北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (4): 723-727. doi: 10.19723/j.issn.1671-167X.2019.04.022
狼疮性肾炎患者足细胞损伤与肾组织巨噬细胞浸润的关系
- 青岛大学附属医院肾内科,山东青岛 266003
Relationship between podocyte injury and macrophage infiltration in renal tissues of patients with lupus nephritis
Ying WANG,Ming-hui LI,Yan ZHANG,Xiao-yan HU,Rui-xia MA( )
)
- Department of Nephrology, the Affiliated Hospital of Qingdao University, Qingdao 266003, Shandong, China
摘要:
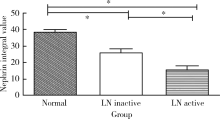
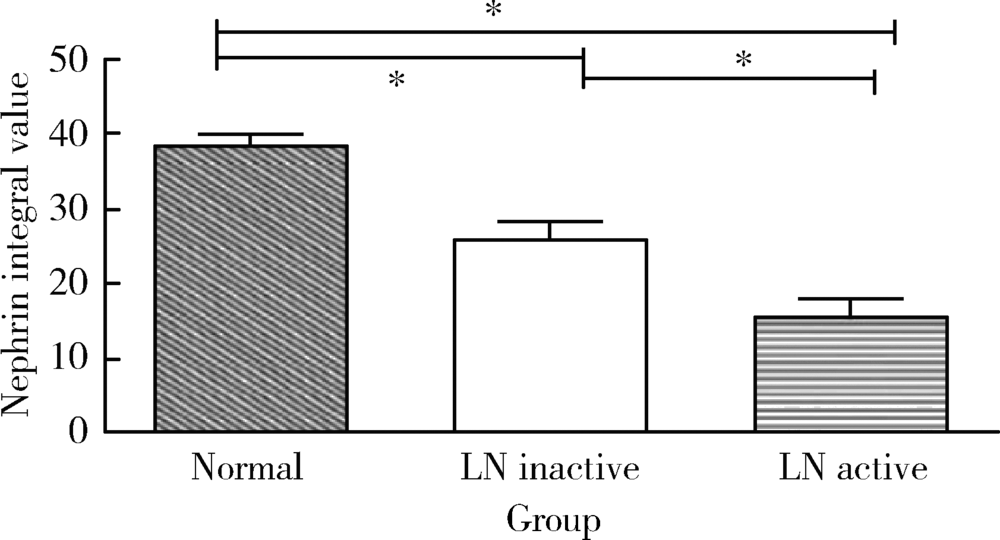
目的:探讨狼疮性肾炎(lupus nephritis, LN)患者足细胞损伤与肾组织巨噬细胞浸润的关系,探索LN足细胞损伤的潜在机制。方法:选择初次诊治经肾活检组织病理学检查确诊为LN的患者60例作为病例组,其中肾疾病活动指数≥4分的38例纳入活动组,另选择10例因肾外伤行肾切除患者的正常肾组织作为对照组。通过光学显微镜和电子显微镜观察肾组织及足细胞的损伤,通过免疫组化、免疫荧光等方法检测60例LN患者及10例正常对照组患者的肾组织中足细胞特异性蛋白nephrin的表达和巨噬细胞(CD68 +细胞)的浸润情况。多组间比较采用方差分析,组间两两比较采用LSD检验,两变量的相关性分析采用Pearson相关分析。 结果:(1)与正常对照组相比,LN患者nephrin表达显著减少,并且活动组LN患者肾nephrin的表达显著低于非活动组(P<0.05);(2)LN患者肾组织巨噬细胞明显多于正常对照组,主要分布在肾小球中,且活动组浸润的巨噬细胞数量多于非活动组(P<0.05);(3) LN患者肾组织中nephrin的表达与巨噬细胞的浸润呈负相关(r=0.761, P<0.001)。结论:LN肾组织中巨噬细胞浸润可能是狼疮肾炎足细胞损伤的重要机制之一。
中图分类号:
- R593.24 +2
| [1] | Maroz N, Segal MS . Lupus nephritis and end-stage kidney disease[J]. Am J Med Sci, 2013,346(4):319-323. |
| [2] | Schiffer L, Bethunaickan R, Ramanujam M , et al. Activated renal macrophages are markers of disease onset and disease remission in lupus nephritis.[J]. J Immunol, 2008,180(3):1938-1947. |
| [3] | Koop K, Eikmans M , Baelde HJ, et a1. Expression of podocyte-associated molecules in acquired human kidney diseases[J]. J Am Soc Nephrol, 2003,14(8):2063-2071. |
| [4] | Desai N, Cimbaluk D , Lewis EJ, et a1. Proteinuria in membranous lupus nephritis: the pathology is in the podocyte[J]. Lupus, 2013,22(5):461-468. |
| [5] | 郭银凤, 赵宇, 姜彧滕 , 等. 巨噬细胞诱导糖尿病肾病足细胞凋亡及其机制[J]. 中华内分泌代谢杂志, 2017,33(8):680-686. |
| [6] | You H, Gao T, Cooper TK , et al. Macrophages directly mediate diabetic renal injury[J]. Am J Physiol Renal Physiol, 2013,305(12):F1719-F1727. |
| [7] | Hochberg MC . Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus[J]. Arthritis Rheum, 1997,40(9):1725. |
| [8] | Higgins DF, Kimura K, Bernhardt WM , et al. Hypoxia promotes fibrogenesis in vivo via HIF-1 stimulation of epithelial-to-mesenchymal transition[J]. J Clin Invest, 2007,117(12):3810-3820. |
| [9] | Mok CC. Biomarkers for lupus nephritis: a critical appraisal [J/OL]. J Biomed Biotechnol, 2010, 2010: 638413. ( 010-04-19) [2018-08-04]. . |
| [10] | Reyes-Thomas J, Blanco I, Putterman C . Urinary biomarkers in lupus nephritis[J]. Clin Rev Allergy Immunol, 2011,40(3):138-150. |
| [11] | 刘文静, 杜玄一 . 肾脏疾病足细胞保护机制研究进展[J]. 中国中西医结合肾病杂志, 2015,16(12):1112-1114. |
| [12] | Hanamura K, Tojo A, Fujita T . Urinary and glomerular podocytes in patients with chronic kidney diseases[J]. Clin Exp Nephrol, 2014,18(1):95-103. |
| [13] | 马瑞霞, 刘楠楠, 李作林 , 等. 白细胞介素-18与狼疮肾炎患者足细胞损伤关系的研究[J]. 中华风湿病学杂志, 2016,20(1):28-33. |
| [14] | 马瑞霞, 周海燕, 孙益婷 , 等. 狼疮肾炎患者肾组织淋巴细胞浸润与足细胞损伤关系的研究[J]. 中华风湿病学杂志, 2015,19(12):824-828. |
| [15] | 姜亚丽, 王媛媛, 孙世仁 , 等. 巨噬细胞在肾脏疾病治疗中的研究新进展[J]. 国际泌尿系统杂志, 2015,35(3):468-470. |
| [16] | Meng XM, Wang S, Huang XR , et al. Inflammatory macrophages can transdifferentiate into myofibroblasts during renal fibrosis[J]. Cell Death Dis, 2016,7(12):e2495. |
| [17] | Yung S, Yap DY , Chan TM. Recent advances in the understanding of renal inflammation and fibrosis in lupus nephritis [J/OL]. F1000 Res, 2017, 6 (F1000 Faculty Rev): 874. ( 2017-06-13) [2018-08-04]. . |
| [18] | Guo YF, Song ZX, Zhou M , et al. Infiltrating macrophages in diabetic nephropathy promote podocytes apoptosis via TNF-α-ROS- p38MAPK pathway[J]. Oncotarget, 2017,8(32):53276-53287. |
| [1] | 罗芷筠,吴佳佳,宋优,梅春丽,杜戎. 伴神经精神系统病变的系统性红斑狼疮相关巨噬细胞活化综合征2例[J]. 北京大学学报(医学版), 2023, 55(6): 1111-1117. |
| [2] | 姚海红,杨帆,唐素玫,张霞,何菁,贾园. 系统性红斑狼疮及成人Still病合并巨噬细胞活化综合征的临床特点及诊断指标[J]. 北京大学学报(医学版), 2023, 55(6): 966-974. |
| [3] | 邢晓燕,张筠肖,朱冯赟智,王一帆,周新尧,李玉慧. 皮肌炎合并巨噬细胞活化综合征5例[J]. 北京大学学报(医学版), 2022, 54(6): 1214-1218. |
| [4] | 贾园,栗占国. 成人巨噬细胞活化综合征诊断困境和个体化治疗[J]. 北京大学学报(医学版), 2020, 52(6): 991-994. |
| [5] | 陈颖怡,胡紫琪,惠甜倩,刘鹤. Zeste同源蛋白2增强子通过调节巨噬细胞趋化影响牙髓炎症反应[J]. 北京大学学报(医学版), 2020, 52(1): 18-23. |
| [6] | 姚海红,王旖旎,张霞,赵金霞,贾园,王昭,栗占国. 67例成人巨噬细胞活化综合征的临床特征及治疗转归[J]. 北京大学学报(医学版), 2019, 51(6): 996-1002. |
| [7] | 赵彦瑞,刘洋,王东,吕文睿,周君琳. 二氧化硫对大鼠肢体缺血再灌注致急性肺损伤中肺泡巨噬细胞凋亡的影响[J]. 北京大学学报(医学版), 2019, 51(2): 239-244. |
| [8] | 刘爽,郭雨龙,杨静逸,王维,徐健. 间充质干细胞治疗系统性红斑狼疮有效性的meta分析[J]. 北京大学学报(医学版), 2018, 50(6): 1014-1021. |
| [9] | 高翔,陈香梅,张婷,张静,陈茉,郭正阳,石岩岩,鲁凤民,丁士刚. 巨噬细胞加帽蛋白与胃癌细胞增殖及迁移能力的关系[J]. 北京大学学报(医学版), 2017, 49(3): 489-494. |
| [10] | 赵曼曼, 张巧丽, 闫辉, 杜军保, 耿彬, 唐朝枢, 金红芳. H2S对氧化型低密度脂蛋白诱导人单核巨噬细胞核转录因子-κB的影响及机制[J]. 北京大学学报(医学版), 2013, 45(2): 192-. |
| [11] | 张效云, 李蓟龙, 董明纲, 高丽芬, 钟光明. 白介素-17 在沙眼衣原体呼吸道感染中的早期产生可提高局部白介素-6和巨噬细胞炎性蛋白-2的表达[J]. 北京大学学报(医学版), 2010, 42(5): 509-513. |
| [12] | 沈臻霖, 聂海瑜, 王海芳, 杨彬, 钟丽君, 邹霞娟, 娄雅欣, 刘丹, 郭健, 贾光. 表面不同修饰的两种多壁碳纳米管引起RAW264.7细胞蛋白质差异表达[J]. 北京大学学报(医学版), 2010, 42(3): 345-350. |
| [13] | 刘淑芳, 丁洁, 范青锋, 张涵. 嘌呤霉素致足细胞损伤细胞模型的建立[J]. 北京大学学报(医学版), 2008, 40(6): 586-589. |
| [14] | 李百花, 张秋香, 董殿军, 林晓明. 番茄红素对急性肺损伤大鼠免疫细胞和炎性细胞因子的影响[J]. 北京大学学报(医学版), 2007, 39(1): 77-82. |
| [15] | 李永强, 肖跃飞, 黄海长, 李惊子, 袁维中. 高糖对足细胞表达结缔组织生长因子及其受体蛋白的调节[J]. 北京大学学报(医学版), 2006, 38(3): 262-265. |
|
||