北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (1): 182-186. doi: 10.19723/j.issn.1671-167X.2022.01.029
手臂位置对射波刀放射治疗脊柱肿瘤患者的剂量学影响
李君1,刘旭红2,3,王工1,程程1,庄洪卿1,杨瑞杰1,△( )
)
- 1.北京大学第三医院肿瘤放射治疗科,北京 100191
2.云南省肿瘤医院放射治疗科,昆明 650018
3.昆明医科大学第三附属医院放射治疗科,昆明 650018
Dosimetric effect of patient arm position on Cyberknife radiosurgery for spinal tumors
LI Jun1,LIU Xu-hong2,3,WANG Gong1,CHENG Cheng1,ZHUANG Hong-qing1,YANG Rui-jie1,△( )
)
- 1. Department of Radiation Oncology, Peking University Third Hospital, Beijing 100191, China
2. Yunnan Cancer Hospital, Kunming 650018, China
3. The Third Affiliated Hospital of Kunming Medical University, Kunming 650018, China
摘要:
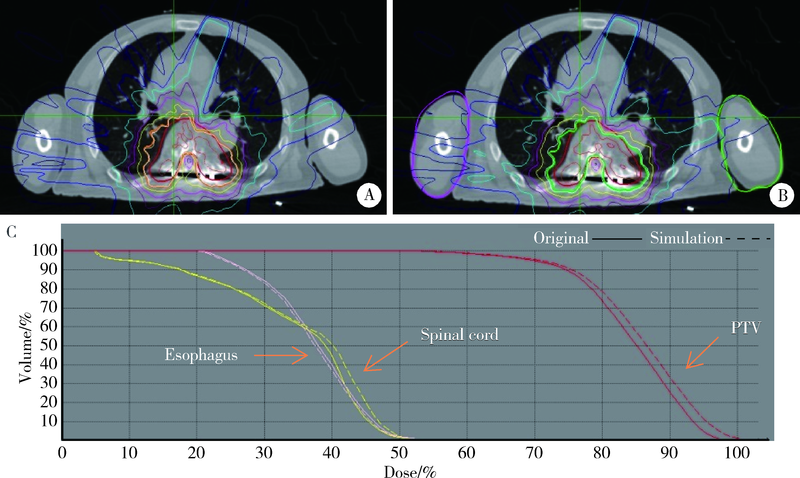
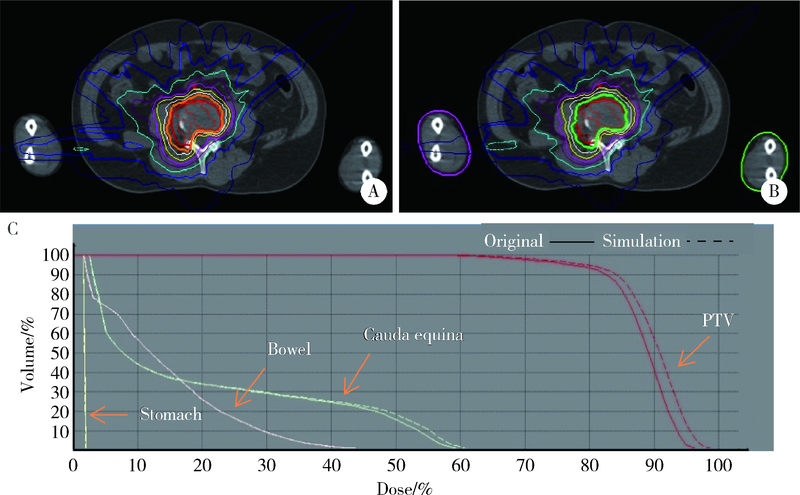
目的: 评估患者手臂位置变化对射波刀脊柱肿瘤放射治疗潜在剂量学的影响。方法: 选取胸椎与腰椎肿瘤患者各12例,勾画患者手臂轮廓并修改CT值和密度,使其等效为空气,模拟手臂完全移出射野的极端情况。保留原治疗计划的射束条件再次计算剂量,通过与原始计划的剂量体积直方图(dose-volume histogram, DVH)的参数比较,分析计划靶区(planning target volume, PTV)100%处方剂量的覆盖体积(V100)、95%PTV体积受照剂量(D95)、90%PTV体积受照剂量(D90)、适形指数(conformity index, CI)与异质性指数(heterogeneity index, HI),以及脊髓、胃、食管、肠道的最大受照剂量(Dmax)、1cc体积(1 mL)受照剂量(D1cc)和2cc体积(2 mL)受照剂量(D2cc)的变化。结果: 与原治疗计划相比,模拟计划的PTV V100、D95、D90、CI平均升高0.86%、2.02%、1.97%、0.80%,差异有统计学意义(P < 0.05);脊髓Dmax、D1cc与D2cc平均升高2.35%、2.59%、1.49%,差异有统计学意义(P < 0.05);胃D2cc平均升高1.70%,差异有统计学意义(P < 0.05);食管与肠道剂量差异无统计学意义。结论: 在基于射波刀的脊柱肿瘤放射治疗过程中最极端的双臂位置情况下,发现手臂位置的改变对剂量学影响很小,并且随手臂位置的改变,靶区与危及器官(organ at risk, OAR)的剂量有所增加,但增幅相对较小,因此,在某些特殊情况下,患者确实无法始终保持手臂位置一致时,可以进行合理的调整,但是为了保证剂量的精确投照,应尽可能实现患者治疗体位的稳定性与一致性。
中图分类号:
- R739.92
| [1] |
Sahgal A, Chang JH, Ma L, et al. Spinal cord dose tolerance to stereotactic body radiation therapy[J]. Int J Radiat Oncol Biol Phys, 2021, 110(1):124-136.
doi: 10.1016/j.ijrobp.2019.09.038 |
| [2] | Hwang L, Okoye CC, Patel RB, et al. Stereotactic body radiotherapy for benign spinal tumors: Meningiomas, schwannomas, and neurofibromas[J]. J Radiosurg SBRT, 2019, 6(3):167-177. |
| [3] |
Hariri O, Takayanagi A, Lischalk J, et al. Clinical efficacy of frameless stereotactic radiosurgery in the management of spinal metastases from thyroid carcinoma[J]. Spine, 2019, 44(20):1188-1195.
doi: 10.1097/BRS.0000000000003087 pmid: 31261273 |
| [4] | 张喜乐, 杨瑞杰, 李君, 等. 射波刀VSI系统主要性能测试[J]. 中华放射肿瘤学杂志, 2018, 27(10):925-929. |
| [5] | 张喜乐, 杨瑞杰, 李君, 等. 四种探测器测量射波刀离轴比曲线的比较分析[J]. 中华放射医学与防护杂志, 2017, 37(9):671-676. |
| [6] | 程光惠, 武宁, 韩东梅, 等. 不同体位固定技术在胸腹部肿瘤放射治疗中的应用比较[J]. 中国肿瘤, 2010, 19(10):702-704. |
| [7] | 司小三. 不同体位固定技术在胸腹部肿瘤放射治疗中的临床效果观察[J]. 白求恩医学杂志, 2017, 15(6):789-791. |
| [8] |
Shultz DB, Jang SS, Hanlon AL, et al. The effect of arm position on the dosimetry of thoracic stereotactic ablative radiation therapy using volumetric modulated arc therapy[J]. Pract Radiat Oncol, 2014, 4:192-197.
doi: S1879-8500(13)00272-5 pmid: 24766687 |
| [9] |
Moore K, Paterson C, Hicks J, et al. Stereotactic ablative body radiotherapy for non-small-cell lung cancer: setup reproducibility with novel arms-down immobilization[J]. Br J Radiol, 2016, 89(1068):20160227.
doi: 10.1259/bjr.20160227 |
| [10] |
Murrell DH, Karnas SJ, Corkum MT, et al. Radical radiotherapy for locally advanced non-small cell lung cancer-what’s up with arm positioning?[J]. J Thorac Dis, 2019, 11(5):2099-2104.
doi: 10.21037/jtd.2019.05.40 pmid: 31285903 |
| [11] | 王建军, 刘邦, 刘伟. 手臂位置对采用容积调制弧光疗法进行胸腔立体定向放疗的影响[J]中西医结合心血管病电子杂志, 2020, 8(20):168-173. |
| [12] |
Fürweger C, Drexler C, Muacevic A, et al. CyberKnife robotic spinal radiosurgery in proneposition: dosimetric advantage due to posterior radiation access?[J]. J Appl Clin Med Phys, 2014, 15(4):11-21.
doi: 10.1120/jacmp.v15i4.4427 |
| [13] |
Lin C, Donaldson SS, Meza JL, et al. Effect of radiotherapy techniques (IMRT vs. 3D-CRT) on outcome in patients with inter-mediate-risk rhabdomyosarcoma enrolled in COG D9803: a report from the Children’s Oncology Group[J]. Int J Radiat Oncol Biol Phys, 2012, 82(5):1764-1770.
doi: 10.1016/j.ijrobp.2011.01.036 |
| [14] |
Rao AD, Chen Q, Million L, et al. Preoperative intensity modulated radiation therapy compared to three-dimensional conformal radiation therapy for high-grade extremity sarcomas in children: analysis of the children’s oncology group study ARST0332[J]. Int J Radiat Oncol Biol Phys, 2019, 103(1):38-44.
doi: 10.1016/j.ijrobp.2018.09.005 |
| [1] | 孙海涛,杨瑞杰,江萍,姜伟娟,李金娜,孟娜,王俊杰. 乳腺癌保乳术后容积旋转调强和切线野调强放疗的剂量学比较[J]. 北京大学学报(医学版), 2018, 50(1): 188-192. |
| [2] | 李彦,姜亮,刘晓光,刘忠军,韦峰,吴奉梁,党礌. 肺癌脊柱转移瘤的手术治疗疗效及生存分析[J]. 北京大学学报(医学版), 2014, 46(1): 138-143. |
|
||