北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (1): 150-156. doi: 10.19723/j.issn.1671-167X.2024.01.023
急性前壁ST段抬高型心肌梗死患者直接冠状动脉介入术后微循环阻力指数与左心室不良重构的相关性
王方芳1,梁芙萌2,李楠3,王晓晓3,韩江莉1,*( ),郭丽君1,*(
),郭丽君1,*( )
)
- 1. 北京大学第三医院心内科、血管医学研究所,血管稳态与重构全国重点实验室,国家卫生健康委员会心血管分子生物学与调节肽重点实验室,心血管受体研究北京市重点实验室,北京 100191
2. 北京大学第三医院北方院区综合内科,北京 100089
3. 北京大学第三医院临床流行病学研究中心,北京 100191
Index of microcirculatory resistance is associated with left ventricular remodeling in patients with acute anterior ST-segment elevation myocardial infarction undergoing emergency primary percutaneous coronary intervention
Fangfang WANG1,Fumeng LIANG2,Nan LI3,Xiaoxiao WANG3,Jiangli HAN1,*( ),Lijun GUO1,*(
),Lijun GUO1,*( )
)
- 1. Department of Cardiology and Institute of Vascular Medicine, Peking University Third Hospital; State Key Laboratory of Vascular Homeostasis and Remodeling, Peking University; NHC Key Laboratory of Cardiovascular Molecular Biology and Regulatory Peptides, Peking University; Beijing Key Laboratory of Cardiovascular Receptors Research, Beijing 100191, China
2. Department of General Medicine, Peking University Third Hospital, Beifang Branch, Beijing 100089, China
3. Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
摘要:
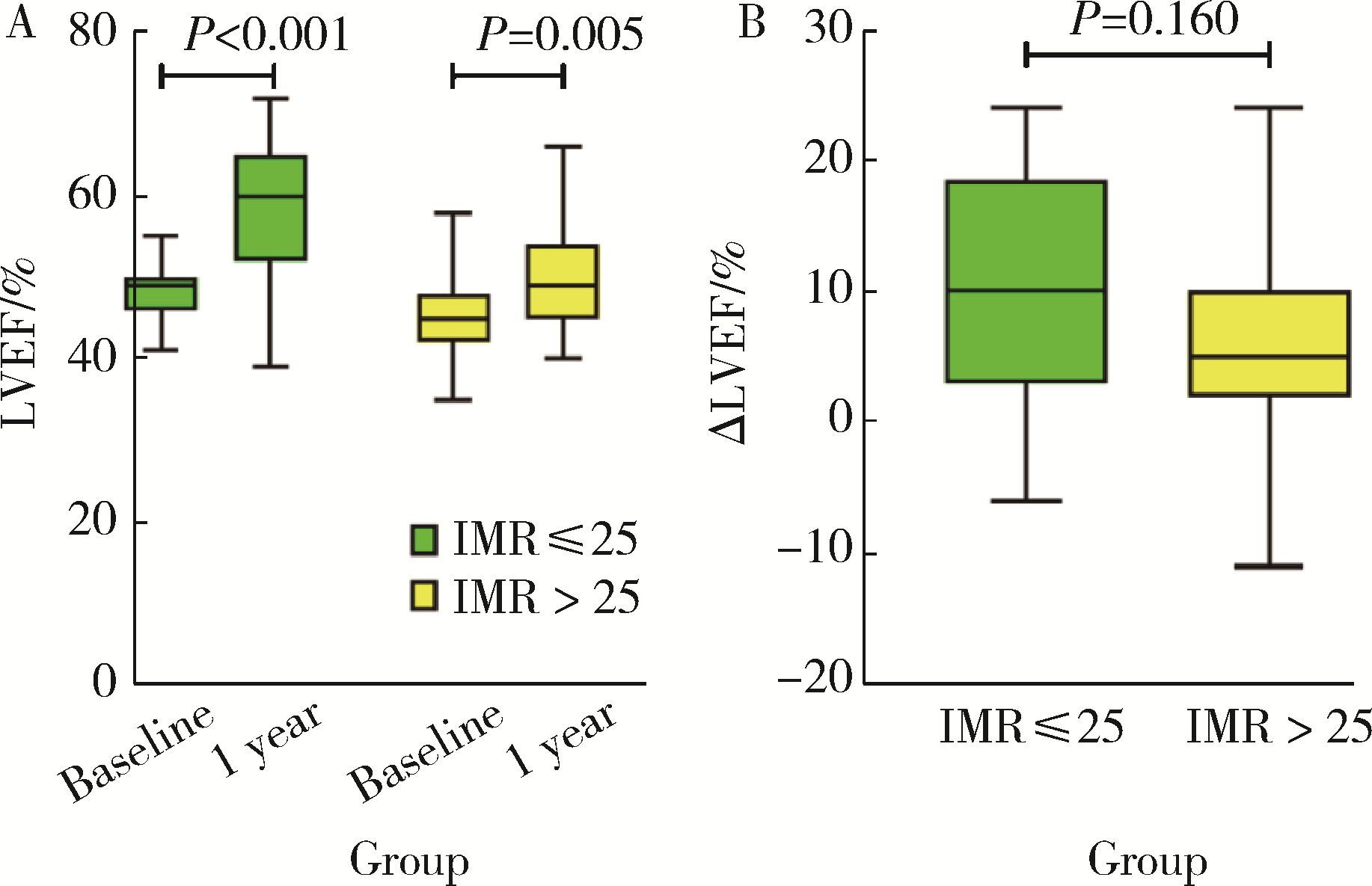
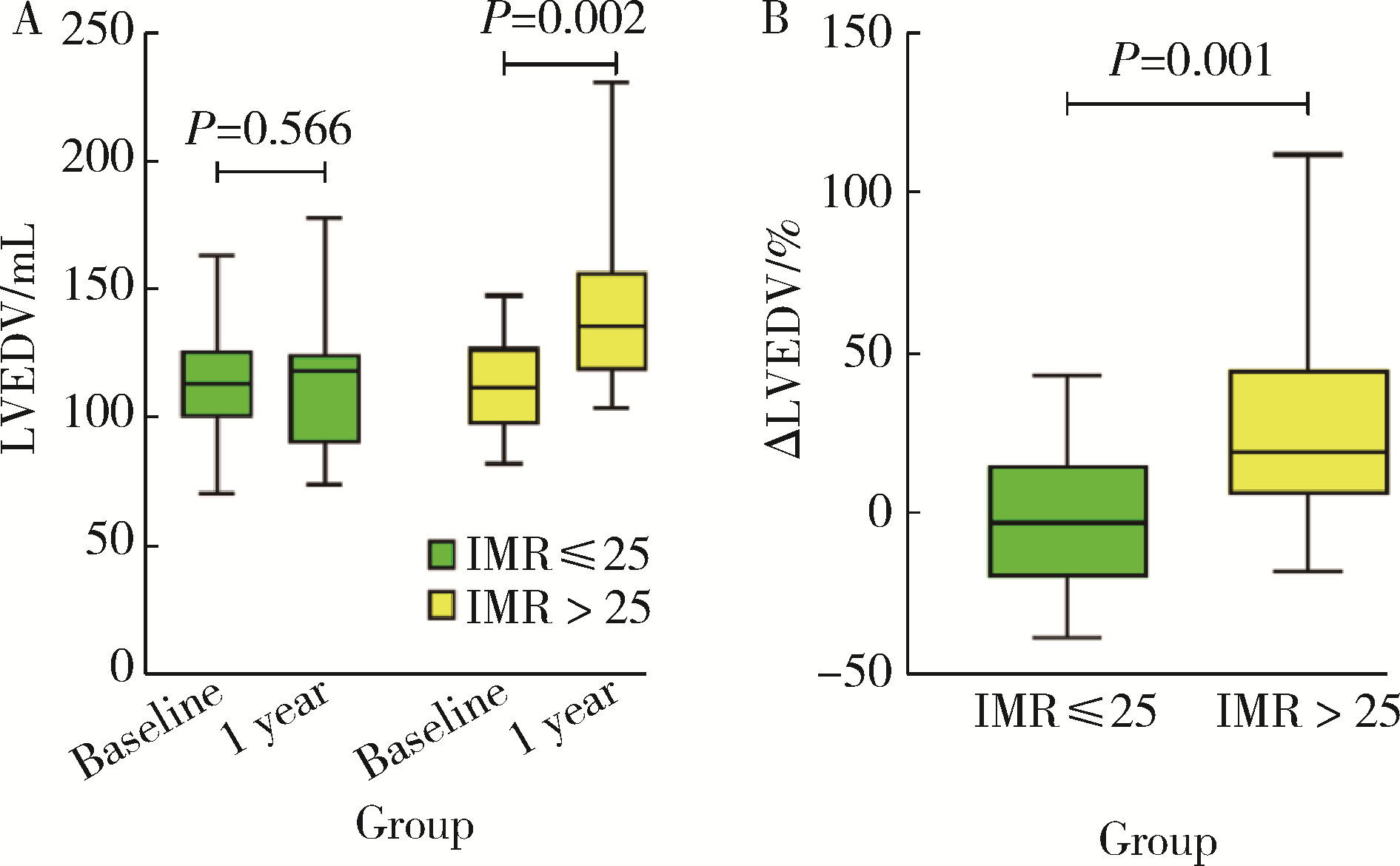
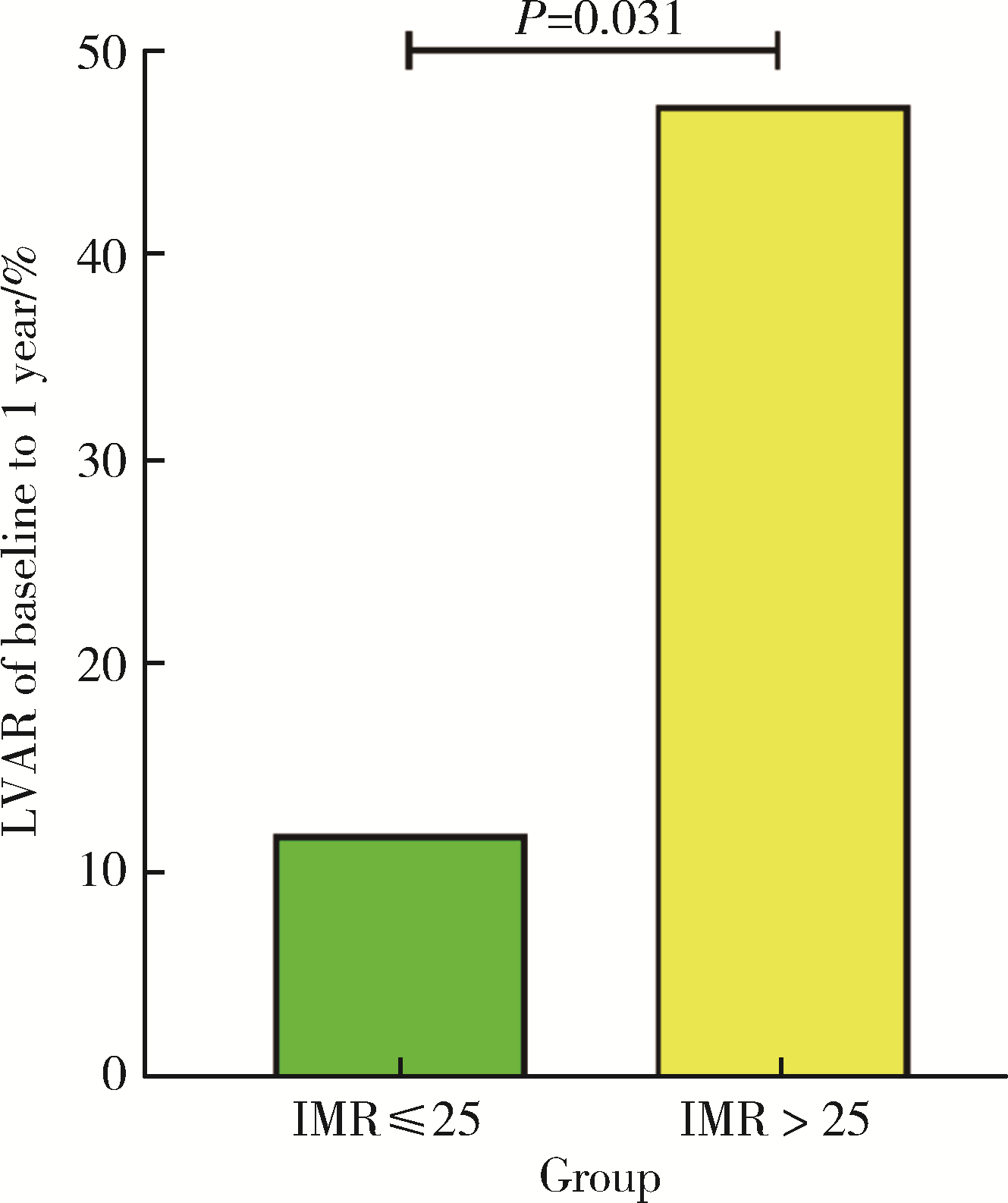
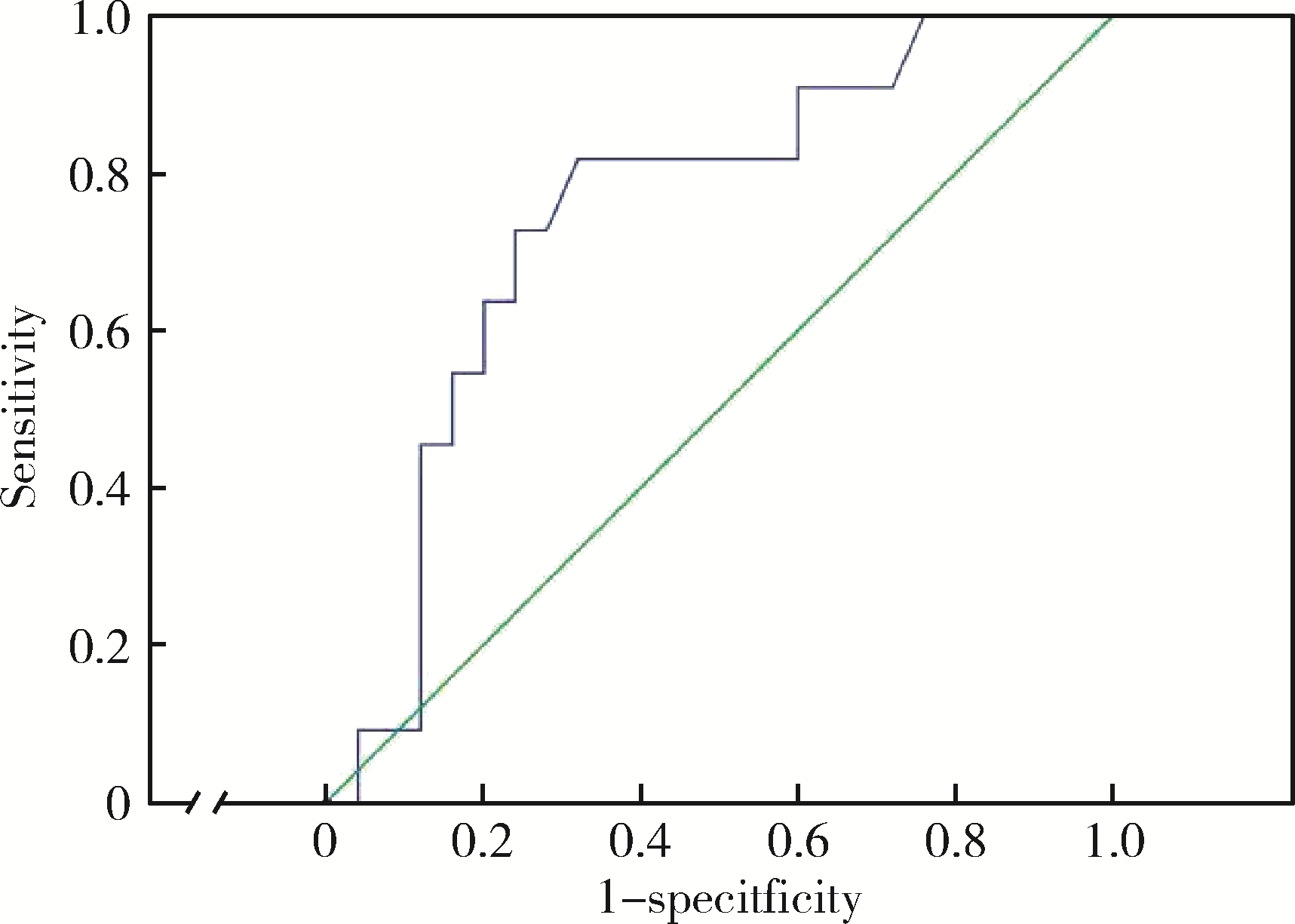
目的: 评估急性前壁ST段抬高心肌梗死(acute anterior ST elevation myocardial infarction,STEMI)患者直接经皮冠状动脉介入术(primary percutaneous coronary intervention,PPCI)后微循环阻力指数(index of microcirculatory resistance,IMR)与1年后左心室不良重构(left ventricular adverse remodeling,LVAR)之间的关系。方法: 采用单中心回顾性队列研究,连续选择2014年1月至2017年8月在北京大学第三医院住院的前壁STEMI并行PPCI患者,术后即刻通过压力/温度导丝测量IMR。利用血清肌酸激酶(creatine kinase,CK)峰值评估梗死面积,心肌梗死(myocardial infarction,MI)后1 d和1年时评估超声心动图,将左心室舒张末期容积(left ventricular end-diastolic volume,LVEDV)较基线增加≥20%定义为LVAR。结果: 共入选43例患者,平均年龄(58.7±12.4)岁。根据IMR正常参考值将患者分为两组,IMR>25(n=23)组较IMR≤25组(n=20)患者冠状动脉造影显示梗死相关血管完全闭塞率(95.7% vs. 65.0%, P=0.029)更高,血清CK峰值水平更高[4 090(383, 15 833)vs. 1 580(396, 5 583), P=0.004],室壁瘤发生率更高(30.4% vs. 5.0%,P=0.021)。MI后1 d两组LVEDV差异无统计学意义[(111.0±18.8) mL vs. (115.0±23.6) mL,P=0.503],而1年后IMR>25组LVEDV明显高于IMR≤25组[(141.5±33.7) mL vs. (115.9±27.9) mL, P=0.018]。IMR>25组LVAR发生比例更高(47.4% vs. 11.8%, P=0.024)。二元Logistics回归显示IMR[B=0.079,exp(B) (95%CI) 为1.082 (1.018~1.149), P=0.011]和血清甘油三酯(triglyceride,TG)水平[B=1.610,exp(B) (95%CI)为5.005 (1.380~18.152), P=0.014]是患者MI后1年发生LVAR的预测因素,IMR对1年后发生LVAR具有良好的预测价值(曲线下面积=0.749, P=0.019),IMR>29为良好的临界点,敏感性81.8%,特异性68.0%。结论: STEMI患者PPCI术后即刻测定IMR可以反映微血管功能,而微血管功能障碍是STEMI后1年左心室不良重构的有力预测指标。
中图分类号:
- R542.22
| 1 | Klancik V , Pesl L , Neuberg M , et al. Long-term follow-up in patients with ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention[J]. Eur Heart J Suppl, 2022, 24 (Suppl B): B16- B22. |
| 2 |
Araszkiewicz A , Grajek S , Lesiak M , et al. Effect of impaired myocardial reperfusion on left ventricular remodeling in patients with anterior wall acute myocardial infarction treated with primary coronary intervention[J]. Am J Cardiol, 2006, 98 (6): 725- 728.
doi: 10.1016/j.amjcard.2006.04.009 |
| 3 |
杨洋, 李楠, 赖红梅, 等. 急性前壁ST段抬高型心肌梗死患者介入治疗前血清血管内皮生长因子与左心室重构的关联性研究[J]. 中国心血管病研究, 2021, 19 (9): 818- 823.
doi: 10.3969/j.issn.1672-5301.2021.09.012 |
| 4 |
van der Bijl P , Abou R , Goedemans L , et al. Left ventricular post-infarct remodeling: Implications for systolic function improvement and outcomes in the modern era[J]. JACC Heart Fail, 2020, 8 (2): 131- 140.
doi: 10.1016/j.jchf.2019.08.014 |
| 5 |
Ng MK , Yong AS , Ho M , et al. The index of microcirculatory resistance predicts myocardial infarction related to percutaneous coronary intervention[J]. Circ Cardiovasc Interv, 2012, 5 (4): 515- 522.
doi: 10.1161/CIRCINTERVENTIONS.112.969048 |
| 6 |
Yoon GS , Ahn SG , Woo SI , et al. The Index of Microcirculatory resistance after primary percutaneous coronary intervention predicts long-term clinical outcomes in patients with ST-segment elevation myocardial infarction[J]. J Clin Med, 2021, 10 (20): 4752.
doi: 10.3390/jcm10204752 |
| 7 |
Qi Y , Gu R , Xu J , et al. Index of microcirculatory resistance predicts long term cardiac systolic function in patients with STEMI undergoing primary PCI[J]. BMC Cardiovasc Disord, 2021, 21 (1): 66.
doi: 10.1186/s12872-021-01887-w |
| 8 |
Fearon WF , Low AF , Yong AS , et al. Prognostic value of the index of microcirculatory resistance measured after primary percutaneous coronary intervention[J]. Circulation, 2013, 127 (24): 2436- 2441.
doi: 10.1161/CIRCULATIONAHA.112.000298 |
| 9 |
韩江莉, 何立芸, 崔鸣, 等. 急性心肌梗死直接冠状动脉介入治疗患者微循环阻力指数检测的可行性及临床价值探讨[J]. 中华医学杂志, 2017, 97 (29): 2261- 2265.
doi: 10.3760/cma.j.issn.0376-2491.2017.29.006 |
| 10 |
Akasaka T , Yoshida K , Kawamoto T , et al. Relation of phasic coronary flow velocity characteristics with TIMI perfusion grade and myocardial recovery after primary percutaneous transluminal coronary angioplasty and rescue stenting[J]. Circulation, 2000, 101 (20): 2361- 2367.
doi: 10.1161/01.CIR.101.20.2361 |
| 11 |
Ng MK , Yeung AC , Fearon WF . Invasive assessment of the coronary microcirculation: Superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve[J]. Circulation, 2006, 113 (17): 2054- 2061.
doi: 10.1161/CIRCULATIONAHA.105.603522 |
| 12 |
Fearon WF , Balsam LB , Farouque HM , et al. Novel index for invasively assessing the coronary microcirculation[J]. Circulation, 2003, 107 (25): 3129- 3132.
doi: 10.1161/01.CIR.0000080700.98607.D1 |
| 13 |
Aarnoudse W , Fearon WF , Manoharan G , et al. Epicardial stenosis severity does not affect minimal microcirculatory resistance[J]. Circulation, 2004, 110 (15): 2137- 2142.
doi: 10.1161/01.CIR.0000143893.18451.0E |
| 14 |
Berry C , Corcoran D , Hennigan B , et al. Fractional flow reserve-guided management in stable coronary disease and acute myocardial infarction: Recent developments[J]. Eur Heart J, 2015, 36 (45): 3155- 3164.
doi: 10.1093/eurheartj/ehv206 |
| 15 |
van Kranenburg M , Magro M , Thiele H , et al. Prognostic value of microvascular obstruction and infarct size, as measured by CMR in STEMI patients[J]. JACC Cardiovasc Imaging, 2014, 7 (9): 930- 939.
doi: 10.1016/j.jcmg.2014.05.010 |
| 16 |
Maznyczka AM , McCartney PJ , Oldroyd KG , et al. Risk stratification guided by the index of microcirculatory resistance and left ventricular end-diastolic pressure in acute myocardial infarction[J]. Circ Cardiovasc Interv, 2021, 14 (2): e009529.
doi: 10.1161/CIRCINTERVENTIONS.120.009529 |
| 17 |
Lim HS , Yoon MH , Tahk SJ , et al. Usefulness of the index of microcirculatory resistance for invasively assessing myocardial viability immediately after primary angioplasty for anterior myocardial infarction[J]. Eur Heart J, 2009, 30 (23): 2854- 2860.
doi: 10.1093/eurheartj/ehp313 |
| 18 |
Bolognese L , Neskovic AN , Parodi G , et al. Left ventricular remodeling after primary coronary angioplasty: Patterns of left ventricular dilation and long-term prognostic implications[J]. Circulation, 2002, 106 (18): 2351- 2357.
doi: 10.1161/01.CIR.0000036014.90197.FA |
| 19 |
Shi K , Ma M , Yang MX , et al. Increased oxygenation is associated with myocardial inflammation and adverse regional remodeling after acute ST-segment elevation myocardial Infarction[J]. Eur Radiol, 2021, 31 (12): 8956- 8966.
doi: 10.1007/s00330-021-08032-3 |
| 20 |
Luo E , Wang D , Yan G , et al. High triglyceride-glucose index is associated with poor prognosis in patients with acute ST-elevation myocardial infarction after percutaneous coronary intervention[J]. Cardiovasc Diabetol, 2019, 18 (1): 150.
doi: 10.1186/s12933-019-0957-3 |
| 21 |
Garg M , Khanna D , Kalra S , et al. Chronic oral administration of low-dose combination of fenofibrate and rosuvastatin protects the rat heart against experimentally induced acute myocardial infarction[J]. Fundam Clin Pharmacol, 2016, 30 (5): 394- 405.
doi: 10.1111/fcp.12204 |
| 22 | Oidor-Chan VH , Hong E , Perez-Severiano F , et al. Fenofibrate plus metformin produces cardioprotection in a type 2 diabetes and acute myocardial infarction model[J]. PPAR Res, 2016, 2016, 8237264. |
| 23 |
Niccoli G , Scalone G , Lerman A , et al. Coronary microvascular obstruction in acute myocardial infarction[J]. Eur Heart J, 2016, 37 (13): 1024- 1033.
doi: 10.1093/eurheartj/ehv484 |
| 24 |
Ishida K , Geshi T , Nakano A , et al. Beneficial effects of statin treatment on coronary microvascular dysfunction and left ventricular remodeling in patients with acute myocardial infarction[J]. Int J Cardiol, 2012, 155 (3): 442- 447.
doi: 10.1016/j.ijcard.2011.11.015 |
| 25 | Węgiel M , Rakowski T . Circulating biomarkers as predictors of left ventricular remodeling after myocardial infarction[J]. Adv interv cardiol, 2021, 17 (1): 21- 32. |
| [1] | 郑生旗,花天池,殷桂草,张伟,姚曳,李一帆. 甘油三酯葡萄糖指数与男性肾结石风险的关联[J]. 北京大学学报(医学版), 2024, 56(4): 610-616. |
| [2] | 郭煌达,彭和香,王斯悦,侯天姣,李奕昕,章涵宇,王梦莹,武轶群,秦雪英,唐迅,李劲,陈大方,胡永华,吴涛. 短期大气颗粒物暴露和MTNR1B基因多态性对甘油三酯-葡萄糖指数影响的家系研究[J]. 北京大学学报(医学版), 2024, 56(3): 375-383. |
| [3] | 高卿,陈彧,刘刚,陈生龙,董穗欣. 心肌梗死后室间隔穿孔:非选择性病例的外科临床结果[J]. 北京大学学报(医学版), 2019, 51(6): 1103-1107. |
| [4] | 李传凤, 李军, 白鹏, 吕愈敏. 结直肠腺瘤与患者血脂代谢水平[J]. 北京大学学报(医学版), 2011, 43(3): 432-435. |
| [5] | 李丽君, 陈红, 任景怡, 王岚, 罗宇. 微粒化非诺贝特对高脂血症患者血脂及尿酸代谢的影响[J]. 北京大学学报(医学版), 2009, 41(5): 541-544. |
| [6] | 段晋瑜, 欧阳翔英, 周于翔. 中、重度慢性牙周炎伴高血脂患者在牙周基础治疗后血脂的变化[J]. 北京大学学报(医学版), 2009, 41(1): 36-39. |
|
||