北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (5): 893-898. doi: 10.19723/j.issn.1671-167X.2023.05.018
术前2 h口服碳水化合物对妇科腹腔镜特殊体位手术患者胃容量及反流误吸风险的影响
- 1. 北京大学国际医院 麻醉科, 北京 102206
2. 北京大学国际医院 妇科, 北京 102206
Effect of preoperative carbohydrates intake on the gastric volume and the risk of reflux aspiration in patients positioning in trendelenburg undergoing gynecological laparoscopic procedures
Yue WEI1,Xi LU1,Jing ZHANG2,Kun-peng LIU1,Yong-jun WANG2,Lan YAO1,*( )
)
- 1. Department of Anesthesiology, Peking University International Hospital, Beijing 102206, China
2. Department of Gynecology, Peking University International Hospital, Beijing 102206, China
摘要:
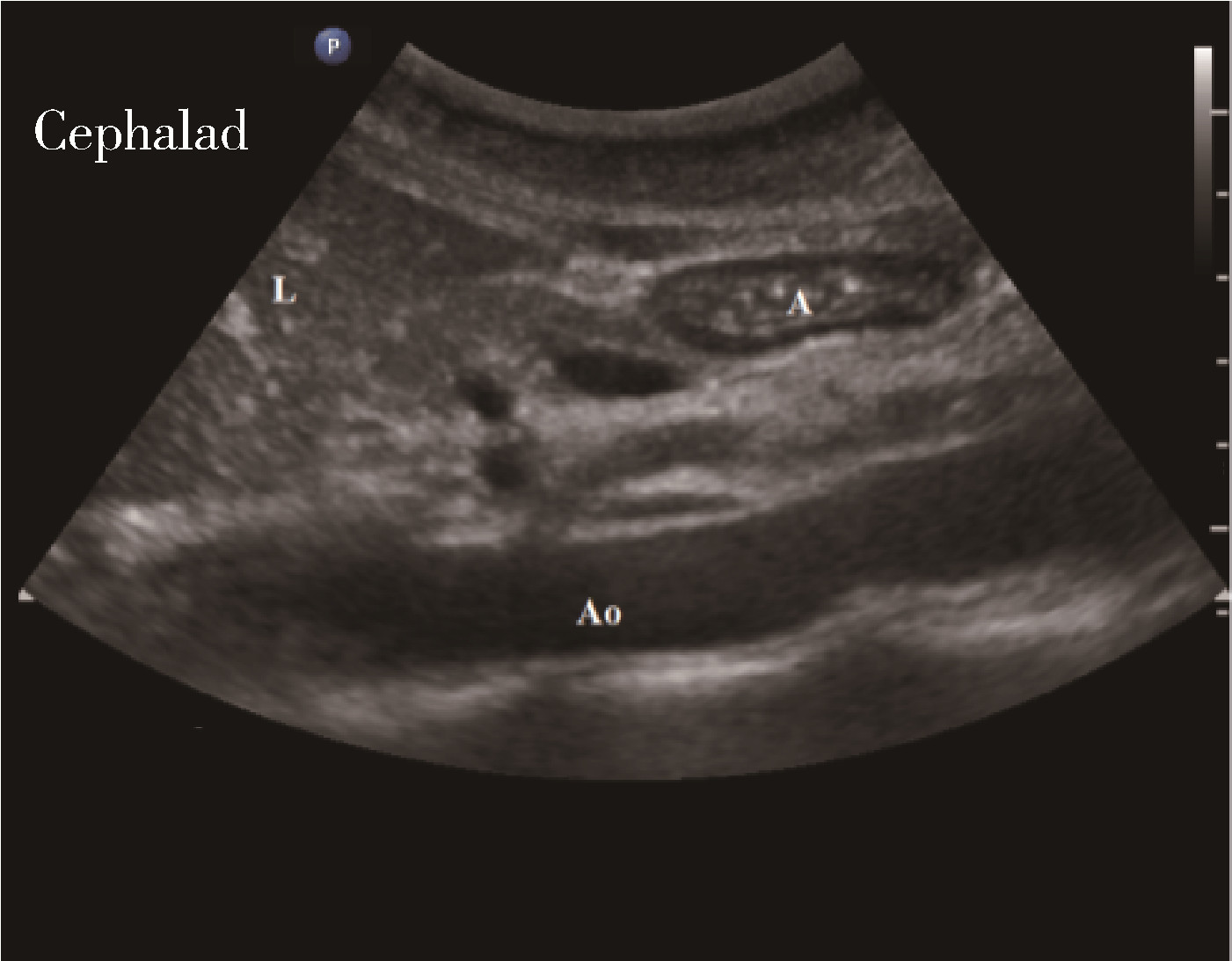
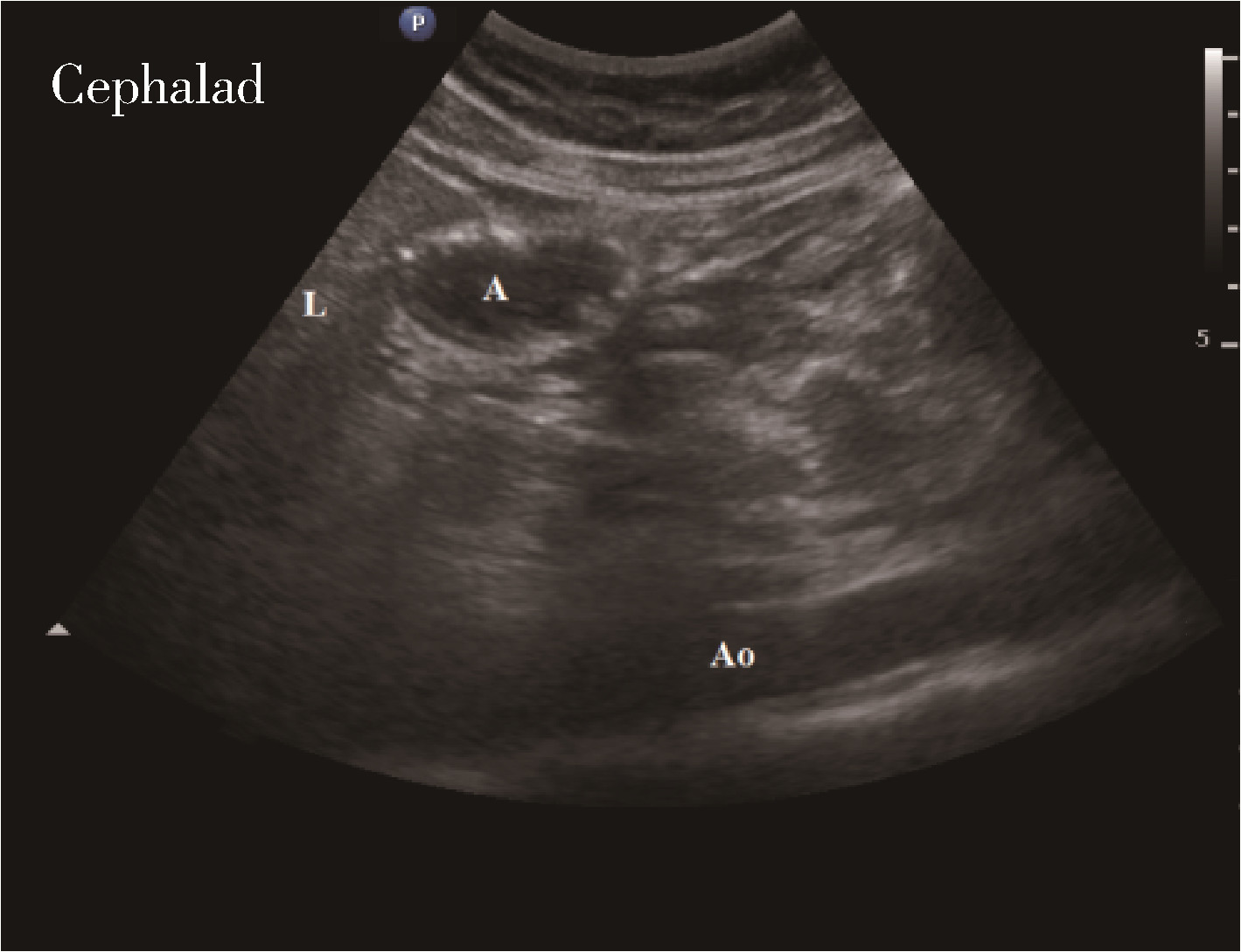
目的: 麻醉前超声测量胃窦部横截面积(cross-sectional area, CSA), 观察术前2 h口服碳水化合物300 mL对妇科腹腔镜手术特殊头低臀高仰卧截石体位患者麻醉前胃容量(gastric volume, GV)的影响, 并评估患者发生反流误吸的风险。方法: 选择2020年6月至2021年2月在北京大学国际医院择期行妇科腹腔镜手术特殊头低臀高仰卧截石体位患者80例, 年龄18~65岁, 体重指数18~35 kg/m2, 美国麻醉医师学会(American Society of Anesthesiologists, ASA)分级Ⅰ或Ⅱ级。采用随机数字表法将患者随机分为干预组和对照组, 每组40例。干预组患者手术前一日24:00后禁食, 对于首台手术患者, 手术日5:30口服碳水化合物300 mL; 对于接台手术患者在预计手术开始前2 h口服碳水化合物300 mL。对照组患者于手术前一日24:00后常规禁食禁饮。麻醉前分别在仰卧位和右侧卧位下行胃窦部超声检查。记录仰卧位和右侧卧位下CSA, 计算出两组患者麻醉前GV, 使用Perlas A半定量评级及胃容量/体质量(gastric volume/weight, GV/W)评估患者发生反流误吸的风险, 记录术前口渴感、饥饿感视觉模拟评分(visual analogue scale, VAS)等。结果: 两组共80例患者均完成胃窦部超声评估及测量, 干预组和对照组麻醉前GV分别为(58.8±23.6) mL和(56.3±22.1) mL, GV/W分别为(0.97±0.39) mL/kg和(0.95±0.35) mL/kg, 上述指标两组间差异均无统计学意义(P>0.05)。Perlas A半定量评级: 干预组0级24例(60%), 1级15例(37.5%), 2级1例(2.5%); 对照组0级25例(62.5%), 1级13例(32.5%), 2级2例(5%), 两组评级构成比差异无统计学意义(P>0.05)。两组共3例(干预组1例, 对照组2例)Perlas A半定量评级为2级的患者, 经干预, 均未发生反流误吸。与对照组比较, 干预组术前口渴感、饥饿感VAS明显降低(P<0.05)。结论: 妇科腹腔镜手术特殊头低臀高仰卧截石体位患者术前2 h口服300 mL碳水化合物, 麻醉前胃容量未见增加, 反流误吸风险未见增加, 对患者生理需求的干扰减少, 患者舒适度增加。
中图分类号:
- R614
| 1 |
Nelson G , Kiyang LN , Crumley ET , et al. Implementation of enhanced recovery after surgery (eras) across a provincial healthcare system: The ERAS Alberta colorectal surgery experience[J]. World J Surg, 2016, 40 (5): 1092- 1103.
doi: 10.1007/s00268-016-3472-7 |
| 2 |
Nygren J , Thacker J , Carli F , et al. Guidelines for perioperative care in elective rectal /pelvic surgery: Enhanced recovery after surgery (ERAS) society recommendations[J]. Clin Nutr, 2012, 31 (6): 801- 816.
doi: 10.1016/j.clnu.2012.08.012 |
| 3 | 赵国胜, 马晓玲. 妇科腹腔镜手术对生理的影响及麻醉处理[J]. 中国误诊学杂志, 2007, 7 (12): 3. |
| 4 | Park YT , Nogami M , Okano S . Influence of trendelenburg position and pneumoperitoneum treatment on gastroesophageal reflux in dogs[J]. Pol J Vet Sci, 2017, 20 (4): 823- 826. |
| 5 |
文亚杰, 吴昌彬, 林金坤, 等. 全麻下妇科腹腔镜手术患者胃食管反流的发生喉罩和气管导管通气下的比较[J]. 中华麻醉学杂志, 2005, 25 (11): 814- 816.
doi: 10.3760/j.issn:0254-1416.2005.11.004 |
| 6 | Roberts CJ , Goodman NW . Gastro-oesophageal reflux during elective laparoscopy[J]. Anaesthesia, 2010, 45 (12): 1009- 1011. |
| 7 | 孙晓黎, 李洁, 王振元, 等. 引流型喉罩对头低位腹腔镜手术反流误吸的影响[J]. 临床麻醉学杂志, 2013, 29 (8): 2. |
| 8 | Ho B , Skinner HJ , Mahajan RP . Gastro-oesophageal reflux during day case gynaecological laparoscopy under positive pressure ventilation: Laryngeal mask vs. tracheal intubation[J]. Anaesthesia, 2015, 53 (9): 921- 924. |
| 9 |
Bouvet L , Mazoit JX , Chassard D , et al. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume[J]. Anesthesiology, 2011, 114 (5): 1086- 1092.
doi: 10.1097/ALN.0b013e31820dee48 |
| 10 |
Perlas A , Davis L , Khan M , et al. Gastric sonography in the fasted surgical patient: A prospective descriptive study[J]. Anesth Analg, 2011, 113 (1): 93- 97.
doi: 10.1213/ANE.0b013e31821b98c0 |
| 11 |
Perlas A , Mitsakakis N , Liu L , et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination[J]. Anesth Analg, 2013, 116 (2): 357- 363.
doi: 10.1213/ANE.0b013e318274fc19 |
| 12 | 中华医学会妇产科学分会加速康复外科协作组. 妇科手术加速康复的中国专家共识[J]. 中华妇产科杂志, 2019, 54 (2): 7. |
| 13 |
Putte VD , Perlas A . Ultrasound assessment of gastric content and volume[J]. Br J Anaesth, 2014, 113 (1): 12- 22.
doi: 10.1093/bja/aeu151 |
| 14 |
Gola W , Domagala M , Cugowski A . Ultrasound assessment of gastric emptying and the risk of aspiration of gastric contents in the perioperative period[J]. Anaesthesiol Intensive Ther, 2018, 50 (4): 297- 302.
doi: 10.5603/AIT.a2018.0029 |
| 15 | Tosun B , Yava A , Acikel C . Evaluating the effects of preoperative fasting and fluid limitation[J]. Int J Nurs Pract, 2014, 21 (2): 156- 165. |
| 16 | 吕毅. 围术期处理[M]. 北京: 人民卫生出版社, 2018: 92. |
| 17 |
Gustafsson UO , Hausel J , Thorell A , et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery[J]. Arch Surg, 2011, 146 (5): 571- 577.
doi: 10.1001/archsurg.2010.309 |
| 18 |
Tsutsumi R , Kakuta N , Kadota T , et al. Effects of oral carbohydrate with amino acid solution on the metabolic status of patients in the preoperative period: A randomized, prospective clinical trial[J]. J Anesth, 2016, 30 (5): 842- 849.
doi: 10.1007/s00540-016-2217-y |
| 19 |
Shiraishi T , Kurosaki D , Nakamura M , et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: A magnetic resonance imaging-based analysis[J]. Anesth Analg, 2017, 124 (4): 1174- 1178.
doi: 10.1213/ANE.0000000000001886 |
| 20 | Fawcett WJ , Thomas M . Pre-operative fasting in adults and children: Clinical practice and guidelines[J]. Anaesthesia, 2019, 74 (1): 83- 88. |
| [1] | 魏越,姚兰,陆希,王军,蔺莉,刘鲲鹏. 胃超声检查评估剖宫产产妇术前饮用碳水化合物后胃排空的效果[J]. 北京大学学报(医学版), 2023, 55(6): 1082-1087. |
| [2] | 王少刚, 余虓. 经皮肾镜碎石术——日间手术新探索[J]. 北京大学学报(医学版), 2017, 49(5): 753-755. |
|
||