北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (5): 927-935. doi: 10.19723/j.issn.1671-167X.2022.05.020
改良牙冠延长术后组织愈合的动物实验研究
- 1. 北京大学口腔医学院·口腔医院牙周科,国家口腔医学中心,国家口腔疾病临床医学研究中心,口腔生物材料和数字诊疗装备国家工程研究中心,国家卫生健康委员会口腔医学计算机应用工程技术研究中心,北京 100081
2. 北京大学口腔医学院·口腔医院中心实验室,国家口腔医学中心,国家口腔疾病临床医学研究中心,口腔生物材料和数字诊疗装备国家工程研究中心,国家卫生健康委员会口腔医学计算机应用工程技术研究中心,北京 100081
Healing of the dento-gingival junction following modified crown lengthening procedure in beagle dogs
Min ZHEN1,Huan-xin MENG1,Wen-jie HU1,*( ),Deng-cheng WU2,Yi-ping WEI1
),Deng-cheng WU2,Yi-ping WEI1
- 1. Department of Periodontology, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & NHC Research Center of Engineering and Technology for Computerized Dentistry, Beijing 100081, China
2. Central Laboratory, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & NHC Research Center of Engineering and Technology for Computerized Dentistry, Beijing 100081, China
摘要:
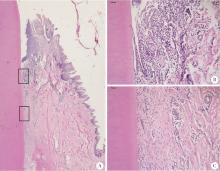
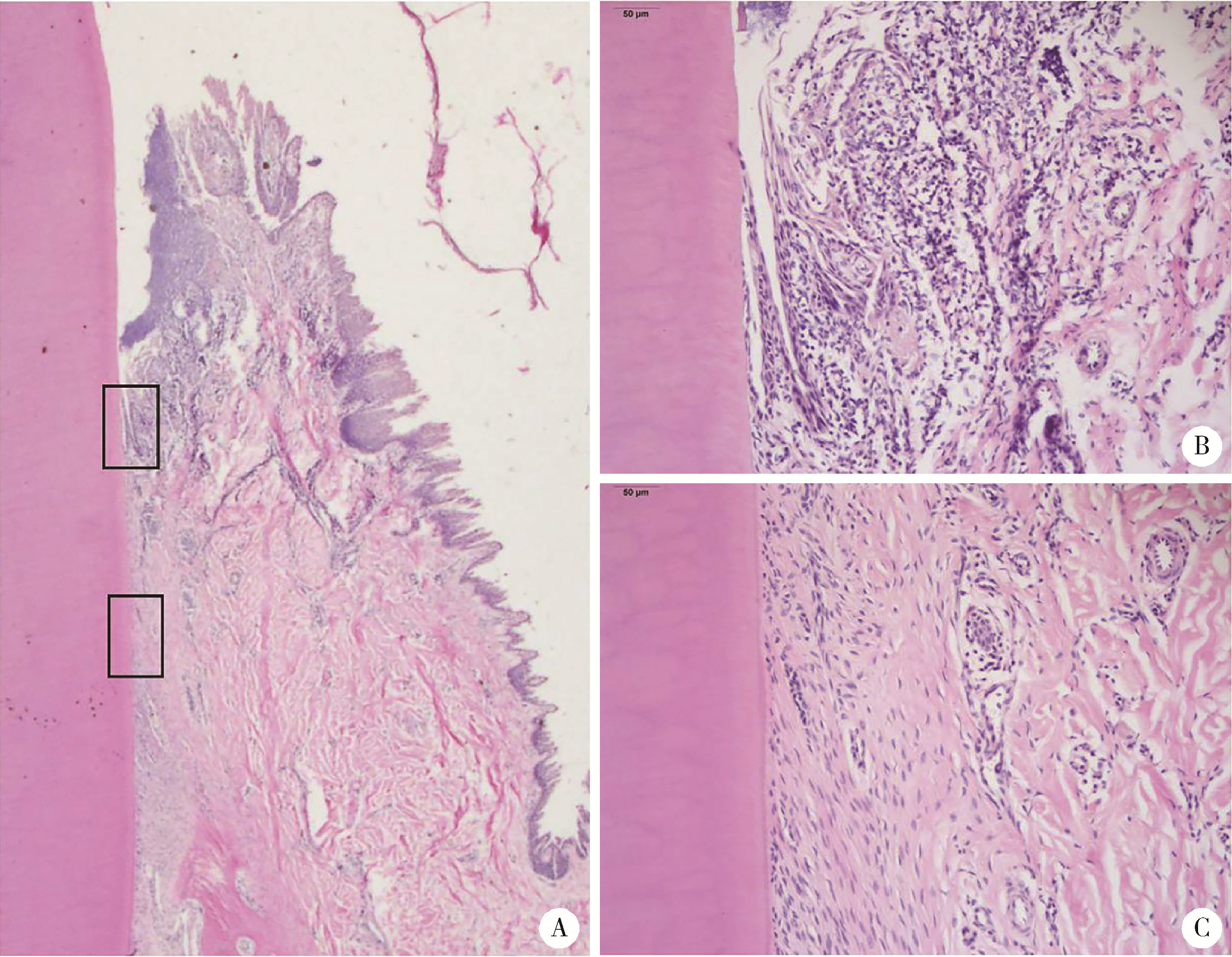
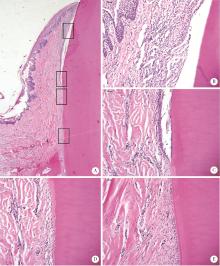
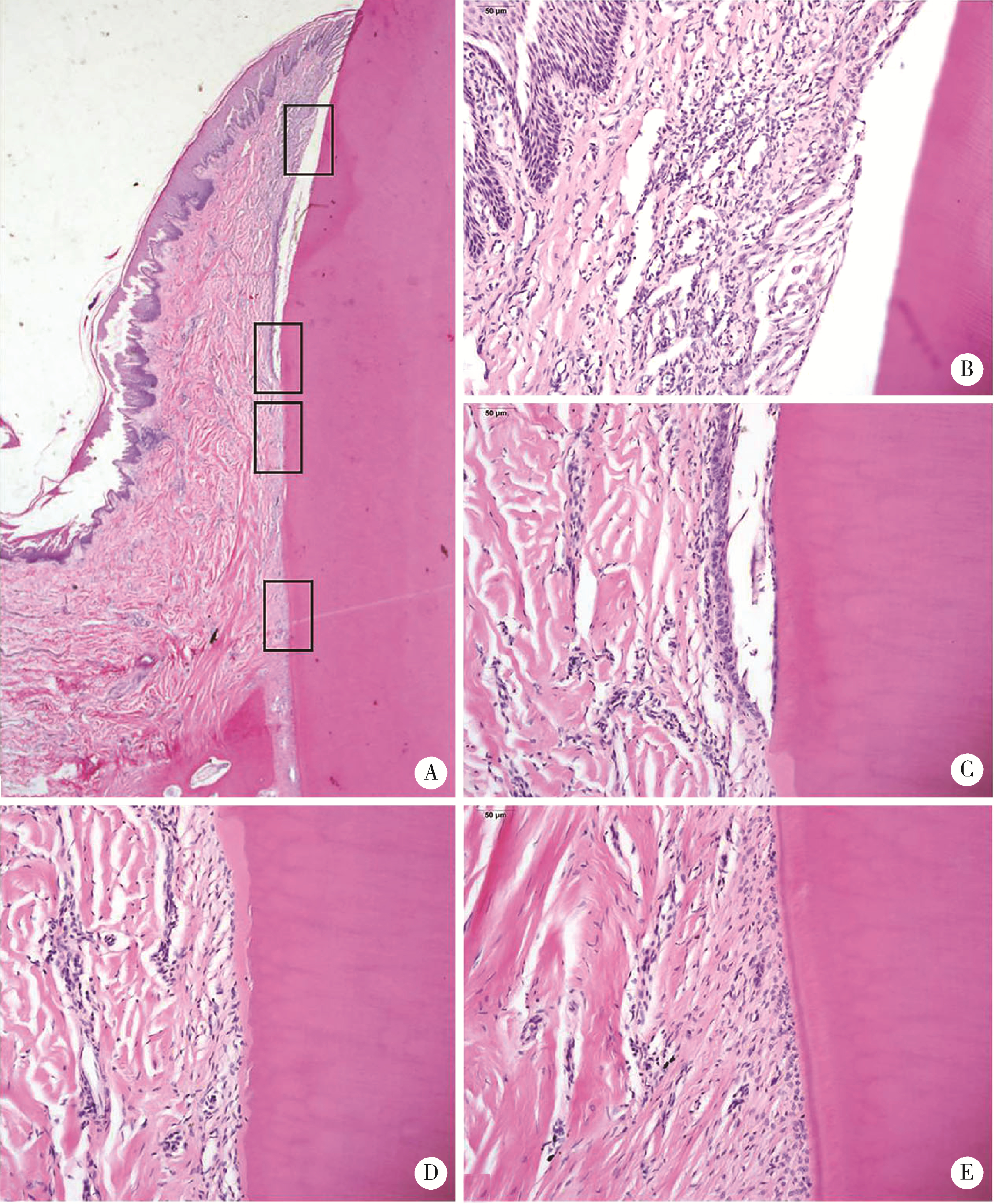
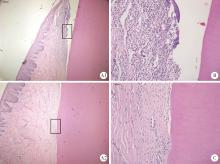
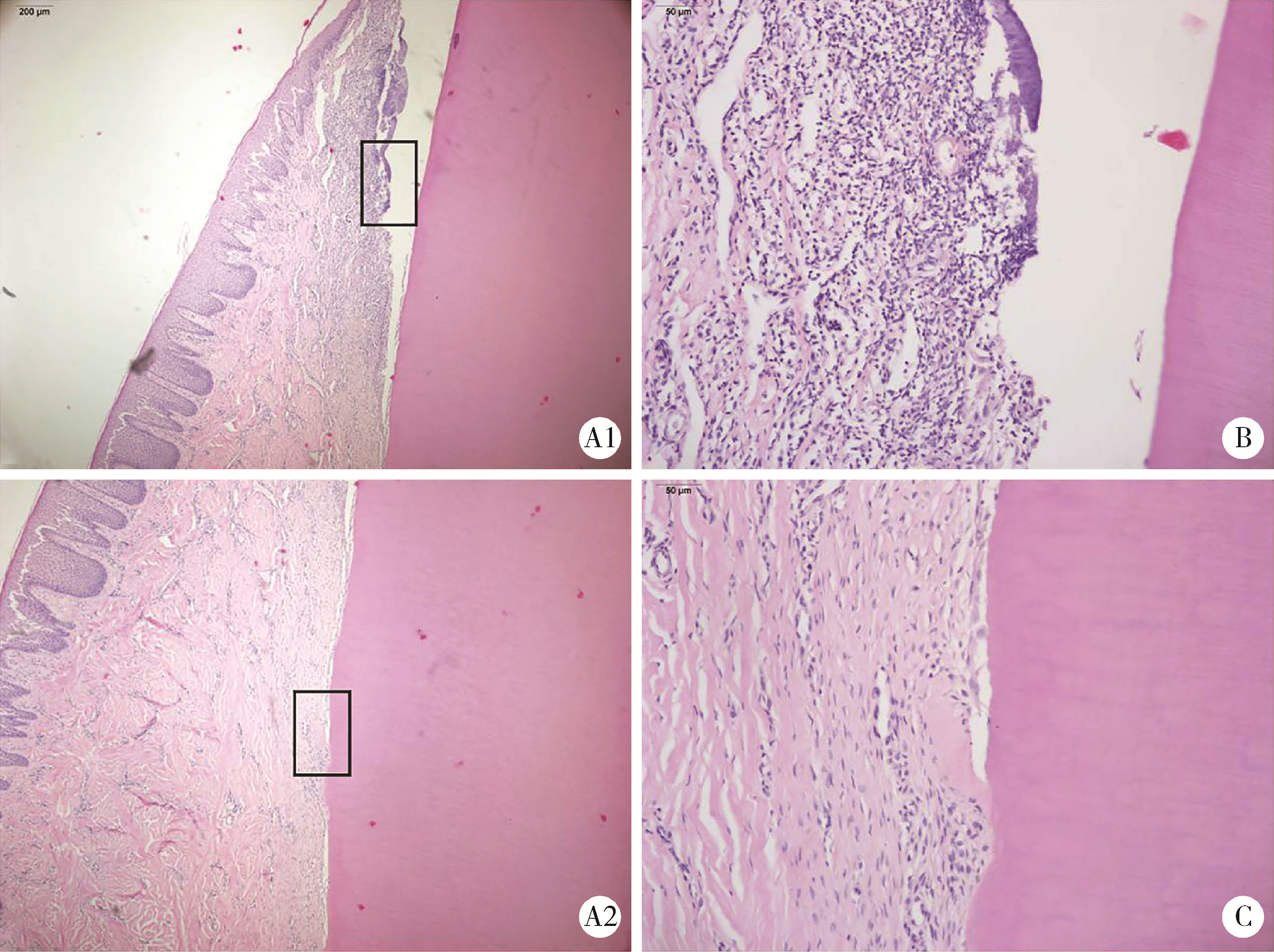
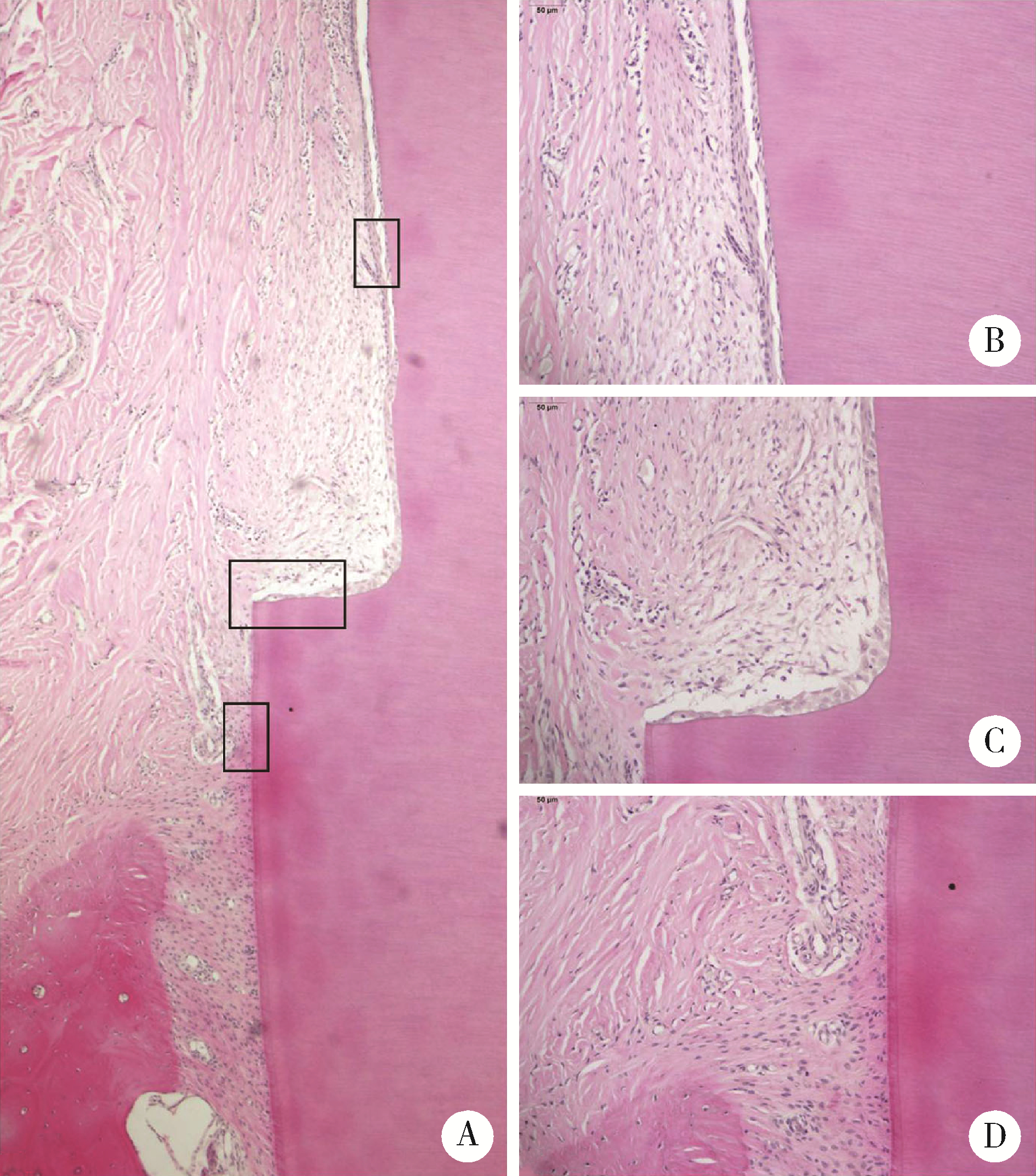
目的: 明确改良牙冠延长术后的组织愈合方式, 为改良牙冠延长术的临床推广应用提供生物学基础。方法: 对5只比格犬的右上中切牙、左上中切牙和左上第一侧切牙分别进行翻瓣术、常规牙冠延长术和改良牙冠延长术, 右上第一侧切牙为对照牙, 不进行手术, 术后36周获取标本进行组织学观察。结果: 颊舌向软硬组织切片苏木素-伊红(hematoxylin-eosin, HE)染色发现翻瓣术的愈合方式为再附着, 与对照组一致。常规牙冠延长术组5只比格犬的根面均存在薄片状的牙骨质缺损, 其中4只比格犬的组织愈合为新附着, 表现为牙骨质缺损区内有新牙骨质形成, 胶原纤维呈一定角度插入其中; 另1只比格犬的组织愈合方式为长结合上皮愈合, 表现为长结合上皮根向移位止于牙骨质缺损区的根方水平。改良牙冠延长术组中4只比格犬根面存在牙骨质缺损(薄片状和浅台阶样缺损各2只), 其中3只比格犬的组织愈合为新附着, 但胶原纤维与根面平行, 1只比格犬的愈合方式为长结合上皮愈合; 另外1只比格犬因组织块未能完整分切而无法观察组织愈合方式。结论: 改良牙冠延长术后的组织愈合方式与常规法相似, 包括新附着和长结合上皮愈合两种方式, 根面处理(根面平整或根面改形)以及根面缺损的类型(薄片状或浅台阶样牙骨质缺损)并未影响组织的愈合方式。
中图分类号:
- R782.1
| 1 |
Brägger U , Lauchenauer D , Lang NP . Surgical lengthening of the clinical crown[J]. J Clin Periodontol, 1992, 19 (1): 58- 63.
doi: 10.1111/j.1600-051X.1992.tb01150.x |
| 2 |
欧阳翔英. 有助于残根修复的牙冠延长术[J]. 中华口腔医学杂志, 2004, 39 (3): 205- 207.
doi: 10.3760/j.issn:1002-0098.2004.03.008 |
| 3 |
Gargiulo AW , Wentz FM , Orban B . Dimensions and relations of the dentogingival junction in humans[J]. J Periodontol, 1961, 32 (3): 261- 267.
doi: 10.1902/jop.1961.32.3.261 |
| 4 | Melker DJ , Richardson CR . Root reshaping: an integral component of periodontal surgery[J]. Int J Periodontics Restorative Dent, 2001, 21 (3): 296- 304. |
| 5 |
胡文杰, 李连生, 张豪, 等. 牙根改形结合少量去骨: 一种改良的牙冠延长术[J]. 北京大学学报(医学版), 2008, 40 (1): 83- 87.
doi: 10.3321/j.issn:1671-167X.2008.01.022 |
| 6 |
甄敏, 胡文杰, 张豪, 等. 改良牙冠延长术术后1至6年疗效观察[J]. 中华口腔医学杂志, 2012, 47 (4): 203- 207.
doi: 10.3760/cma.j.issn.1002-0098.2012.04.003 |
| 7 |
Zhen M , Wang C , Hu WJ , et al. Periodontal evaluation of crown-root fractured teeth following modified crown lengthening surgery[J]. Br Dent J, 2017, 222 (1): 21- 25.
doi: 10.1038/sj.bdj.2017.25 |
| 8 |
da Cruz MK , Martos J , Silveira LF , et al. Odontoplasty associated with clinical crown lengthening in management of extensive crown destruction[J]. J Conserv Dent, 2012, 15 (1): 56- 60.
doi: 10.4103/0972-0707.92608 |
| 9 |
甄敏, 危伊萍, 胡文杰, 等. 不同冠延长术式处理上中切牙冠根折并桩核冠修复的三维有限元比较[J]. 中华口腔医学杂志, 2016, 51 (6): 362- 367.
doi: 10.3760/cma.j.issn.1002-0098.2016.06.009 |
| 10 |
Wang C , Jia XT , Zhen M , et al. Success rate of fractured teeth receiving modified crown lengthening surgery and restorations[J]. BMC Oral Health, 2022, 22 (1): 99.
doi: 10.1186/s12903-022-02143-z |
| 11 |
王翠, 贾雪婷, 胡文杰, 等. 改良牙冠延长术后长期临床疗效评价及其影响因素分析[J]. 中华口腔医学杂志, 2017, 52 (3): 182- 187.
doi: 10.3760/cma.j.issn.1002-0098.2017.03.011 |
| 12 | Oakley E , Rhyu IC , Karatzas S , et al. Formation of the biologic width following crown lengthening in nonhuman primates[J]. Int J Periodontics Restorative Dent, 1999, 19 (6): 529- 541. |
| 13 |
Selvig KA , Torabinejad M . Wound healing after mucoperiosteal surgery in the cat[J]. J Endod, 1996, 22 (10): 507- 515.
doi: 10.1016/S0099-2399(96)80008-2 |
| 14 | Carnevale G , Sterrantino SF , Di Febo G . Soft and hard tissue wound healing following tooth preparation to the alveolar crest[J]. Int J Periodontics Restorative Dent, 1983, 3 (6): 36- 53. |
| 15 |
Levine HL , Stahl SS . Repair following periodontal flap surgery with the retention of gingival fibers[J]. J Periodontol, 1972, 43 (2): 99- 103.
doi: 10.1902/jop.1972.43.2.99 |
| 16 |
Claffey N , Motsinger S , Ambruster J , et al. Placement of a porous membrane underneath the mucoperiosteal flap and its effect on periodontal wound healing in dogs[J]. J Clin Periodontol, 1989, 16 (1): 12- 16.
doi: 10.1111/j.1600-051X.1989.tb01605.x |
| 17 |
Steiner SS , Crigger M , Egelberg J . Connective tissue regeneration to periodontally diseased teeth. Ⅱ. Histologic observations of cases following replaced flap surgery[J]. J Periodontal Res, 1981, 16 (1): 109- 116.
doi: 10.1111/j.1600-0765.1981.tb00954.x |
| 18 |
Caton J , Nyman S . Histometric evaluation of periodontal surgery. Ⅲ. The effect of bone resection on the connective tissue attachment level[J]. J Periodontol, 1981, 52 (8): 405- 409.
doi: 10.1902/jop.1981.52.8.405 |
| 19 |
Wilderman MN , Pennel BM , King K , et al. Histogenesis of repair following osseous surgery[J]. J Periodontol, 1970, 41 (10): 551- 565.
doi: 10.1902/jop.1970.41.10.551 |
| 20 |
Lindskog S , Blomlöf L . Mineralized tissue-formation in periodontal wound healing[J]. J Clin Periodontol, 1992, 19 (10): 741- 748.
doi: 10.1111/j.1600-051X.1992.tb02164.x |
| 21 | Middleton CT , Bowers GM . Histologic evaluation of cementogenesis on periodontitis-affected roots in humans[J]. Int J Periodontics Restorative Dent, 1990, 10 (6): 428- 435. |
| [1] | 汪琪伟, 包鹏宇, 洪士皓, 杨昕, 王宇, 曹永平. 改良股骨颈截骨术在伴严重屈曲畸形强直性脊柱炎患者手术治疗过程中的疗效[J]. 北京大学学报(医学版), 2024, 56(5): 884-889. |
| [2] | 张雯,刘筱菁,李自力,张益. 基于解剖标志的鼻翼基底缩窄缝合术对正颌患者术后鼻唇部形态的影响[J]. 北京大学学报(医学版), 2023, 55(4): 736-742. |
| [3] | 郭玉兴,张建运,王佃灿,郭传瑸. 药物相关颌骨骨坏死的病理特点及临床治疗策略[J]. 北京大学学报(医学版), 2022, 54(6): 1190-1195. |
| [4] | 刘恒,李卓扬,曹永平,崔云鹏,吴浩. 胫骨侧徒手截骨的膝关节置换术后力线测量及其影响因素分析[J]. 北京大学学报(医学版), 2018, 50(5): 850-854. |
| [5] | 曹婕1,孟焕新. 锥形束CT用于评估牙槽骨骨缺损的情况和骨再生区域骨密度的变化[J]. 北京大学学报(医学版), 2018, 50(1): 110-116. |
| [6] | 吴煜,李自力,王兴, 伊彪, 马莲. 腭侧入路改良Le Fort Ⅰ型截骨术矫正唇腭裂继发上颌骨发育不足的临床初步应用[J]. 北京大学学报(医学版), 2016, 48(3): 550-554. |
| [7] | 赵旻暐,田华,曾琳,李邦国,张峰霖,李凌宇. 中国人采用胫骨结节及胫前肌腱定位的髓外截骨法术后胫骨假体冠状位力线的测量与分析[J]. 北京大学学报(医学版), 2016, 48(2): 351-355. |
| [8] | 杨胜松,黄雷,滕星,王陶,王满宜. 外固定架辅助髓内钉治疗膝外翻或膝内翻畸形[J]. 北京大学学报(医学版), 2016, 48(2): 244-249. |
| [9] | 何伟, 谢晓艳, 王兴, 王晓霞, 傅开元, 李自力. 上颌Le FortⅠ型分块截骨术及双侧下颌升支矢状劈开术对骨性Ⅲ类错牙合畸形患者髁突位置的影响[J]. 北京大学学报(医学版), 2015, 47(5): 829-833. |
| [10] | 白洁, 赵玉鸣, 秦满. 儿童恒牙全脱出牙周组织预后的回顾性研究[J]. 北京大学学报(医学版), 2015, 47(2): 312-316. |
| [11] | 褚亚明, 周一新, 寇玉辉, 杨德金. 股骨转子下截骨全髋置换术治疗Hartofilakidis C1和C2型髋关节发育不良的对比研究[J]. 北京大学学报(医学版), 2015, 47(2): 232-236. |
| [12] | 王宗琦, 王晓霞, 李自力, 伊彪, 梁成, 王兴. 3种缝合方法控制上颌Le Fort Ⅰ型截骨术后鼻翼宽度的效果比较[J]. 北京大学学报(医学版), 2015, 47(1): 104-108. |
| [13] | 欧阳翔英, 阳雯. 转化医学及其在牙周干细胞研究中的应用[J]. 北京大学学报(医学版), 2013, 45(1): 152-155. |
| [14] | 朱卫东, 侯建霞, 刘凯宁, 孟焕新, 唐晓琳. 自体牙周膜细胞和釉基质蛋白修复猴下后牙Ⅲ度根分叉病变[J]. 北京大学学报(医学版), 2009, 41(1): 56-61. |
| [15] | 李淳德, 李宏, 刘宪义. 后路脊柱截骨矫形治疗重度僵硬后凸型脊柱侧凸[J]. 北京大学学报(医学版), 2007, 39(4): 399-402. |
|
||