北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (6): 1214-1218. doi: 10.19723/j.issn.1671-167X.2022.06.026
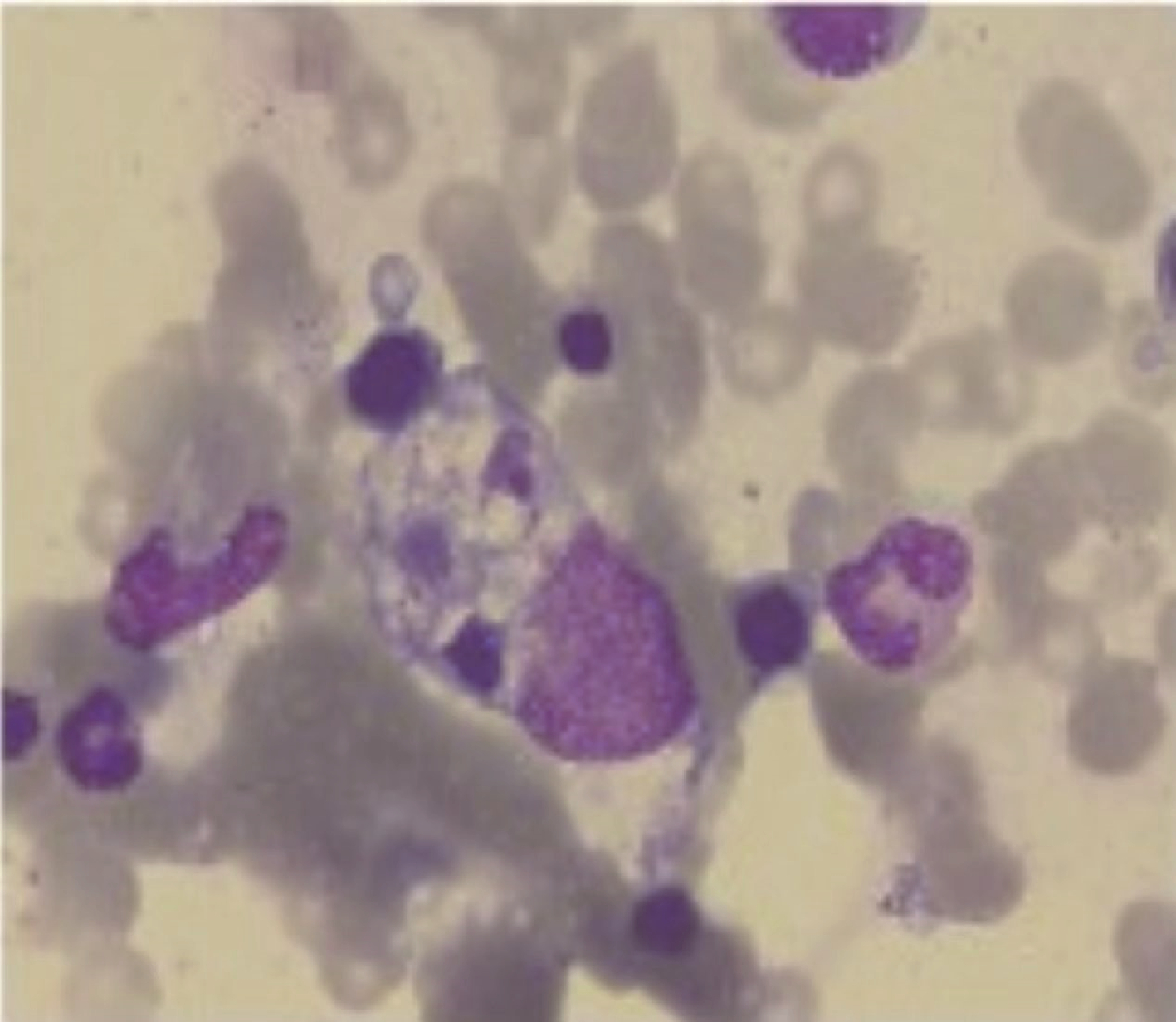
皮肌炎合并巨噬细胞活化综合征5例
邢晓燕1,张筠肖2,朱冯赟智1,王一帆1,周新尧3,李玉慧1,*( )
)
- 1. 北京大学人民医院风湿免疫科,北京 100044
2. 北京市监狱管理局清河分局医院内科,天津 300481
3. 中国中医科学院广安门医院风湿病科,北京 100053
Clinical analysis of 5 cases of dermatomyositis complicated with macrophage activation syndrome
Xiao-yan XING1,Jun-xiao ZHANG2,Feng-yun-zhi ZHU1,Yi-fan WANG1,Xin-yao ZHOU3,Yu-hui LI1,*( )
)
- 1. Department of Rheumatology and Immunology, Peking University People' s Hospital, Beijing 100044, China
2. Department of Internal Medicine, Beijing Prison Administration Qinghe Branch, Tianjin 300481, China
3. Department of Rheumatology and Immunology, Guang' anmen Hospital of China Academy of Chinese Medical Sciences, Beijing 100053, China
中图分类号:
- R593.26
| 1 |
Bohan A , Peter JB . Polymyositis and dermatomyositis (first of two parts)[J]. N Engl J Med, 1975, 292 (7): 344- 347.
doi: 10.1056/NEJM197502132920706 |
| 2 |
Lundberg IE , Tjarnlund A , Bottai M , et al. 2017 European League Against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups[J]. Ann Rheum Dis, 2017, 76 (12): 1955- 1964.
doi: 10.1136/annrheumdis-2017-211468 |
| 3 |
Henter JI , Horne A , Arico M , et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis[J]. Pediatr Blood Cancer, 2007, 48 (2): 124- 131.
doi: 10.1002/pbc.21039 |
| 4 |
Lerkvaleekul B , Vilaiyuk S . Macrophage activation syndrome: Early diagnosis is key[J]. Open Access Rheumatol, 2018, 10, 117- 128.
doi: 10.2147/OARRR.S151013 |
| 5 |
Kumakura S , Murakawa Y . Clinical characteristics and treatment outcomes of autoimmune-associated hemophagocytic syndrome in adults[J]. Arthritis Rheumatol, 2014, 66 (8): 2297- 2307.
doi: 10.1002/art.38672 |
| 6 |
Liang J , Xu D , Sun C , et al. Hemophagocytic lymphohistiocytosis: Prevalence, risk factors, outcome, and outcome-related factors in adult idiopathic inflammatory myopathies[J]. J Rheumatol, 2020, 47 (10): 1532- 1540.
doi: 10.3899/jrheum.190542 |
| 7 |
Minoia F , Davi S , Horne A , et al. Clinical features, treatment, and outcome of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: A multinational, multicenter study of 362 patients[J]. Arthritis Rheumatol, 2014, 66 (11): 3160- 3169.
doi: 10.1002/art.38802 |
| 8 |
Tang S , Li S , Zheng S , et al. Understanding of cytokines and targeted therapy in macrophage activation syndrome[J]. Semin Arthritis Rheum, 2021, 51 (1): 198- 210.
doi: 10.1016/j.semarthrit.2020.12.007 |
| 9 |
Kostik MM , Dubko MF , Masalova VV , et al. Identification of the best cutoff points and clinical signs specific for early recognition of macrophage activation syndrome in active systemic juvenile idiopathic arthritis[J]. Semin Arthritis Rheum, 2015, 44 (4): 417- 422.
doi: 10.1016/j.semarthrit.2014.09.004 |
| 10 |
Fardet L , Galicier L , Lambotte O , et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome[J]. Arthritis Rheumatol, 2014, 66 (9): 2613- 2620.
doi: 10.1002/art.38690 |
| 11 |
Schulert GS . The storm beneath the storm: MAS-HLH in inflammatory myopathies[J]. J Rheumatol, 2020, 47 (10): 1461- 1463.
doi: 10.3899/jrheum.191274 |
| 12 |
Gono T , Kawaguchi Y , Ozeki E , et al. Serum ferritin correlates with activity of anti-MDA5 antibody-associated acute interstitial lung disease as a complication of dermatomyositis[J]. Mod Rheumatol, 2011, 21 (2): 223- 227.
doi: 10.3109/s10165-010-0371-x |
| 13 |
La Rosee P , Horne A , Hines M , et al. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults[J]. Blood, 2019, 133 (23): 2465- 2477.
doi: 10.1182/blood.2018894618 |
| 14 |
Canna SW , Girard C , Malle L , et al. Life-threatening NLRC4-associated hyperinflammation successfully treated with IL-18 inhibition[J]. J Allergy Clin Immunol, 2017, 139 (5): 1698- 1701.
doi: 10.1016/j.jaci.2016.10.022 |
| 15 |
Gabr JB , Liu E , Mian S , et al. Successful treatment of secondary macrophage activation syndrome with emapalumab in a patient with newly diagnosed adult-onset Still's disease: Case report and review of the literature[J]. Ann Transl Med, 2020, 8 (14): 887.
doi: 10.21037/atm-20-3127 |
| 16 |
Ahmed A , Merrill SA , Alsawah F , et al. Ruxolitinib in adult patients with secondary haemophagocytic lymphohistiocytosis: An open-label, single-centre, pilot trial[J]. Lancet Haematol, 2019, 6 (12): e630- e637.
doi: 10.1016/S2352-3026(19)30156-5 |
| 17 |
Verweyen E , Holzinger D , Weinhage T , et al. Synergistic signaling of TLR and IFNalpha/beta facilitates escape of IL-18 expression from endotoxin tolerance[J]. Am J Respir Crit Care Med, 2020, 201 (5): 526- 539.
doi: 10.1164/rccm.201903-0659OC |
| 18 | Wu J, Sun L, Tang X, et al. Effective therapy of tocilizumab on systemic juvenile idiopathic arthritis associated refractory macrophage activation syndrome[J]. Mod Rheumatol, 2021[2022-08-01]. https://doi.org/10.1093/mr/roab119. |
| 19 |
Fujita Y , Fukui S , Suzuki T , et al. Anti-MDA5 antibody-positive dermatomyositis complicated by autoimmune-associated hemophagocytic syndrome that was successfully treated with immunosuppressive therapy and plasmapheresis[J]. Intern Med, 2018, 57 (23): 3473- 3478.
doi: 10.2169/internalmedicine.1121-18 |
| 20 |
Kaieda S , Yoshida N , Yamashita F , et al. Successful treatment of macrophage activation syndrome in a patient with dermatomyositis by combination with immunosuppressive therapy and plasmapheresis[J]. Mod Rheumatol, 2015, 25 (6): 962- 966.
doi: 10.3109/14397595.2013.844402 |
| 21 |
Komiya Y , Saito T , Mizoguchi F , et al. Hemophagocytic syndrome complicated with dermatomyositis controlled successfully with infliximab and conventional therapies[J]. Intern Med, 2017, 56 (23): 3237- 3241.
doi: 10.2169/internalmedicine.7966-16 |
| 22 |
Sasaki H , Kohsaka H . Current diagnosis and treatment of polymyositis and dermatomyositis[J]. Mod Rheumatol, 2018, 28 (6): 913- 921.
doi: 10.1080/14397595.2018.1467257 |
| 23 |
Gavand PE , Serio I , Arnaud L , et al. Clinical spectrum and therapeutic management of systemic lupus erythematosus-associated macrophage activation syndrome: A study of 103 episodes in 89 adult patients[J]. Autoimmun Rev, 2017, 16 (7): 743- 749.
doi: 10.1016/j.autrev.2017.05.010 |
| [1] | 欧俊永,倪坤明,马潞林,王国良,颜野,杨斌,李庚午,宋昊东,陆敏,叶剑飞,张树栋. 肌层浸润性膀胱癌合并中高危前列腺癌患者的预后因素[J]. 北京大学学报(医学版), 2024, 56(4): 582-588. |
| [2] | 刘帅,刘磊,刘茁,张帆,马潞林,田晓军,侯小飞,王国良,赵磊,张树栋. 伴静脉癌栓的肾上腺皮质癌的临床治疗及预后[J]. 北京大学学报(医学版), 2024, 56(4): 624-630. |
| [3] | 虞乐,邓绍晖,张帆,颜野,叶剑飞,张树栋. 具有低度恶性潜能的多房囊性肾肿瘤的临床病理特征及预后[J]. 北京大学学报(医学版), 2024, 56(4): 661-666. |
| [4] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [5] | 方杨毅,李强,黄志高,陆敏,洪锴,张树栋. 睾丸鞘膜高分化乳头状间皮肿瘤1例[J]. 北京大学学报(医学版), 2024, 56(4): 741-744. |
| [6] | 乔佳佳,田聪,黄晓波,刘军. 肾结石合并系统性红斑狼疮行经皮肾镜碎石取石术的安全性和有效性评估[J]. 北京大学学报(医学版), 2024, 56(4): 745-749. |
| [7] | 曾媛媛,谢云,陈道南,王瑞兰. 脓毒症患者发生正常甲状腺性病态综合征的相关因素[J]. 北京大学学报(医学版), 2024, 56(3): 526-532. |
| [8] | 朱金荣,赵亚娜,黄巍,赵微微,王悦,王松,苏春燕. 感染新型冠状病毒的血液透析患者的临床特征[J]. 北京大学学报(医学版), 2024, 56(2): 267-272. |
| [9] | 刘鑫,石雪迎,李军. 新型冠状病毒感染相关缺血性结肠炎1例[J]. 北京大学学报(医学版), 2024, 56(2): 362-365. |
| [10] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [11] | 李建斌,吕梦娜,池强,彭一琳,刘鹏程,吴锐. 干燥综合征患者发生重症新型冠状病毒肺炎的早期预测[J]. 北京大学学报(医学版), 2023, 55(6): 1007-1012. |
| [12] | 罗芷筠,吴佳佳,宋优,梅春丽,杜戎. 伴神经精神系统病变的系统性红斑狼疮相关巨噬细胞活化综合征2例[J]. 北京大学学报(医学版), 2023, 55(6): 1111-1117. |
| [13] | 王丽芳,石连杰,宁武,高乃姝,王宽婷. 干燥综合征合并冷凝集素病1例[J]. 北京大学学报(医学版), 2023, 55(6): 1130-1134. |
| [14] | 张陈光,陈旭岩,吴圣,冯莉莉,王琰,陈妤,段敏,王科,宋琳琳. 咽旁脓肿致颈内动脉假性动脉瘤1例[J]. 北京大学学报(医学版), 2023, 55(6): 1135-1138. |
| [15] | 姚海红,杨帆,唐素玫,张霞,何菁,贾园. 系统性红斑狼疮及成人Still病合并巨噬细胞活化综合征的临床特点及诊断指标[J]. 北京大学学报(医学版), 2023, 55(6): 966-974. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 337
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 462
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||