北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (2): 346-352. doi: 10.19723/j.issn.1671-167X.2020.02.024
引导性组织再生术对浓缩生长因子联合植骨术治疗下颌磨牙Ⅱ度根分叉病变临床效果的影响
- 北京大学口腔医学院·口腔医院,门诊部 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室, 北京 100034
Effect of concentrated growth factors combined with guided tissue regeneration in treatment of classⅡ furcation involvements of mandibular molars
Fei LI,Jing QIAO,Jin-yu DUAN,Yong ZHANG,Xiu-jing WANG( )
)
- First Clinical Division, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100034, China
摘要:
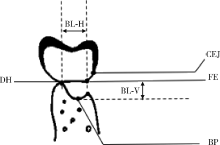
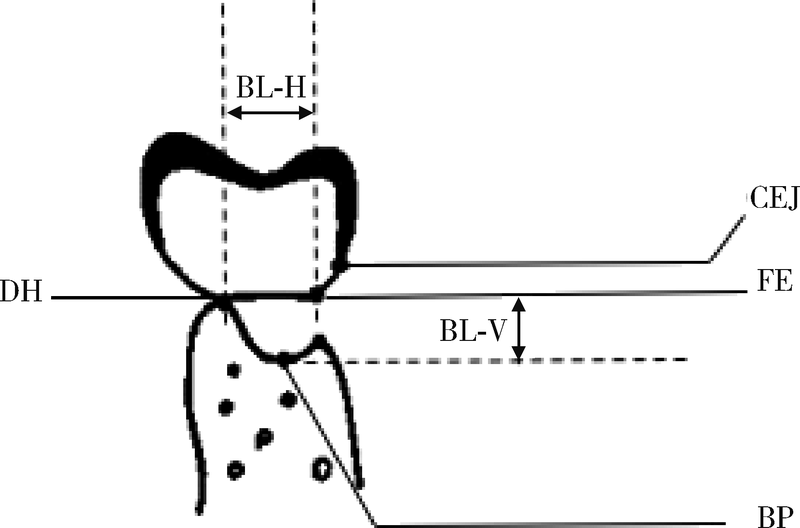
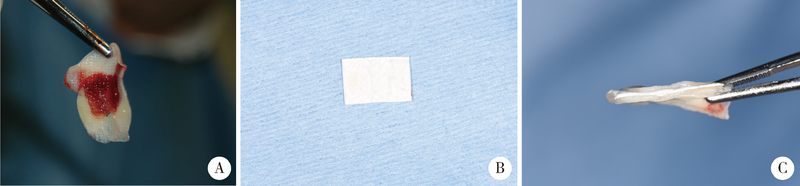
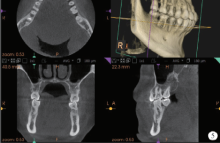
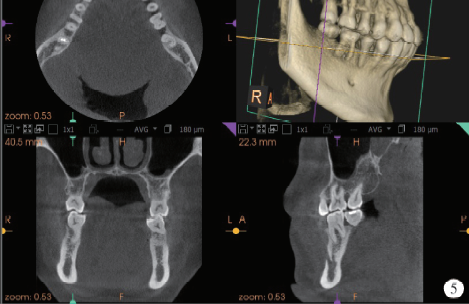
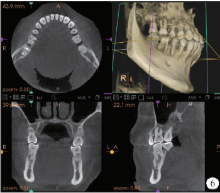
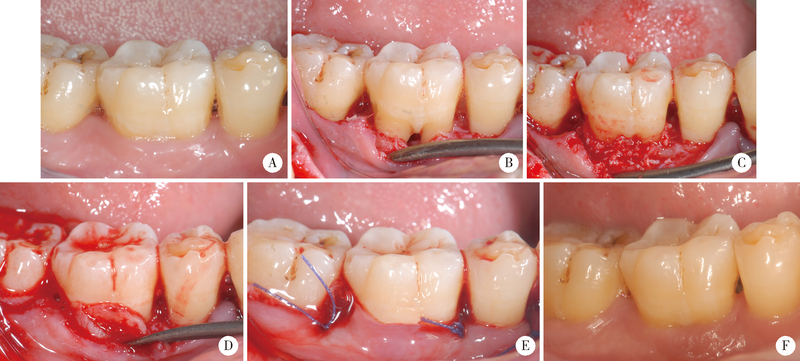
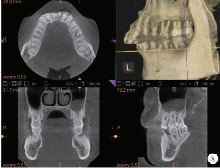
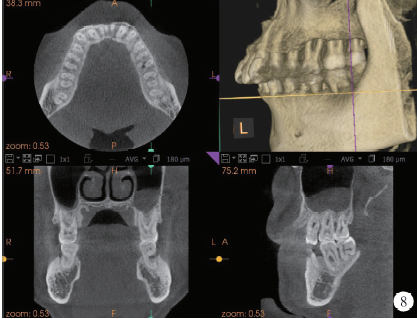
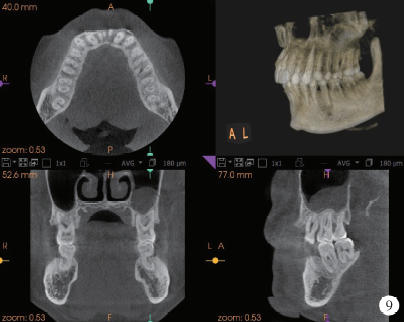
目的 评价引导性组织再生术(guided tissue regeneration, GTR)是否能够增进浓缩生长因子(concentrated growth factors, CGF)联合植骨术治疗下颌磨牙Ⅱ度根分叉病变的临床效果,以期为根分叉病变的再生寻求更好的治疗方法.方法: 纳入需进行牙周手术的35例下颌磨牙Ⅱ度根分叉病变患者,随机分为两组,试验组采用GTR+CGF+植骨术进行治疗,对照组采用CGF+植骨术进行治疗.在术前和术后1年时分别对患牙进行临床检查,并拍摄锥形束CT(cone beam computed tomography, CBCT).比较试验组和对照组手术前后临床和CBCT数据的变化.结果: 基线时两组的探诊深度,垂直附着丧失和水平附着丧失差异均无统计学意义(P>0.05).术后1年时,两组的临床指标较基线时均有显著改善(P<0.001),其中试验组的垂直附着获得和水平附着获得分别为(4.11±1.98) mm和(3.84±1.68) mm,改善程度显著高于对照组(P<0.001).基线时两组的CBCT显示的垂直骨丧失和水平骨丧失差异均无统计学意义(P>0.05).术后1年时,试验组的垂直骨缺损和水平骨缺损较基线时和对照组均有显著改善(P<0.001),分别减少(3.84±1.68) mm和(3.88±2.12) mm.结论: 下颌磨牙Ⅱ度根分叉病变患者观察1年的结果显示,GTR可以促进CGF+植骨术在下颌磨牙Ⅱ度根分叉病变中的治疗效果.
中图分类号:
- R781.3
| [1] | Janssen KM , Vissink A, de Smit MJ, et al.Lessons to be learned from periodontitis[J]. Curr Opin Rheumatol, 2013,25(2):241-247. |
| [2] | Trombelli L, Farina R . Clinical outcomes with bioactive agents alone or in combination with grafting or guided tissue regeneration[J]. J Clin Periodontol, 2008,35(8 Suppl):117-135. |
| [3] | Stoecklin-Wasmer C ,Rutjes AW,da Costa BR,et al.Absorbable collagen membranes for periodontal regeneration: a systematic review[J]. J Dent Res, 2013,92(9):773-781. |
| [4] | Susin C, Fiorini T, Lee J , et al. Wound healing following surgical and regenerative periodontal therapy[J]. Periodontol 2000, 2015,68(1):83-98. |
| [5] | Martin P . Wound healing--aiming for perfect skin regeneration[J]. Science, 1997,276(5309):75-81. |
| [6] | Giannobile WV, Finkelman RD, Lynch SE . Comparison of canine and non-human primate animal models for periodontal regenerative therapy: results following a single administration of PDGF/IGF-I[J]. J Periodontol, 1994,65(12):1158-1168. |
| [7] | Qiao J, An N, Ouyang X . Quantification of growth factors in different platelet concentrates[J]. Platelets, 2017,28(8):774-778. |
| [8] | Rodella LF, Favero G, Boninsegna R , et al. Growth factors, CD34 positive cells, and fibrin network analysis in concentrated growth factors fraction[J]. Microsc Res Tech, 2011,74(8):772-777. |
| [9] | 乔静, 段晋瑜, 褚祎 , 等. 浓缩生长因子在下颌磨牙Ⅱ度根分叉病变再生治疗中的应用[J]. 北京大学学报(医学版), 2017,49(1):36-42. |
| [10] | Hamp SE, Nyman S, Lindhe J . Periodontal treatment of multiroo-ted teeth. Results after 5 years[J]. J Clin Periodontol, 1975,2(3):126-135. |
| [11] | Qiao J, Duan J, Zhang Y , et al. The effect of concentrated growth factors in the treatment of periodontal intrabony defects [J].Future Sci OA, 2016, 2(4): FS136. |
| [12] | Pirpir C, Yilmaz O, Candirli C , et al. Evaluation of effectiveness of concentrated growth factor on osseointegration[J]. Int J Implant Dent, 2017,3(1):7. |
| [13] | Shyu SS, Fu E, Shen EC . Clinical and microcomputed topography evaluation of the concentrated growth factors as a sole material in a cystic bony defect in alveolar bone followed by dental implantation: a case report[J]. Implant Dent, 2016,25(5):707-714. |
| [14] | Masuki H, Okudera T, Watanebe T , et al. Growth factor and pro-inflammatory cytokine contents in platelet-rich plasma (PRP), plasma rich in growth factors (PRGF), advanced platelet-rich fibrin (A-PRF), and concentrated growth factors (CGF)[J]. Int J Implant Dent, 2016,2(1):19. |
| [15] | Sahin IO, Gokmenoglu C, Kara C . Effect of concentrated growth factor on osteoblast cell response[J]. J Stomatol Oral Maxillofac Surg, 2018,119(6):477-481. |
| [16] | Qin J, Wang L, Sun Y , et al. Concentrated growth factor increases Schwann cell proliferation and neurotrophic factor secretion and promotes functional nerve recovery in vivo[J]. Int J Mol Med, 2016,37(2):493-500. |
| [17] | Pontoriero R, Lindhe J, Nyman S , et al. Guided tissue regeneration in degree Ⅱ furcation-involved mandibular molars. A clinical study[J]. J Clin Periodontol, 1988,15(4):247-254. |
| [18] | Needleman I, Tucker R, Giedrys-Leeper E , et al. A systematic review of guided tissue regeneration for periodontai infrabony defects[J]. J Periodont Res, 2002,37(5):380-388. |
| [19] | Behring J, Junker R, Walboomers XF , et al. Toward guided tissue and bone regeneration: morphology, attachment, proliferation, and migration of cells cultured on collagen barrier membranes. A systematic review[J]. Odontology, 2008,96(1):1-11. |
| [20] | Felipe M, Andrade PF, Grisi MFM , et al. Comparison of two surgical procedures for use of the acellular dermal matrix graft in the treatment of gingival recession: a randomized controlled clinical study[J]. J Periodontol, 2007,78(7):1209-1217. |
| [21] | Pajnigara NG, Kolte AP, Kolte RA , et al. Volumetric assessment of regenerative efficacy of demineralized freeze-dried bone allograft with or without amnion membrane in grade Ⅱ furcation defects: a cone beam computed tomography study[J]. Int J Periodontics Restorative Dent, 2017,37(2):255-262. |
| [22] | Irokawa D, Takeuchi T, Noda K , et al. Clinical outcome of periodontal regenerative therapy using collagen membrane and deproteinized bovine bone mineral: a 2.5-year follow-up study[J]. BMC Res Notes, 2017,10(1):102. |
| [23] | Kini V, Nayak DG, Uppoor AS . A clinical evaluation of biphasic calcium phosphate alloplast with and without a flowable bioabsorbable guided tissue regeneration barrier in the treatment of mandi-bular molar class Ⅱ furcation defects[J]. J Contemp Dent Pract, 2016,17(2):143-148. |
| [24] | Bozkurt A, Apel C, Sellhaus B , et al. Differences in degradation behavior of two non-cross-linked collagen barrier membranes: an in vitro and in vivo study[J]. Clin Oral Implants Res, 2014,25(12):1403-1411. |
| [1] | 李红光,韩玮华,吴训,冯继玲,李刚,孟娟红. 关节腔冲洗联合液态浓缩生长因子注射治疗单侧颞下颌关节骨关节炎的初步研究[J]. 北京大学学报(医学版), 2024, 56(2): 338-344. |
| [2] | 王聪伟,高敏,于尧,章文博,彭歆. 游离腓骨瓣修复下颌骨缺损术后义齿修复的临床分析[J]. 北京大学学报(医学版), 2024, 56(1): 66-73. |
| [3] | 汪大伟,王华东,李利,尹欣,黄伟,郭继东,杨亚锋,刘义灏,郑扬. 自体下关节突骨块应用于骨质疏松患者腰椎椎间融合术的疗效分析[J]. 北京大学学报(医学版), 2023, 55(5): 899-909. |
| [4] | 李维婷,李蓬,朴牧子,张芳,邸杰. 不同备洞方法收集自体骨骨量[J]. 北京大学学报(医学版), 2020, 52(1): 103-106. |
| [5] | 李博文,吴唯伊,唐琳,张一,刘玉华. 改良猪小肠黏膜下层可吸收膜在兔下颌骨缺损早期愈合中的作用[J]. 北京大学学报(医学版), 2019, 51(5): 887-892. |
| [6] | 乔静,段晋瑜,褚祎,孙昌洲. 浓缩生长因子在下颌磨牙Ⅱ度根分叉病变再生治疗中的应用[J]. 北京大学学报(医学版), 2017, 49(1): 36-042. |
| [7] | 陈飞,潘韶霞,冯海兰. 转化生长因子β1和血管内皮生长因子在浓缩生长因子各层中的分布及含量特点[J]. 北京大学学报(医学版), 2016, 48(5): 860-865. |
| [8] | 郭阳, 李淳, 田光磊, 姜保国, 赵俊会, 田文, 陈山林, 王海华. 手部骨巨细胞瘤的诊断和手术治疗[J]. 北京大学学报(医学版), 2012, 44(6): 866-. |
| [9] | 张立, 冯向辉, 路瑞芳, 孟焕新. 骨诱导活性异种骨移植治疗牙周炎骨下袋的临床疗效评价[J]. 北京大学学报(医学版), 2012, 44(5): 797-800. |
| [10] | 裴征, 关振鹏, 张绍龙, 李云鹏, 张卓. 重度膝内翻伴骨缺损的全膝表面置换术中的自体骨移植治疗[J]. 北京大学学报(医学版), 2011, 43(5): 707-713. |
| [11] | 康军, 沙月琴, 欧阳翔英. 脱矿冻干骨粉与富血小板血浆联合治疗牙周骨下袋[J]. 北京大学学报(医学版), 2010, 42(1): 24-27. |
| [12] | 唐志辉, 吕宏, 曹梅霞, 吴敏节. 下颌骨半柱状骨块重建牙种植患者萎缩牙槽嵴的临床疗效[J]. 北京大学学报(医学版), 2010, 42(1): 94-97. |
|
||