北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (1): 170-176. doi: 10.19723/j.issn.1671-167X.2022.01.027
影响全膝关节置换术患者术前预期的患者因素
- 北京大学人民医院骨关节科,北京 100044
Patient factors influencing preoperative expectations of patients undergoing total knee arthroplasty
LI Zhi-chang,HOU Yun-fei,ZHOU Zhi-wei,JIANG Long,ZHANG Shu,LIN Jian-hao( )
)
- Institute of Arthritis, Peking University People’s Hospital, Beijing 100044, China
摘要:
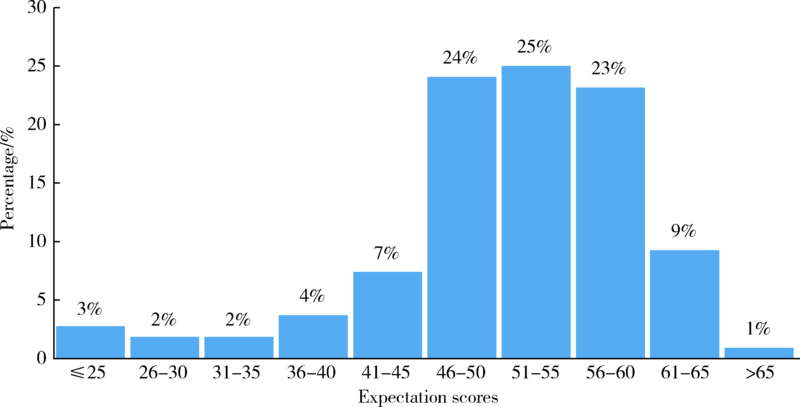
目的: 术前预期会影响关节置换术后患者的主观满意度及客观功能,调查患者对全膝关节置换术的预期情况,并分析其影响因素。方法: 收集108例单侧全膝关节置换术患者的人口学资料,以及术前的美国特种外科医院(Hospital for Special Surgery,HSS) 膝关节置换手术预期量表评分、30秒座椅站立测试、40米快速步行测试、12级爬楼梯测试、3米起立行走测试、6分钟步行测试、美国西部Ontario和McMaster大学(the Western Ontario and McMaster Universities,WOMAC)骨关节炎指数评分、膝关节学会评分 (Knee Society score,KSS)、健康调查简表(the MOS 36-item short-from health survey, SF-36)评分、视觉模拟评分(visual analogue scale, VAS)以及连续7天的每日步数。对各数据的观察值进行描述性报告,应用Pearson相关分析评估各参数间的相关性并进行多因素线性回归分析。结果: 患者的平均术前预期评分为58.98±5.44,其与患者的12级爬楼梯测试、3米起立行走测试、6分钟步行测试、KSS功能评分、SF-36的精神健康评分有弱相关性(相关系数0.1~0.3),与患者的每日平均步数,30秒座椅站立测试, 40米快速步行测试,KSS膝关节评分,WOMAC及其疼痛、僵直、功能三个评分,SF-36的生理功能、生理职能、躯体疼痛、活力及躯体健康评分有中度相关性(相关系数0.3~0.6)。多因素线性回归分析显示,仅有30秒座椅站立测试和SF-36量表中的生理职能、躯体疼痛及活力与患者对手术效果的预期评分有相关性(P<0.05)。结论: 术前疼痛更重、躯体功能更差、整体健康状况更低下的患者更迫切希望得到改善,医生要在术前与预期不现实的患者充分沟通。
中图分类号:
- R687.4
| [1] | Feng B, Zhu W, Bian YY, et al. China artificial joint annual data report[J]. Chin Med J (Engl), 2020, 134(6):752-753. |
| [2] |
Gunaratne R, Pratt DN, Banda J, et al. Patient dissatisfaction following total knee arthroplasty: A systematic review of the literature[J]. J Arthroplasty, 2017, 32(12):3854-3860.
doi: S0883-5403(17)30619-8 pmid: 28844632 |
| [3] |
Neuprez A, Delcour JP, Fatemi F, et al. Patients’ expectations impact their satisfaction following total hip or knee arthroplasty[J]. PLoS One, 2016, 11(12):e0167911.
doi: 10.1371/journal.pone.0167911 |
| [4] |
Hepinstall MS, Rutledge JR, Bornstein LJ, et al. Factors that impact expectations before total knee arthroplasty[J]. J Arthroplasty, 2011, 26(6):870-876.
doi: 10.1016/j.arth.2010.09.010 pmid: 21074356 |
| [5] |
Rief W, Shedden-Mora MC, Laferton JA, et al. Preoperative optimization of patient expectations improves long-term outcome in heart surgery patients: results of the randomized controlled PSY-HEART trial[J]. BMC Med, 2017, 15(1):4.
doi: 10.1186/s12916-016-0767-3 |
| [6] |
Hafkamp FJ, Lodder P, de Vries J, et al. Characterizing patients’ expectations in hip and knee osteoarthritis[J]. Qual Life Res, 2020, 29(6):1509-1519.
doi: 10.1007/s11136-019-02403-6 |
| [7] |
Ponzio DY, Chiu YF, Salvatore A, et al. An analysis of the influence of physical activity level on total knee arthroplasty expectations, satisfaction, and outcomes: Increased revision in active patients at five to ten years[J]. J Bone Joint Surg Am, 2018, 100(18):1539-1548.
doi: 10.2106/JBJS.17.00920 |
| [8] |
Mizner RL, Petterson SC, Clements KE, et al. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: A longitudinal analysis of outcomes[J]. J Arthroplasty, 2011, 26(5):728-737.
doi: 10.1016/j.arth.2010.06.004 pmid: 20851566 |
| [9] |
Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee[J]. J Rheumatol, 1988, 15(12):1833-1840.
pmid: 3068365 |
| [10] |
Symonds T, Hughes B, Liao S, et al. Validation of the Chinese Western Ontario and McMaster Universities Osteoarthritis Index in patients from Mainland China with osteoarthritis of the knee[J]. Arthritis Care Res (Hoboken), 2015, 67(11):1553-1560.
doi: 10.1002/acr.22631 pmid: 26018634 |
| [11] |
Xie F, Li SC, Goeree R, et al. Validation of Chinese Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) in patients scheduled for total knee replacement[J]. Qual Life Res, 2008, 17(4):595-601.
doi: 10.1007/s11136-008-9340-7 |
| [12] | Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society clinical rating system[J]. Clin Orthop Relat Res, 1989, 248:13-14. |
| [13] |
Scuderi GR, Bourne RB, Noble PC, et al. The new Knee Society knee scoring system[J]. Clin Orthop Relat Res, 2012, 470(1):3-19.
doi: 10.1007/s11999-011-2135-0 |
| [14] |
Dobson F, Hinman RS, Roos EM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis[J]. Osteoarthritis Cartilage, 2013, 21(8):1042-1052.
doi: 10.1016/j.joca.2013.05.002 |
| [15] |
Lyons EJ, Lewis ZH, Mayrsohn BG, et al. Behavior change techniques implemented in electronic lifestyle activity monitors: A systematic content analysis[J]. J Med Internet Res, 2014, 16(8):e192.
doi: 10.2196/jmir.3469 |
| [16] |
Kooiman TJ, Dontje ML, Sprenger SR, et al. Reliability and validity of ten consumer activity trackers[J]. BMC Sports Sci Med Rehabil, 2015, 7:24.
doi: 10.1186/s13102-015-0018-5 pmid: 26464801 |
| [17] |
Mancuso CA, Sculco TP, Wickiewicz TL, et al. Patients’ expectations of knee surgery[J]. J Bone Joint Surg Am, 2001, 83(7):1005-1012.
pmid: 11451969 |
| [18] |
Wang C, Zhang C, Liu DL, et al. Simplified Chinese version of hip and knee replacement expectations surveys in patients with osteoarthritis and ankylosing spondylitis: Cross-cultural adaptation, validation and reliability[J]. BMC Musculoskelet Disord, 2018, 19(1):247.
doi: 10.1186/s12891-018-2129-0 |
| [19] |
Cross M, Lapsley H, Barcenilla A, et al. Patient expectations of hip and knee joint replacement surgery and postoperative health status[J]. Patient, 2009, 2(1):51-60.
doi: 10.2165/01312067-200902010-00006 |
| [20] |
Mahomed NN, Liang MH, Cook EF, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty[J]. J Rheumatol, 2002, 29(6):1273-1279.
pmid: 12064846 |
| [21] |
Swarup I, Henn CM, Gulotta LV, et al. Patient expectations and satisfaction in orthopaedic surgery: A review of the literature[J]. J Clin Orthop Trauma, 2019, 10(4):755-760.
doi: 10.1016/j.jcot.2018.08.008 |
| [22] |
Zywiel MG, Mahomed A, Gandhi R, et al. Measuring expectations in orthopaedic surgery: A systematic review[J]. Clin Orthop Relat Res, 2013, 471(11):3446-3456.
doi: 10.1007/s11999-013-3013-8 |
| [23] |
Mancuso CA, Graziano S, Briskie LM, et al. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties[J]. Clin Orthop Relat Res, 2008, 466(2):424-431.
doi: 10.1007/s11999-007-0052-z |
| [24] | Scott CE, Bugler KE, Clement ND, et al. Patient expectations of arthroplasty of the hip and knee[J]. J Bone Joint Surg Br, 2012, 94(7):974-981. |
| [25] |
Harmsen RTE, Haanstra TM, Den Oudsten BL, et al. A high proportion of patients have unfulfilled sexual expectations after TKA: A prospective study[J]. Clin Orthop Relat Res, 2020, 478(9):2004-2016.
doi: 10.1097/CORR.0000000000001003 |
| [26] |
Muniesa JM, Marco E, Tejero M, et al. Analysis of the expectations of elderly patients before undergoing total knee replacement[J]. Arch Gerontol Geriatr, 2010, 51(3):e83-e87.
doi: 10.1016/j.archger.2010.01.003 |
| [27] | Lingard EA, Sledge CB, Learmonth ID, et al. Patient expectations regarding total knee arthroplasty: Differences among the United States, United Kingdom, and Australia[J]. J Bone Joint Surg Am, 2006, 88(6):1201-1207. |
| [28] |
Mancuso CA, Sculco TP, Salvati EA. Patients with poor preoperative functional status have high expectations of total hip arthroplasty[J]. J Arthroplasty, 2003, 18(7):872-878.
pmid: 14566742 |
| [29] | Yoo JH, Chang CB, Kang YG, et al. Patient expectations of total knee replacement and their association with sociodemographic factors and functional status[J]. J Bone Joint Surg Br, 2011, 93(3):337-344. |
| [30] |
Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty[J]. J Arthroplasty, 2009, 24(5):716-721.
doi: 10.1016/j.arth.2008.05.016 pmid: 18701241 |
| [31] |
Koenen P, Bäthis H, Schneider MM, et al. How do we face patients’ expectations in joint arthroplasty?[J] Arch Orthop Trauma Surg, 2014, 134(7):925-931.
doi: 10.1007/s00402-014-2012-x |
| [32] |
Kudibal MT, Kallemose T, Troelsen A, et al. Does ethnicity and education influence preoperative disability and expectations in patients undergoing total knee arthroplasty?[J] World J Orthop, 2018, 9(10):220-228.
doi: 10.5312/wjo.v9.i10.220 |
| [33] |
Barrack RL, Ruh EL, Chen J, et al. Impact of socioeconomic factors on outcome of total knee arthroplasty[J]. Clin Orthop Relat Res, 2014, 472(1):86-97.
doi: 10.1007/s11999-013-3002-y |
| [34] |
Bourne RB, Chesworth BM, Davis AM, et al. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not?[J] Clin Orthop Relat Res, 2010, 468(1):57-63.
doi: 10.1007/s11999-009-1119-9 |
| [35] |
Tolk JJ, Janssen RPA, Haanstra TM, et al. The influence of expectation modification in knee arthroplasty on satisfaction of patients: A randomized controlled trial [J]. Bone Joint J, 2021, 103-B(4):619-626.
doi: 10.1302/0301-620X.103B4.BJJ-2020-0629.R3 |
| [36] | Neter J, Kutner MH, Nachtsheim CJ, et al. Applied linear statistical models[M]. 4th ed. New York: McGraw-Hill/Irwin Companies, Inc., 1996. |
| [1] | 安思兰,郑群怡,王锴,高姗. 全膝关节置换术后患者早期疼痛的特点及其影响因素[J]. 北京大学学报(医学版), 2024, 56(1): 167-173. |
| [2] | 赵然,刘延青,田华. 应用累积和控制图分析全膝关节置换术中电子压力垫片指导软组织平衡的学习曲线[J]. 北京大学学报(医学版), 2023, 55(4): 658-664. |
| [3] | 叶一林,刘恒,潘利平,柴卫兵. 全膝关节置换术后假体周围痛风发作误诊1例[J]. 北京大学学报(医学版), 2023, 55(2): 362-365. |
| [4] | 王梓,张军军,左力,王悦,李文歌,程虹,蔡广研,裴华颖,王利华,周绪杰,师素芳,刘立军,吕继成,张宏. 血浆置换治疗新月体型IgA肾病的有效性分析: 多中心队列研究[J]. 北京大学学报(医学版), 2022, 54(5): 1038-1046. |
| [5] | 贾金凤,梁菲,黄建伟,王昊,韩璞青. 双重血浆分子吸附系统模式人工肝治疗对血小板的影响[J]. 北京大学学报(医学版), 2022, 54(3): 548-551. |
| [6] | 苗欣,黄红拾,胡晓青,时会娟,任爽,敖英芳. 膝关节前交叉韧带断裂后单腿位置觉测试时脑电功率谱的变化特征[J]. 北京大学学报(医学版), 2021, 53(5): 871-876. |
| [7] | 吴浩,潘利平,刘恒,塔拉提百克·买买提居马,王洪彬,宁太国,曹永平. 胫骨假体的不同后倾角度对内侧间室单髁置换术后膝关节功能的影响[J]. 北京大学学报(医学版), 2021, 53(5): 877-882. |
| [8] | 印钰,梅宇,王泽刚,宋首一,刘鹏飞,何鹏峰,武文杰,谢兴. 固定袢和可调节袢在粗骨道中的长度对股骨骨道增宽及膝关节功能的影响[J]. 北京大学学报(医学版), 2021, 53(5): 883-890. |
| [9] | 王鑫光,耿霄,李杨,吴天晨,李子剑,田华. 便携式导航与计算机导航辅助在全膝关节置换力线对准和手术时间的比较[J]. 北京大学学报(医学版), 2021, 53(4): 728-733. |
| [10] | 彭顺壮, 付茜茜, 冯星淋. 中国中老年居民教育程度与失能发生:社会参与的中介作用[J]. 北京大学学报(医学版), 2021, 53(3): 549-554. |
| [11] | 及松洁,黄野,王兴山,柳剑,窦勇,姜旭,周一新. Oxford膝关节单间室置换术后内翻多因素分析[J]. 北京大学学报(医学版), 2021, 53(2): 293-297. |
| [12] | 柯岩,张蔷,马云青,李儒军,陶可,桂先革,李克鹏,张洪,林剑浩. 全髋关节置换术治疗脊柱骨骺发育不良患者Tönnis 3级髋关节骨关节炎的早期疗效[J]. 北京大学学报(医学版), 2021, 53(1): 175-182. |
| [13] | 石茂静,高伟波,黄文凤,朱继红. 61例血栓性血小板减少性紫癜患者的临床分析[J]. 北京大学学报(医学版), 2021, 53(1): 210-214. |
| [14] | 刘中砥,许庭珉,党育,张殿英,付中国. 关节镜下改良outside-in穿刺缝合技术修复半月板撕裂的中期临床随访[J]. 北京大学学报(医学版), 2020, 52(5): 870-874. |
| [15] | 刘中砥,芦浩,袁玉松,徐海林. Swanson人工跖趾关节置换术治疗第2~5跖趾关节疾病的疗效评价[J]. 北京大学学报(医学版), 2020, 52(4): 726-729. |
|
||