北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (1): 182-186. doi: 10.19723/j.issn.1671-167X.2019.01.031
计算机导航辅助下口内入路髁突切除术精确性分析
李明哲1,2,王晓霞1,△( ),李自力1,伊彪1,梁成1,何伟1
),李自力1,伊彪1,梁成1,何伟1
- 1. 北京大学口腔医学院·口腔医院,口腔颌面外科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室, 北京 100081
2. 国家儿童医学中心,首都医科大学附属北京儿童医院口腔科, 北京 100045
Accuracy analysis of computer assisted navigation for condylectomy via intraoral approach
Ming-zhe LI1,2,Xiao-xia WANG1,△( ),Zi-li LI1,Biao YI1,Cheng LIANG1,Wei HE1
),Zi-li LI1,Biao YI1,Cheng LIANG1,Wei HE1
- 1. Department of Oral and Maxilloficial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Department of Stomatology,Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing 100045, China
摘要:
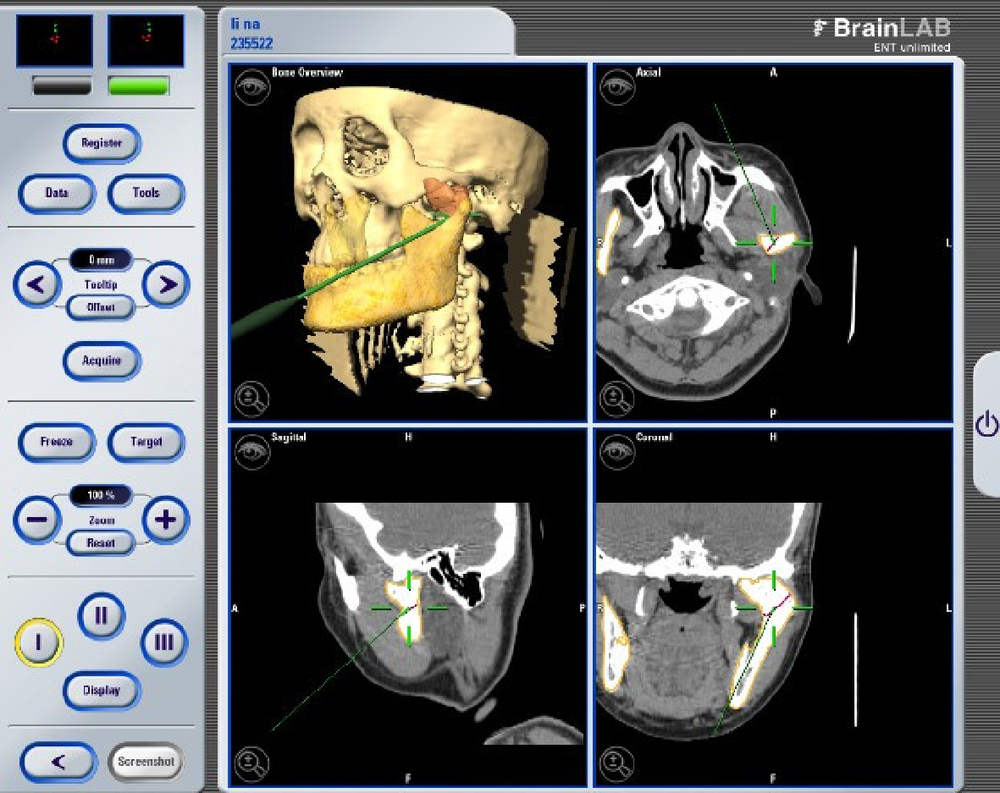
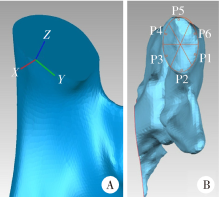
目的:在计算机导航辅助下,通过口内入路进行下颌骨髁突切除术,评估其术前设计方案在术中实现的精确性,并分析误差产生的部位和原因,为术式改良提供参考和思路。方法:收集2012年12月至2016年12月,在北京大学口腔医学院口腔颌面外科接受计算机导航辅助下口内入路髁突切除术的患者资料共23例。术前将患者螺旋CT数据导入ProPlan软件,将患侧下颌升支进行三维重建并根据病变范围设计髁突截骨线,生成术前设计模型,导入BrainLab导航系统,术中在计算机导航辅助下,采用口内入路,按术前设计截骨线完成髁突切除术。术后1周内拍摄颅颌面部螺旋CT,将术后患侧下颌升支进行三维重建,生成术后即刻模型,应用Geomagic软件将术前设计模型与术后即刻模型进行对齐,并在术后即刻模型的实际截骨面划分6个区域并定义相应区域测量点P1~P6,比较术前设计截骨面与术后实际截骨面在三维空间位置上的偏差,分析导航辅助手术实施的精确性。结果: 23例患者均顺利完成手术,获得满意疗效,术后CT复查病变完整切除,髁突截骨线与手术设计基本吻合。术后随访期内未见肿物复发及关节粘连。术后对髁突切除术实施精确性的验证分析显示,P1~P6共6组测量点所测得的偏差可信区间分别为(-2.26 mm,-1.89 mm),(-2.30 mm,-1.45 mm),(-3.37 mm,-2.91 mm),(-2.83 mm,-1.75 mm),(-1.13 mm, 0.99 mm),(-1.17 mm, 0.17 mm), 其中P3组与其他5组比较差异均有统计学意义,P5、P6组间差异无统计学意义而与其他4组差异有统计学意义。结论: 在计算机导航辅助下可以较精确地完成口内入路髁突切除术;截骨面各部位的手术偏差以过多切除为主,其中前内侧测量点所代表的髁突前内侧区域实际过多切除现象最明显,后侧、后外侧测量点所代表的髁突后外侧区域平均偏差不大,但偏差值的波动较其他4组大;计算机导航辅助下髁突切除术的精确性还有待提高。
中图分类号:
- R782.05
| [1] |
Luo E, Du W, Li J , et al. Guideline for the treatment of condylar osteochondroma combined with secondary dentofacial deformities[J]. J Craniofac Surg, 2016,27(5):1156-1161.
doi: 10.1097/SCS.0000000000002471 pmid: 27258707 |
| [2] |
Ord RA, Warburton G, Caccamese JF . Osteochondroma of the condyle: review of 8 cases[J]. Int J Oral Max Surg, 2010,39(6):523-528.
doi: 10.1016/j.ijom.2010.02.015 pmid: 20346630 |
| [3] |
Mehrotra D, Dhasmana S, Kamboj M , et al. Condylar hyperplasia and facial asymmetry: report of five cases[J]. J Maxillofac Oral Surg, 2011,10(1):50-56.
doi: 10.1007/s12663-010-0141-5 pmid: 3177497 |
| [4] |
Iizuka T, Schroth G, Laeng RH , et al. Osteochondroma of the mandibular condyle: report of a case.[J]. J Oral Maxillofac Surg, 1996,54(4):495-501.
doi: 10.1016/S0278-2391(96)90127-5 pmid: 8600267 |
| [5] |
Chen MJ, Yang C, Qiu YT , et al. Osteochondroma of the mandibular condyle: a classification system based on computed tomographic appearances[J]. J Craniofac Surg, 2014,25(5):1703-1706.
doi: 10.1097/SCS.0000000000000898 |
| [6] |
Wolford LM, Mehra P, Franco P . Use of conservative condylectomy for treatment of osteochondroma of the mandibular condyle[J]. J Oral Maxillofac Surg, 2002,60(3):262-268.
doi: 10.1053/joms.2002.30570 pmid: 11887135 |
| [7] |
Wolford LM, Mehra P, Reiche-Fischel O , et al. Efficacy of high condylectomy for management of condylar hyperplasia[J]. Am J Orthod Dentofacial Orthop, 2002,121(2):136-151.
doi: 10.1067/mod.2002.118403 pmid: 11840126 |
| [8] | 李自力, 王兴, 伊彪 , 等. 口腔内入路髁突切除术的临床应用研究[J]. 现代口腔医学杂志, 2008,22(4):341-344. |
| [9] |
Schoen R, Herklotz I, Metzger MC , et al. Endoscopic approach to removal of an osteochondroma of the mandibular condyle[J]. J Oral Maxillofac Surg, 2011,69(6):1657-1660.
doi: 10.1016/j.joms.2009.04.004 pmid: 20591549 |
| [10] |
王晓霞, 李自力, 伊彪 , 等. 计算机导航辅助下口内入路髁突切除术的临床应用[J]. 中华口腔医学杂志, 2013,48(6):350-354.
doi: 10.3760/cma.j.issn.1002-0098.2013.06.008 |
| [11] |
沈末伦, 余婧爽, 于洪波 . 导航及内镜技术联合正颌手术矫治髁突骨软骨瘤伴颌骨畸形数字化流程的建立和应用[J]. 中华口腔医学杂志, 2017,51(12):728-733.
doi: 10.3760/cma.j.issn.1002-0098.2016.12.006 |
| [12] |
Ewers R, Schicho K, Undt G , et al. Basic research and 12 years of clinical experience in computer-assisted navigation technology: a review[J]. Int J Oral Maxillofac Surg, 2005,34(1):1-8.
doi: 10.1016/j.ijom.2004.03.018 pmid: 15617960 |
| [13] | 赵泽亮, 沈国芳, 石慧敏 , 等. 髁突骨软骨瘤与髁突增生患者的CT表现特点分析[J]. 中国口腔颌面外科杂志, 2012,10(2):139-145. |
| [14] |
He Y, Zhang Y, An JG , et al. Zygomatic surface marker-assisted surgical navigation: a new computer-assisted navigation method for accurate treatment of delayed zygomatic fractures[J]. J Oral Ma-xillofac Surg, 2013,71(12):2101-2114.
doi: 10.1016/j.joms.2013.07.003 pmid: 24237774 |
| [15] |
Widmann G, Stoffner R, Bale R . Errors and error management in image-guided craniomaxillofacial surgery[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009,107(5):701-715.
doi: 10.1016/j.tripleo.2009.02.011 pmid: 19426922 |
| [16] |
Khadem R, Yeh CC, Sadeghi-Tehrani M , et al. Comparative tracking error analysis of five different optical tracking systems[J]. Comput Aided Surg, 2000,5(2):98-107.
doi: 10.3109/10929080009148876 pmid: 10862132 |
| [17] |
Luebbers HT, Messmer P, Obwegeser JA , et al. Comparison of different registration methods for surgical navigation in cranio-maxillofacial surgery[J]. J Craniomaxillofac Surg, 2008,36(2):109-116.
doi: 10.1016/j.jcms.2007.09.002 pmid: 18280173 |
| [18] |
Bell RB, Weimer KA, Dierks EJ , et al. Computer planning and intraoperative navigation for palatomaxillary and mandibular reconstruction with fibular free flaps.[J]. J Oral Maxillofac Surg, 2011,69(3):724.
doi: 10.1016/j.joms.2009.12.040 pmid: 20888108 |
| [1] | 李红光,韩玮华,吴训,冯继玲,李刚,孟娟红. 关节腔冲洗联合液态浓缩生长因子注射治疗单侧颞下颌关节骨关节炎的初步研究[J]. 北京大学学报(医学版), 2024, 56(2): 338-344. |
| [2] | 周境,刘怡. 不同垂直骨面型骨性Ⅱ类青少年女性颞下颌关节锥形束CT测量分析[J]. 北京大学学报(医学版), 2021, 53(1): 109-119. |
| [3] | 韩玮华,罗海燕,郭传瑸,宁琦,孟娟红. 软骨寡聚基质蛋白在颞下颌关节滑膜软骨瘤病中的表达[J]. 北京大学学报(医学版), 2021, 53(1): 34-39. |
| [4] | 陈硕,贺洋,安金刚,张益. 计算机辅助设计虚拟颌位在儿童颞下颌关节强直合并颌骨畸形同期矫治中的应用[J]. 北京大学学报(医学版), 2019, 51(5): 954-958. |
| [5] | 王丹丹,甘业华,马绪臣,孟娟红. ADAMTS14基因单核苷酸多态性与汉族女性颞下颌关节骨关节炎的相关性研究[J]. 北京大学学报(医学版), 2018, 50(2): 279-283. |
| [6] | 孟娟红,郭玉兴,罗海燕,郭传瑸,马绪臣. 颞下颌关节弥漫型腱鞘巨细胞瘤的诊断与治疗[J]. 北京大学学报(医学版), 2016, 48(6): 1049-1054. |
| [7] | 雷杰,刘木清,傅开元. 睡眠问题、焦虑及压力是颞下颌关节紊乱病肌筋膜疼痛发病的风险指标[J]. 北京大学学报(医学版), 2016, 48(4): 692-696. |
| [8] | 孟娟红,郭传瑸,马绪臣. 颞下颌关节腱鞘囊肿和滑膜囊肿的诊断与治疗[J]. 北京大学学报(医学版), 2014, 46(1): 43-47. |
| [9] | 王志辉, 姜岚, 赵燕平, 马绪臣. 青少年颞下颌关节骨关节病锥形束CT分析[J]. 北京大学学报(医学版), 2013, 45(2): 280-. |
| [10] | 孟娟红, 甘业华, 马绪臣. 颞下颌关节骨关节炎发病的分子机制及相关治疗的实验研究[J]. 北京大学学报(医学版), 2013, 45(1): 5-8. |
| [11] | 王霄, 张益, 李江明. 髁突矢状骨折继发颞下颌关节强直动物模型的建立[J]. 北京大学学报(医学版), 2011, 43(6): 903-907. |
| [12] | 曹烨, 李锴, 傅开元, 谢秋菲. 咬合干扰致大鼠咬肌组织蛋白基因产物及P物质表达变化[J]. 北京大学学报(医学版), 2010, 42(1): 50-55. |
| [13] | 张豪, 赵燕平, 韩科, 马绪臣. 稳定(牙合)垫治疗对颞下颌关节腔内压力的影响[J]. 北京大学学报(医学版), 2008, 40(1): 68-70. |
| [14] | 孙志鹏, 邹冰爽, 赵燕平, 马绪臣. 口腔正畸患者颞下颌关节骨关节病的临床分析[J]. 北京大学学报(医学版), 2008, 40(1): 47-51. |
| [15] | 王瑞永, 马绪臣, 张万林, 柳登高. 健康成年人颞下颌关节间隙锥形束计算机体层摄影术测量分析[J]. 北京大学学报(医学版), 2007, 39(5): 503-506. |
|
||