Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (2): 275-280. doi: 10.19723/j.issn.1671-167X.2020.02.013
Previous Articles Next Articles
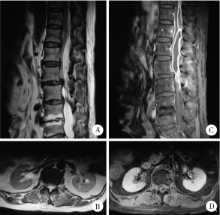
Diagnosis and treatment of primary intraspinal abscess
Chang-cheng MA,Zhen-yu WANG( ),Guo-zhong LIN
),Guo-zhong LIN
- Department of Neurosurgery, Peking University Third Hospital, Beijing, 100191, China
CLC Number:
- R632.5
| [1] | Honig A, Or O, Barzilay Y , et al. Spinal epidural abscess with a rapid course in young healthy infantry recruits with multiple skin lacerations[J]. J Clin Neurosci, 2016,31:127-132. |
| [2] | Reihsaus E, Waldbaur H, Seeling W . Spinal epidural abscess: a meta-analysis of 915 patients[J]. Neurosurg Rev, 2000,23(4):175-205. |
| [3] | Ersahin Y . Spinal epidural abscess: a meta-analysis of 915 patients[J]. Neurosurg Rev, 2001,24(2/3):156. |
| [4] | Karikari IO, Powers CJ, Reynolds RM , et al. Management of a spontaneous spinal epidural abscess: a single-center 10-year experience[J]. Neurosurgery, 2009,65(5):919-924. |
| [5] | Bartels RH, de Jong TR, Grotenhuis JA . Spinal subdural abscess[J]. J Neurosurg, 1992,76(2):307-311. |
| [6] | Kirzner H, Oh YK, Lee SH . Intraspinal air: a CT finding of epidural abscess[J]. Am J Roentgenol, 1988,151(6):1217-1218. |
| [7] | Farber SH, Murphy KR, Suryadevara CM , et al. Comparing outcomes of early, late, and non-surgical management of intraspinal abscess[J]. J Clin Neurosci, 2017,36:64-71. |
| [8] | Kulkarni AG, Chu G, Fehlings MG . Pyogenic intradural abscess: a case report[J]. Spine, 2007,32(12):E354-E357. |
| [9] | Thomé C, Krauss JK, Zevgaridis D , et al. Pyogenic abscess of the filum terminale. Case report[J]. J Neurosurg, 2001,95(Suppl 1):100-104. |
| [10] | Darouiche RO . Spinal epidural absces[J]. N Engl J Med, 2006,355(19):2012-2020. |
| [11] | Hanci M, Sarioglu AC, Uzan M , et al. Intramedullary tuberculous abscess: a case report[J]. Spine, 1996,21(6):766-769. |
| [12] | Bingöl A, Yücemen N, Meço O . Medically treated intraspinal "Brucella" granuloma[J]. Surg Neurol, 1999,52(6):570-576. |
| [13] | Kamat AS, Thango NS, Husein MB . Proteus mirabilis abscess involving the entire neural axis[J]. J Clin Neurosci, 2016,30:127-129. |
| [14] | Al Barbarawi M, Khriesat W, Qudsieh S , et al. Management of intramedullary spinal cord abscess: experience with four cases, pathophysiology and outcomes[J]. Eur Spine J, 2009,18(5):710-717. |
| [15] | Hindy J, Shelef I, Slovik Y , et al. Late prevertebral and spinal abscess following chemoradiation for laryngeal squamous cell carcinoma[J]. Case Rep Otolaryngol, 2014,2014:425724. |
| [16] | Miyazaki M, Yoshiiwa T, Kodera R , et al. Clinical features of cervical pyogenic spondylitis and intraspinal abscess[J]. J Spinal Disord Tech, 2011,24(7):E57-E61. |
| [17] | Ur-rahman N, El-bakry A, Jamjoom AB , et al. Atypical forms of spinal tuberculosis: case report and review of the literature[J]. Surg Neurol, 1999,51(6):602-607. |
| [18] | Khalil JG, Nassr A, Diehn FE , et al. Thoracolumbosacral spinal subdural abscess: magnetic resonance imaging appearance and limited surgical management[J]. Spine, 2013,38(13):E844-E847. |
| [19] | Narlawar RS, Shah JR, Pimple MK , et al. Isolated tuberculosis of posterior elements of spine: magnetic resonance imaging findings in 33 patients[J]. Spine, 2002,27(3):275-281. |
| [20] | Tanriverdi T, Kizilkiliç O, Hanci M , et al. Atypical intradural spinal tuberculosis: report of three cases[J]. Spinal Cord, 2003,41(7):403-409. |
| [21] | Hung PC, Wang HS, Wu CT , et al. Spinal intramedullary abscess with an epidermoid secondary to a dermal sinus[J]. Pediatr Neurol, 2007,37(2):144-147. |
| [22] | ter Avest E, Uyttenboogaart M, Dorgelo J , et al. A patient with neck pain and fever. Combined prevertebral and intraspinal abscess in a patient with a de novo HIV infection[J]. Neth J Med, 2009,67(10):356-357. |
| [23] | Vajramani GV, Nagmoti MB, Patil CS . Neurobrucellosis presenting as an intramedullary spinal cord abscess[J]. Ann Clin Microbiol Antimicrob, 2005,16(4):14. |
| [24] | Dev R, Husain M, Gupta A , et al. MR of multiple intraspinal abscesses associated with congenital dermal sinus[J]. Am J Neuroradiol, 1997,18(4):742-743. |
| [25] | Nagar VR, Springer JE, Salles S . Increased incidence of spinal abscess and substance abuse after implementation of state mandated prescription drug legislation[J]. Pain Med, 2015,16(10):2031-2035. |
| [26] | Singh I, Rohilla S, Kumar P , et al. Spinal dorsal dermal sinus tract: An experience of 21 cases[J]. Surg Neurol Int, 2015,6(Suppl 17):S429-434. |
| [1] | Le YU,Shaohui DENG,Fan ZHANG,Ye YAN,Jianfei YE,Shudong ZHANG. Clinicopathological characteristics and prognosis of multilocular cystic renal neoplasm of low malignant potential [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 661-666. |
| [2] | Kewei CHEN,Shaohui DENG,Zhuo LIU,Hongxian ZHANG,Lulin MA,Shudong ZHANG. Discussion on the surgical timing of rupture and hemorrhage of renal angiomyolipoma [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 326-331. |
| [3] | Silan AN,Qunyi ZHENG,Kai WANG,Shan GAO. Characteristics and influencing factors of early pain in patients after total knee arthroplasty [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 167-173. |
| [4] | Xiaomeng REN,Kaiyi LI,Chunlei LI. Detection of molecular affecting sensitivity to local glucocorticoid therapy in oral lichen planus through transcriptome sequencing [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 32-38. |
| [5] | Li-fang WANG,Lian-jie SHI,Wu NING,Nai-shu GAO,Kuan-ting WANG. Sjögren's syndrome combined with cold agglutinin disease: A case report [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1130-1134. |
| [6] | Hai MAO,Fan ZHANG,Zhan-yi ZHANG,Ye YAN,Yi-chang HAO,Yi HUANG,Lu-lin MA,Hong-ling CHU,Shu-dong ZHANG. Predictive model of early urinary continence recovery based on prostate gland MRI parameters after laparoscopic radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 818-824. |
| [7] | Yue WEI,Xi LU,Jing ZHANG,Kun-peng LIU,Yong-jun WANG,Lan YAO. Effect of preoperative carbohydrates intake on the gastric volume and the risk of reflux aspiration in patients positioning in trendelenburg undergoing gynecological laparoscopic procedures [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 893-898. |
| [8] | Xin-ling ZHANG,Zhi-yu LIN,Yu-jie CHEN,Wen-fang DONG,Xin YANG. Plastic and reconstruction surgery for non-healing wound after posterior spinal surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 910-914. |
| [9] | Guo-zhong LIN,Jing-cheng XIE,Xiao-dong CHEN,Jun YANG. Classification and microsurgical treatment of primary tethered cord syndrome in adults [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 641-645. |
| [10] | Xi-yan PEI,Wen YANG,Xiang-ying OUYANG,Feng SUN. Comparison of clinical effects between periodontal endoscopy aiding subgingival debridement and flap surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 716-720. |
| [11] | Chao WU,Bin LIU,Jing-cheng XIE,Zhen-yu WANG,Chang-cheng MA,Jun YANG,Jian-jun SUN,Xiao-dong CHEN,Tao YU,Guo-zhong LIN,Yu SI,Yun-feng HAN,Su-hua CHEN,Xiao-liang YIN,Qian-quan MA,Mu-tian ZHENG,Lin ZENG. Reinforced radiculoplasty for the treatment of symptomatic sacral Tarlov cysts: A clinical analysis of 71 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 133-138. |
| [12] | Jing-cheng XIE,Xiao-dong CHEN,Jun YANG. Diagnosis and surgical treatment of tethered cord syndrome accompanied by congenital dermal sinus tract in adults [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1163-1166. |
| [13] | Le-qing CAO,Jing-rui ZHOU,Yu-hong CHEN,Huan CHEN,Wei HAN,Yao CHEN,Yuan-yuan ZHANG,Chen-hua YAN,Yi-fei CHENG,Xiao-dong MO,Hai-xia FU,Ting-ting HAN,Meng LV,Jun KONG,Yu-qian SUN,Yu WANG,Lan-ping XU,Xiao-hui ZHANG,Xiao-jun HUANG. Relationship between treatment and prognosis in patients with late-onset severe pneumonia after allogeneic hematopoietic stem cell transplantation [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1013-1020. |
| [14] | YUAN Chang-wei,WANG Ying-jin,ZHANG Shu-jie,SHEN Sheng-li,DUAN Hong-zhou. Clinical outcomes following microsurgery and endovascular embolization in the management of spinal dural arteriovenous fistula: A meta-analysis study [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 304-314. |
| [15] | WANG Wei,CAI Lin,GAO Ying,GUO Xiao-hui,ZHANG Jun-qing. Persistent and serious hyperkalemia after surgery of primary aldosteronism: A case report [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 376-380. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 385
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 1417
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||