫生,2023,39(3):330-334. |
| 8 |
Glovaci D , Fan W , Wong ND .Epidemiology of diabetes mellitus and cardiovascular disease[J].Curr Cardiol Rep,2019,21(4):21.
doi: 10.1007/s11886-019-1107-y |
| 9 |
Kaze AD , Santhanam P , Musani SK , et al.Metabolic dyslipidemia and cardiovascular outcomes in type 2 diabetes mellitus: Findings from the look ahead study[J].J Am Heart Assoc,2021,10(7):e016947.
doi: 10.1161/JAHA.120.016947 |
| 10 |
李贤, 赵连成, 李莹, 等.缺血性心脑血管病10年发病预测模型的验证[J].中华心血管病杂志,2007,35(8):761-764.
doi: 10.3760/j.issn:0253-3758.2007.08.018 |
| 11 | 国家"十五"攻关"冠心病、脑卒中综合危险度评估及干预方案的研究"课题组.国人缺血性心血管病发病危险的评估方法及简易评估工具的开发研究[J].中华心血管病杂志,2003,31(12):16-24. |
| 12 |
Andresen EM , Malmgren JA , Carter WB , et al.Screening for depression in well older adults: Evaluation of a short form of the CES-D (center for epidemiologic studies depression scale)[J].Am J Prev Med,1994,10(2):77-84.
doi: 10.1016/S0749-3797(18)30622-6 |
| 13 | Bragg F , Li L , Bennett D , et al.Association of random plasma glucose levels with the risk for cardiovascular disease among Chinese adults without known diabetes[J].JAMA Cardiol,2016,1(7):813-823. |
| 14 | Iso H , Cui R , Takamoto I , et al.Risk classification for metabolic syndrome and the incidence of cardiovascular disease in japan with low prevalence of obesity: A pooled analysis of 10 prospective cohort studies[J].J Am Heart Assoc,2021,10(23):e020760. |
| 15 | Talaei M , Sarrafzadegan N , Sadeghi M , et al.Incidence of cardio-vascular diseases in an iranian population: The isfahan cohort study[J].Arch Iran Med,2013,16(3):138-144. |
| 16 | Sun Y , Zhang H , Wang B , et al.Joint exposure to positive affect, life satisfaction, broad depression, and neuroticism and risk of cardiovascular diseases: A prospective cohort study[J].Atherosclerosis,2022,359,44-51. |
| 17 | Li H , Zheng D , Li Z , et al.Association of depressive symptoms with incident cardiovascular diseases in middle-aged and older Chinese adults[J].JAMA Netw Open,2019,2(12):e1916591. |
| 18 | Hamieh N , Meneton P , Wiernik E , et al.Depression, treatable cardiovascular risk factors and incident cardiac events in the gazel cohort[J].Int J Cardiol,2019,284,90-95. |
| [1] | 陈敬,单蕊,肖伍才,张晓蕊,刘峥. 青春期和成年早期自制力与抑郁症状和超重肥胖共病风险的关联:基于全国调查的十年前瞻性队列研究[J]. 北京大学学报(医学版), 2024, 56(3): 397-402. |
| [2] | 陈楚云,孙蓬飞,赵静,贾佳,范芳芳,王春燕,李建平,姜一梦,霍勇,张岩. 北京社区人群促红细胞生成素相关因素及其与10年心血管疾病风险的关系[J]. 北京大学学报(医学版), 2023, 55(6): 1068-1073. |
| [3] | 祝春素,连至炜,崔一民. 中国中老年人抑郁和慢性病的关联[J]. 北京大学学报(医学版), 2023, 55(4): 606-611. |
| [4] | 王婷,李乔晟,刘皓冉,简伟研. 人格特征、城乡差异与抑郁症状变化的关系[J]. 北京大学学报(医学版), 2023, 55(3): 385-391. |
| [5] | 张云静,乔丽颖,祁萌,严颖,亢伟伟,刘国臻,王明远,席云峰,王胜锋. 乳腺癌患者新发心血管疾病预测模型的建立与验证:基于内蒙古区域医疗数据[J]. 北京大学学报(医学版), 2023, 55(3): 471-479. |
| [6] | 张明露,刘秋萍,巩超,王佳敏,周恬静,刘晓非,沈鹏,林鸿波,唐迅,高培. 阿司匹林用于心血管病一级预防的不同策略比较:一项马尔可夫模型研究[J]. 北京大学学报(医学版), 2023, 55(3): 480-487. |
| [7] | 董尔丹. 心血管受体的信号转导与疾病[J]. 北京大学学报(医学版), 2022, 54(5): 796-802. |
| [8] | 郭子宁, 梁志生, 周仪, 张娜, 黄捷. 基于国际疾病分类的心血管疾病亚型的基因组学研究[J]. 北京大学学报(医学版), 2021, 53(3): 453-459. |
| [9] | 刘秋萍,陈汐瑾,王佳敏,刘晓非,司亚琴,梁靖媛,沈鹏,林鸿波,唐迅,高培. 基于马尔可夫模型的社区人群心血管病筛查策略的效果评价[J]. 北京大学学报(医学版), 2021, 53(3): 460-466. |
| [10] | 陈家丽,金月波,王一帆,张晓盈,李静,姚海红,何菁,李春. 老年发病类风湿关节炎的临床特征及其心血管疾病危险因素分析:一项大样本横断面临床研究[J]. 北京大学学报(医学版), 2020, 52(6): 1040-1047. |
| [11] | 徐涛,韩敬丽,姚伟娟. 雄激素剥夺治疗相关心血管疾病的机制与临床对策[J]. 北京大学学报(医学版), 2020, 52(4): 607-609. |
| [12] | 刘欢,何映东,刘金波,黄薇,赵娜,赵红薇,周晓华,王宏宇. 血管健康指标对新发心脑血管事件的预测价值:北京血管健康分级标准的初步验证[J]. 北京大学学报(医学版), 2020, 52(3): 514-520. |
| [13] | 任川,吴晓月,赵威,陶立元,刘萍,高炜. 心肺适能对动脉粥样硬化性心血管疾病高危患者的保护作用[J]. 北京大学学报(医学版), 2020, 52(1): 152-157. |
| [14] | 段丽萍,郑朝霞,张宇慧,董捷. 腹膜透析患者营养不良-炎症-心血管疾病与认知功能恶化的关系[J]. 北京大学学报(医学版), 2019, 51(3): 510-518. |
| [15] | 司亚琴,唐迅,张杜丹,何柳,曹洋,王晋伟,李娜,刘建江,高培,胡永华. 北方农村人群心血管病一级预防筛查策略的评价[J]. 北京大学学报(医学版), 2018, 50(3): 443-449. |
|
||