北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (5): 868-873. doi: 10.19723/j.issn.1671-167X.2024.05.018
前交叉韧带重建术后侧切动作的生物力学特征
任爽, 时会娟, 梁子轩, 张思, 胡晓青, 黄红拾*( ), 敖英芳*(
), 敖英芳*( )
)
- 北京大学第三医院运动医学科,北京大学运动医学研究所,运动医学关节伤病北京市重点实验室,运动创伤治疗技术与器械教育部工程研究中心,北京 100191
Biomechanics during cutting movement in individuals after anterior cruciate ligament reconstruction
Shuang REN, Huijuan SHI, Zixuan LIANG, Si ZHANG, Xiaoqing HU, Hongshi HUANG*( ), Yingfang AO*(
), Yingfang AO*( )
)
- Department of Sports Medicine, Peking University Third Hospital; Institute of Sports Medicine of Peking University; Beijing Key Laboratory of Sports Injuries; Engineering Research Center of Sports Trauma Treatment Technology and Devices, Ministry of Education, Beijing 100191, China
摘要:
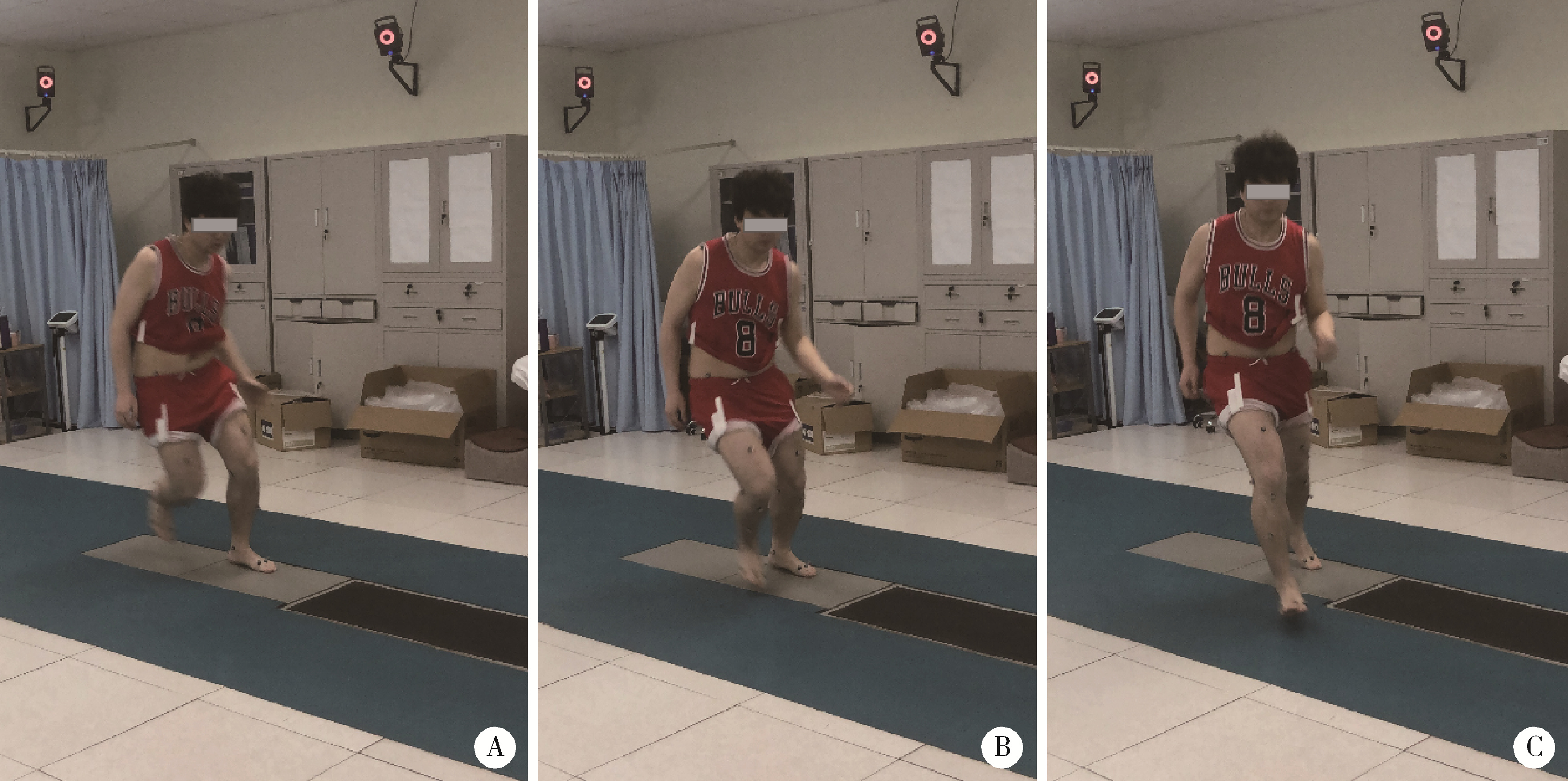
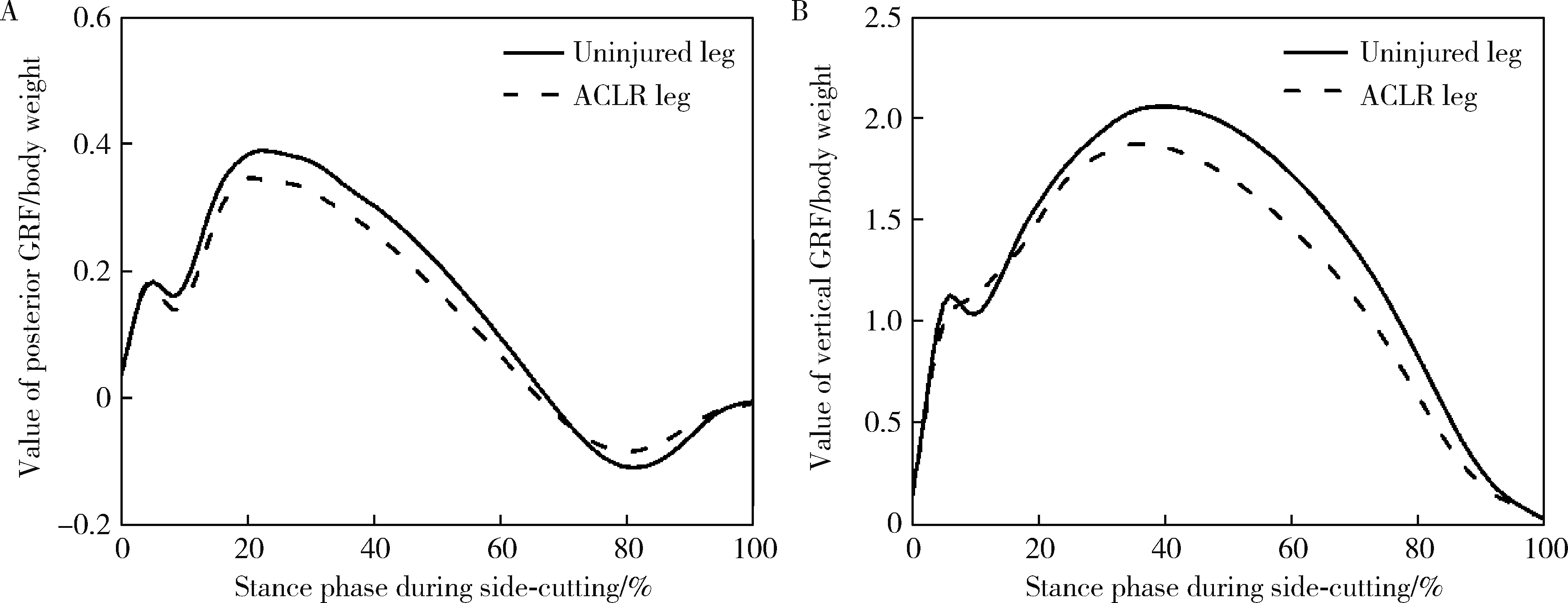
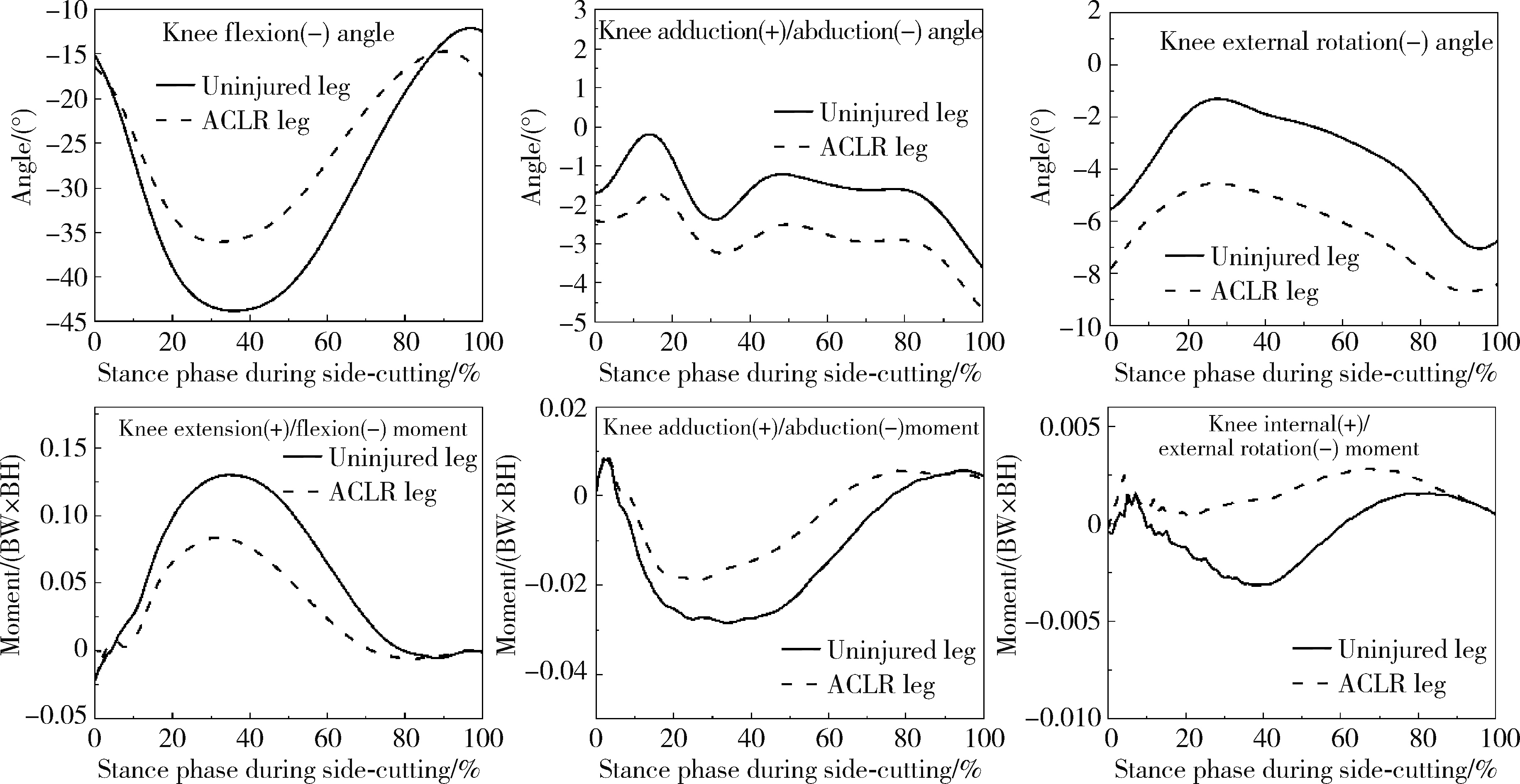
目的: 探究前交叉韧带(anterior cruciate ligament, ACL)重建术后12个月左右的患者在侧切动作过程中的生物力学特征,确定主要的异常生物力学特征及其机制。方法: 对16例ACL重建术后12个月左右的患者同步采集侧切动作过程中的运动学和动力学参数,计算膝关节的三维角度和三维力矩。应用配对t检验方法分析重建侧与未伤侧之间的生物力学特征差异。结果: 在侧切动作过程中,ACL重建侧的水平向后地面反作用力峰值(ACL重建侧0.380±0.071,未伤侧0.427±0.069,P = 0.003)和垂直向上地面反作用力峰值(ACL重建侧1.996±0.202,未伤侧2.110±0.182,P = 0.001)均显著小于未伤侧。与未伤侧相比,重建侧的膝关节屈曲角度较小(ACL重建侧38.3°±7.4°,未伤侧42.8°±7.9°,P < 0.001),而外旋角度较大(ACL重建侧10.3°±2.4°,未伤侧7.7°±2.1°, P=0.008)。ACL重建侧的膝关节伸展力矩峰值(ACL重建侧0.092±0.031,未伤侧0.133±0.024,P < 0.001)和外旋力矩峰值(ACL重建侧0.005±0.004,未伤侧0.008±0.004,P=0.015)均显著小于未伤侧。结论: 在侧切动作过程中,ACL重建患者膝关节运动主要在矢状面和水平面内呈现不对称特征,重建侧呈现较小的屈膝角度、膝关节伸展力矩和外旋力矩和较大的膝关节外旋角度。
中图分类号:
- R686.5
| 1 |
Ardern CL , Taylor NF , Feller JA , et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors[J]. Br J Sports Med, 2014, 48 (21): 1543- 1552.
doi: 10.1136/bjsports-2013-093398 |
| 2 |
Wiggins AJ , Grandhi RK , Schneider DK , et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis[J]. Am J Sports Med, 2016, 44 (7): 1861- 1876.
doi: 10.1177/0363546515621554 |
| 3 |
Johnston JT , Mandelbaum BR , Schub D , et al. Video analysis of anterior cruciate ligament tears in professional american football athletes[J]. Am J Sports Med, 2018, 46 (4): 862- 868.
doi: 10.1177/0363546518756328 |
| 4 | Kobayashi H , Kanamura T , Koshida S , et al. Mechanisms of the anterior cruciate ligament injury in sports activities: A twenty-year clinical research of 1 700 athletes[J]. J Sports Sci Med, 2010, 9 (4): 669- 675. |
| 5 |
Yang C , Yao W , Garrett WE , et al. Effects of an intervention program on lower extremity biomechanics in stop-jump and side-cutting tasks[J]. Am J Sports Med, 2018, 46 (12): 3014- 3022.
doi: 10.1177/0363546518793393 |
| 6 |
Arundale AJH , Silvers-Granelli HJ , Marmon A , et al. Changes in biomechanical knee injury risk factors across two collegiate soccer seasons using the 11+ prevention program[J]. Scand J Med Sci Sports, 2018, 28 (12): 2592- 2603.
doi: 10.1111/sms.13278 |
| 7 |
Dai B , Garrett WE , Gross MT , et al. The effects of 2 landing techniques on knee kinematics, kinetics, and performance during stop-jump and side-cutting tasks[J]. Am J Sports Med, 2015, 43 (2): 466- 474.
doi: 10.1177/0363546514555322 |
| 8 |
Hughes G , Musco P , Caine S , et al. Lower limb asymmetry after anterior cruciate ligament reconstruction in adolescent athletes: A systematic review and meta-analysis[J]. J Athl Train, 2020, 55 (8): 811- 825.
doi: 10.4085/1062-6050-0244-19 |
| 9 |
Sharafoddin-Shirazi F , Letafatkar A , Hogg J , et al. Biomechanical asymmetries persist after ACL reconstruction: Results of a 2-year study[J]. J Exp Orthop, 2020, 7 (1): 86.
doi: 10.1186/s40634-020-00301-2 |
| 10 | 李翰君, 刘卉, 张美珍, 等. 确定前交叉韧带损伤概率及危险因素的随机生物力学模型与模拟[J]. 体育科学, 2014, 34 (12): 37- 43. |
| 11 |
Burland JP , Toonstra JL , Howard JS . Psychosocial barriers after anterior cruciate ligament reconstruction: A clinical review of factors influencing postoperative success[J]. Sports Health, 2019, 11 (6): 528- 534.
doi: 10.1177/1941738119869333 |
| 12 | Gokeler A , Hof AL , Arnold MP , et al. Abnormal landing strategies after ACL reconstruction[J]. Scand J Med Sci Sports, 2010, 20 (1): e12- e19. |
| 13 |
Dai B , Butler RJ , Garrett WE , et al. Anterior cruciate ligament reconstruction in adolescent patients: Limb asymmetry and functional knee bracing[J]. Am J Sports Med, 2012, 40 (12): 2756- 2763.
doi: 10.1177/0363546512460837 |
| 14 |
Nunley RM , Wright D , Renner JB , et al. Gender comparison of patellar tendon tibial shaft angle with weight bearing[J]. Res Sports Med, 2003, 11 (3): 173- 185.
doi: 10.1080/15438620390231193 |
| 15 |
Yu B , Lin CF , Garrett WE . Lower extremity biomechanics during the landing of a stop-jump task[J]. Clin Biomech (Bristol, Avon), 2006, 21 (3): 297- 305.
doi: 10.1016/j.clinbiomech.2005.11.003 |
| 16 |
Li G , Papannagari R , de Frate LE , et al. Comparison of the ACL and ACL graft forces before and after ACL reconstruction: An in vitro robotic investigation[J]. Acta Orthop, 2006, 77 (2): 267- 274.
doi: 10.1080/17453670610046019 |
| 17 |
Woo SL , Hollis JM , Adams DJ , et al. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation[J]. Am J Sports Med, 1991, 19 (3): 217- 225.
doi: 10.1177/036354659101900303 |
| 18 |
Scanlan SF , Chaudhari AM , Dyrby CO , et al. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees[J]. J Biomech, 2010, 43 (9): 1817- 1822.
doi: 10.1016/j.jbiomech.2010.02.010 |
| 19 |
Pairot-de-Fontenay B , Willy RW , Elias ARC , et al. Running biomechanics in individuals with anterior cruciate ligament reconstruction: A systematic review[J]. Sports Med, 2019, 49 (9): 1411- 1424.
doi: 10.1007/s40279-019-01120-x |
| 20 | Karanikas K , Arampatzis A , Brüggemann GP . Motor task and muscle strength followed different adaptation patterns after anterior cruciate ligament reconstruction[J]. Eur J Phys Rehabil Med, 2009, 45 (1): 37- 45. |
| 21 |
Perraton LG , Hall M , Clark RA , et al. Poor knee function after ACL reconstruction is associated with attenuated landing force and knee flexion moment during running[J]. Knee Surg Sports Traumatol Arthrosc, 2018, 26 (2): 391- 398.
doi: 10.1007/s00167-017-4810-5 |
| 22 | Arhos EK , Capin JJ , Buchanan TS , et al. Quadriceps strength symmetry does not modify gait mechanics after anterior cruciate ligament reconstruction, rehabilitation, and return-to-sport training[J]. Am J Sports Med, 2020, 49 (2): 417- 425. |
| 23 |
King E , Richter C , Franklyn-Miller A , et al. Biomechanical but not timed performance asymmetries persist between limbs 9 months after ACL reconstruction during planned and unplanned change of direction[J]. J Biomech, 2018, 81, 93- 103.
doi: 10.1016/j.jbiomech.2018.09.021 |
| [1] | 王江静,魏顺依,敖英芳,杨渝平. 前交叉韧带重建术后三种不同药物镇痛早期疗效的对比[J]. 北京大学学报(医学版), 2024, 56(2): 293-298. |
| [2] | 赵菡,卫彦,张学慧,杨小平,蔡晴,宁成云,徐明明,刘雯雯,黄颖,何颖,郭亚茹,江圣杰,白云洋,吴宇佳,郭雨思,郑晓娜,李文静,邓旭亮. 口腔硬组织修复材料仿生设计制备和临床转化[J]. 北京大学学报(医学版), 2024, 56(1): 4-8. |
| [3] | 印钰,梅宇,王泽刚,宋首一,刘鹏飞,何鹏峰,武文杰,谢兴. 固定袢和可调节袢在粗骨道中的长度对股骨骨道增宽及膝关节功能的影响[J]. 北京大学学报(医学版), 2021, 53(5): 883-890. |
| [4] | 任爽,时会娟,张家豪,刘振龙,邵嘉艺,朱敬先,胡晓青,黄红拾,敖英芳. 前交叉韧带重建术后移植物应力的有限元分析[J]. 北京大学学报(医学版), 2021, 53(5): 865-870. |
| [5] | 蒋艳芳,王健,王永健,刘佳,裴殷,刘晓鹏,敖英芳,马勇. 前交叉韧带翻修重建术后中长期临床疗效及影响因素[J]. 北京大学学报(医学版), 2021, 53(5): 857-863. |
| [6] | 吴元,李晓丽,杨松霖,晏晓明,李海丽. 应用CorVis ST对圆锥角膜及亚临床期圆锥角膜生物力学特性的研究及判别标准分析[J]. 北京大学学报(医学版), 2019, 51(5): 881-886. |
| [7] | 吴超,王振宇,林国中,于涛,刘彬,司雨,张一博,李元超. 单侧半椎板及不同程度小关节切除术对羊颈椎生物力学的影响[J]. 北京大学学报(医学版), 2019, 51(4): 728-732. |
| [8] | 张家豪,任爽,邵嘉艺,牛星跃,胡晓青,敖英芳. 前交叉韧带生物力学止点重建的解剖学与有限元分析[J]. 北京大学学报(医学版), 2019, 51(3): 586-590. |
| [9] | 荣艳波,田光磊,陈山林. 深层桡尺远侧韧带对桡尺远侧关节稳定作用的生物力学研究[J]. 北京大学学报(医学版), 2017, 49(3): 518-521. |
| [10] | 刘海鹰,王捷夫,朱震奇. 融合与Topping-off术对腰椎影响的有限元分析[J]. 北京大学学报(医学版), 2013, 45(5): 723-727. |
| [11] | 郭阳,田光磊,姜保国,陈山林,韩娜. 舟骨骨折的螺钉居中固定:生物力学试验[J]. 北京大学学报(医学版), 2013, 45(5): 684-687. |
| [12] | 李智, 王新知, 高承志, IVO Krejci. 计算机辅助设计与制作一体化玻璃纤维桩核修复漏斗状根管的抗疲劳和抗折性能[J]. 北京大学学报(医学版), 2013, 45(1): 59-63. |
| [13] | 彭长亮*, 杨毅*, 孙馨, 郭卫. 高渗盐水灭活自体骨再植的动物实验[J]. 北京大学学报(医学版), 2012, 44(6): 950-953. |
| [14] | 张红芳 , 赵超勇, 范红松, 张晖 , 裴福兴, 王光林. 多孔钛修复兔桡骨骨缺损的组织学和力学研究[J]. 北京大学学报(医学版), 2011, 43(5): 724-729. |
| [15] | 李永舵, 刘书茂, 贾金生, 周君琳 . 后踝骨折内固定方法的选择:生物力学及临床应用研究[J]. 北京大学学报(医学版), 2011, 43(5): 718-723. |
|
||