北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (5): 961-966. doi: 10.19723/j.issn.1671-167X.2025.05.022
腹腔镜下膀胱癌根治术同期行肾输尿管全长切除术的预后分析
李慎谟1,2,*, 苏丹丹1,*, 林己煜1,3, 宋昊东1,3, 马潞林1, 侯小飞1, 王国良1, 张洪宪1, 叶剑飞1,*( ), 张树栋1,*(
), 张树栋1,*( )
)
- 1. 北京大学第三医院泌尿外科, 北京 100191
2. 郑州人民医院泌尿外科, 郑州 450002
3. 北京大学基础医学院临床医学专业, 北京 100191
Prognostic analysis of laparoscopic simultaneous radical cystectomy and nephroureterectomy
Shenmo LI1,2, Dandan SU1, Jiyu LIN1,3, Haodong SONG1,3, Lulin MA1, Xiaofei HOU1, Guoliang WANG1, Hongxian ZHANG1, Jianfei YE1,*( ), Shudong ZHANG1,*(
), Shudong ZHANG1,*( )
)
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Department of Urology, Zhengzhou People's Hospital, Zhengzhou 450002, China
3. Department of Clinical Medicine, Peking University School of Basic Medical Sciences, Beijing 100191, China
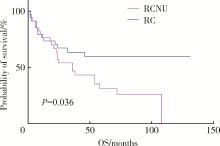
摘要: 目的: 探讨腹腔镜下膀胱癌根治术同期行单侧肾输尿管全长切除术(radical cystectomy and nephrourete-rectomy, RCNU)治疗上尿路尿路上皮癌合并膀胱癌的安全性及预后影响因素。方法: 回顾性分析2009年1月至2023年9月, 北京大学第三医院收治并行腹腔镜下RCNU手术患者的临床资料。根据相同性别、年龄(±5岁)、既往尿路上皮肿瘤病史、基础疾病、T分期、N分期、M分期、美国麻醉医师协会(American Society of Anesthesiologists, ASA)评分、Charlson合并症指数和体重指数(body mass index, BMI)(±5)等指标情况, 将34例RCNU患者与单独接受腹腔镜下膀胱癌根治术(radical cystectomy, RC)的膀胱癌患者进行1 ∶1人工匹配。采用Kaplan-Meier生存分析法计算患者的生存率, 应用Cox比例回归风险模型分析影响预后的临床因素。结果: 组的68例患者中, 随访率100%, 中位随访时间27.0(11.7, 60.2)个月。两组患者术中情况(包括手术时间、术中估计出血量、术中输血量等)的对比差异均无统计学意义(P>0.05)。两组患者术前肌酐和术后肌酐的差异均有统计学意义(P < 0.05)。RC组围术期Clavien Ⅲ~Ⅳ级并发症的发生率为2.9%(1/34), RCNU组为5.9%(2/34), 两组患者的围术期并发症发生率差异无统计学意义。与单独接受RC的匹配组相比, 接受RCNU的患者总生存期显著降低(P < 0.05)。Cox回归分析提示, N分期高、术后肌酐高这两个因素是影响患者预后的独立危险因素(P < 0.05)。结论: 同期行单侧RCNU手术与单纯行腹腔镜下RC手术的患者相比, 手术时间、术中出血量以及围术期并发症等方面临床上未见显著差异, 但术前肾功能和术后肾功能的差异均有统计学意义, RCNU手术患者比单纯RC手术患者的生存预后更差。
中图分类号:
- R737.1
| 1 |
doi: 10.1016/j.eururo.2023.03.013 |
| 2 |
doi: 10.1186/s12894-019-0457-5 |
| 3 |
doi: 10.1007/s00432-014-1585-7 |
| 4 |
doi: 10.1038/srep18014 |
| 5 |
doi: 10.1016/j.urolonc.2021.03.002 |
| 6 |
doi: 10.1016/j.urology.2022.09.039 |
| 7 |
doi: 10.1111/ases.12989 |
| 8 |
doi: 10.1016/j.eururo.2014.12.007 |
| 9 |
doi: 10.1016/S0140-6736(18)30996-6 |
| 10 |
doi: 10.1186/s12894-021-00839-y |
| 11 |
doi: 10.1016/j.urology.2022.08.064 |
| [1] | 缪祺, 洪保安, 张学舟, 孙志鹏, 王维, 王宇轩, 薄予轩, 赵佳晖, 张宁. 膀胱癌合并冠心病患者行经尿道膀胱肿瘤切除术围手术期抗血小板药物管理[J]. 北京大学学报(医学版), 2025, 57(4): 698-703. |
| [2] | 刘欢锐,彭祥,李森林,苟欣. 基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估[J]. 北京大学学报(医学版), 2023, 55(5): 793-801. |
| [3] | 张崔建,何志嵩,周利群. 上尿路尿路上皮癌的淋巴清扫[J]. 北京大学学报(医学版), 2022, 54(4): 592-594. |
| [4] | 戴翔,王飞,杜依青,宋宇轩,徐涛. 上尿路尿路上皮癌组织中脂肪因子表达与临床病理特征及预后的相关性[J]. 北京大学学报(医学版), 2022, 54(4): 605-614. |
| [5] | 李志华,徐纯如,刘颖,贯华,张萌,车新艳,唐琦,黄燕波,李学松,周利群. 饮水习惯与上尿路尿路上皮癌病理特征的相关性分析[J]. 北京大学学报(医学版), 2022, 54(4): 621-627. |
| [6] | 王飞,秦彩朋,杜依青,刘士军,李清,徐涛. 中危非肌层浸润性膀胱癌的最佳膀胱镜监测强度[J]. 北京大学学报(医学版), 2022, 54(4): 669-673. |
| [7] | 关豹,翁迈,凡航,彭鼎,方冬,熊耕砚,李学松,周利群. 术前贫血对上尿路尿路上皮癌预后的影响: 单中心686例患者回顾性研究[J]. 北京大学学报(医学版), 2019, 51(6): 1056-1061. |
| [8] | 黄海文,闫兵,尚美霞,刘漓波,郝瀚,席志军. 女性膀胱癌患者腹腔镜膀胱全切术与开放膀胱全切术的倾向性评分匹配比较[J]. 北京大学学报(医学版), 2019, 51(4): 698-705. |
| [9] | 马闰卓,夏海缀,陆敏,张智荧,张启鸣,卢剑,王国良,马潞林. 输尿管镜活体组织检查对上尿路尿路上皮癌根治性手术的影响[J]. 北京大学学报(医学版), 2019, 51(4): 665-672. |
| [10] | 杨飞龙,洪锴,赵国江,刘承,宋一萌,马潞林. 基于长链非编码RNA的生物信息学分析构建膀胱癌预后模型并确定预后生物标志物[J]. 北京大学学报(医学版), 2019, 51(4): 615-622. |
| [11] | 覃子健,毕海,马潞林,黄毅,张帆. 肠代膀胱内原发肠源性腺癌1例[J]. 北京大学学报(医学版), 2018, 50(4): 737-739. |
| [12] | 唐兴国,颜野,邱敏,卢剑,陆敏,侯小飞,黄毅,马潞林. 单中心16年青年膀胱尿路上皮癌患者的诊治[J]. 北京大学学报(医学版), 2018, 50(4): 630-633. |
| [13] | 关豹,曹振朋,彭鼎,李一帆,詹永豪,刘漓波,何世明,熊耕砚,李学松,周利群. T2N0M0期上尿路尿路上皮癌患者预后相关因素分析:单中心235例患者回顾性研究[J]. 北京大学学报(医学版), 2017, 49(4): 603-607. |
| [14] | 鲍正清,方冬,岳才博,蔡林,王天昱,李学松,周利群. 原发性阴茎阴囊Paget病22例临床分析[J]. 北京大学学报(医学版), 2016, 48(4): 638-642. |
| [15] | 叶海云,许清泉,黄晓波,马凯,王晓峰. 卡介苗膀胱灌注治疗致结核性前列腺脓肿1例[J]. 北京大学学报(医学版), 2015, 47(6): 1039-1041. |
|
||