Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (2): 396-401. doi: 10.19723/j.issn.1671-167X.2021.02.027
Previous Articles Next Articles
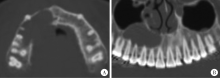
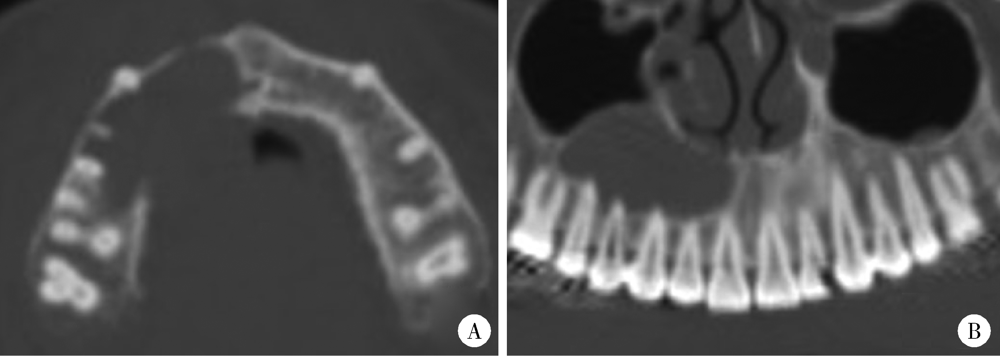
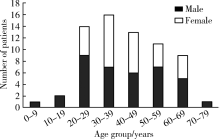
Three-dimentional radiographic features of 67 maxillary radicular cysts
MENG Yuan1,ZHANG Li-qi1,ZHAO Ya-ning1,LIU Deng-gao1,Δ( ),ZHANG Zu-yan1,GAO Yan2
),ZHANG Zu-yan1,GAO Yan2
- 1. Department of Oral and Maxillofacial Radiology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Department of Oral Pathology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R781.34
| [1] | White SC, Pharoah MJ. Oral radiology principles and interpretation[M]. 7th ed. Missouri: Mosby Inc., 2014. |
| [2] | Takata T, Slootweg PJ. Odontogenic and maxillofacial bone tumors[M] // El-Naggar AE, Chan JKC, Grandis JR, et al. WHO classification of head and neck tumors. 4th ed. Lyon: IARC, 2017: 203-260. |
| [3] | Kilinc A, Saruhan N, Gundogdu B, et al. Benign tumors and tumorlike lesions of the oral cavity and jaws: an analysis of 709 cases[J]. Niger J Clin Pract, 2017,20(1):1448-1454. |
| [4] | 张震康, 俞光岩. 口腔颌面外科学[M]. 2版. 北京: 北京大学医学出版社, 2013. |
| [5] | 马绪臣. 口腔颌面医学影像学[M]. 2版. 北京: 北京大学医学出版社, 2014. |
| [6] | 吴运堂. 口腔颌面骨疾病临床影像诊断学[M]. 北京: 北京大学医学出版社, 2005. |
| [7] |
Scarfe WC, Toghyani S, Azevedo B. Imaging of benign odontoge-nic lesions[J]. Radiol Clin North Am, 2018,56(1):45-62.
pmid: 29157548 |
| [8] |
Barros C, Santos HBP, Cavalcante IL, et al. Clinical and histopathological features of nasopalatine duct cyst: A 47-year retrospective study and review of current concepts[J]. J Craniomaxillofac Surg, 2018,46(2):264-268.
pmid: 29248496 |
| [9] |
Araujo JP, Lemos CA, Miniello TG, et al. The relevance of clinical and radiographic features of jaw lesions: a prospective study[J]. Braz Oral Res, 2016,30(1):e96-e104.
pmid: 27556683 |
| [10] |
Nunez-Urrutia S, Figueiredo R, Gay-Escoda C. Retrospective clinicopathological study of 418 odontogenic cysts[J]. Med Oral Patol Oral Cir Bucal, 2010,15(5):e767-e773.
pmid: 20383117 |
| [11] |
Chen JH, Tseng CH, Wang WC, et al. Clinicopathological analysis of 232 radicular cysts of the jawbone in a population of southern Taiwanese patients[J]. Kaohsiung J Med Sci, 2018,34(4):249-254.
doi: 10.1016/j.kjms.2018.01.011 pmid: 29655415 |
| [12] |
Gondak RO, Rocha AC, Neves Campos JG, et al. Unicystic ameloblastoma mimicking apical periodontitis: a case series[J]. J Endod, 2013,39(1):145-148.
doi: 10.1016/j.joen.2012.09.017 pmid: 23228275 |
| [13] | 高岩, 李铁军. 口腔组织学与病理学[M]. 2版. 北京: 北京大学医学出版社, 2013. |
| [14] |
Faitaroni LA, Bueno MR, Carvalhosa AA, et al. Differential diagnosis of apical periodontitis and nasopalatine duct cyst[J]. J Endod, 2011,37(3):403-410.
doi: 10.1016/j.joen.2010.11.022 pmid: 21329830 |
| [15] |
Omoregie FO, Sede MA, Ojo AM. Ameloblastomatous change in radicular cyst of the jaw in a Nigerian population[J]. Ghana Med J, 2015,49(2):107-111.
doi: 10.4314/gmj.v49i2.8 pmid: 26339095 |
| [16] | Mass E, Kaplan I, Hirshberg A. A clinical and histopathological study of radicular cysts associated with primary molars[J]. J Oral Pathol Med, 1995,24(1):458-461. |
| [17] |
Aboulhosn M, Noujeim Z, Nader N, et al. Decompression and enucleation of a mandibular radicular cyst, followed by bone regeneration and implant-supported dental restoration[J]. Case Rep Dent, 2019,2019:9584235.
doi: 10.1155/2019/9584235 pmid: 30729045 |
| [18] |
Pitcher B, Alaqla A, Noujeim M, et al. Binary decision trees for preoperative periapical cyst screening using cone-beam computed tomography[J]. J Endod, 2017,43(3):383-388.
doi: 10.1016/j.joen.2016.10.046 pmid: 28231977 |
| [19] | 孟圆, 张亚琼, 叶欣, 等. 上颌成釉细胞瘤、牙源性角化囊肿及含牙囊肿的螺旋CT和锥形束CT影像分析[J]. 中华口腔医学杂志, 2018,53(10):659-664. |
| [20] |
Guo J, Simon JH, Sedghizadeh P, et al. Evaluation of the reliability and accuracy of using cone-beam computed tomography for diagnosing periapical cysts from granulomas[J]. J Endod, 2013,39(12):1485-1490.
doi: 10.1016/j.joen.2013.08.019 pmid: 24238434 |
| [1] | Hua ZHONG, Yuan LI, Liling XU, Mingxin BAI, Yin SU. Application of 18F-FDG PET/CT in rheumatic diseases [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 853-859. |
| [2] | Shishi BO,Chengzhi GAO. Tooth segmentation and identification on cone-beam computed tomography with convolutional neural network based on spatial embedding information [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 735-740. |
| [3] | Xiaotong LING,Liuyang QU,Danni ZHENG,Jing YANG,Xuebing YAN,Denggao LIU,Yan GAO. Three-dimensional radiographic features of calcifying odontogenic cyst and calcifying epithelial odontogenic tumor [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 131-137. |
| [4] | Chen CHEN,Yuhong LIANG. Root canal therapy of maxillary molars with atypical canals: A report of three cases [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 190-195. |
| [5] | Sui LI,Wenjie MA,Shimin WANG,Qian DING,Yao SUN,Lei ZHANG. Trueness of different digital design methods for incisal guidance of maxillary anterior implant-supported single crowns [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 81-87. |
| [6] | Deng-hui DUAN,Hom-Lay WANG,En-bo WANG. Role of collagen membrane in modified guided bone regeneration surgery using buccal punch flap approach: A retrospective and radiographical cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1097-1104. |
| [7] | Xiang LIU,Hui-hui XIE,Yu-feng XU,Xiao-dong ZHANG,Xiao-feng TAO,Lin LIU,Xiao-ying WANG. Value of artificial intelligence in the improvement of diagnostic consistency of radiology residents [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 670-675. |
| [8] | Ying HUANG,Zhi-yuan WU,Xing-hong ZHOU,Zhi-gang CAI,Jie ZHANG. Category of facial symmetry perception after maxillary reconstruction using anterolateral thigh flap [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 708-715. |
| [9] | Jin-hua ZHANG,Jie PAN,Zhi-peng SUN,Xiao WANG. Effect of various intracanal materials on the diagnostic accuracy of cone-beam computed tomography in vertical root fractures [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 333-338. |
| [10] | Jia-xue YE,Yu-hong LIANG. A prevalence survey of cone-beam computed tomography use among endodontic practitioners [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 114-119. |
| [11] | Meng-qiao PAN,Jian LIU,Li XU,Xiao XU,Jian-xia HOU,Xiao-tong LI,Xiao-xia WANG. A long-term evaluation of periodontal phenotypes before and after the periodontal-orthodontic-orthognathic combined treatment of lower anterior teeth in patients with skeletal Angle class Ⅲ malocclusion [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 52-61. |
| [12] | Yu FU,Xin-nong HU,Sheng-jie CUI,Jie SHI. Decompensation effectiveness and alveolar bone remodeling analysis of mandibular anterior teeth after preoperative orthodontic treatment in high-angle patients with skeletal class Ⅱ malocclusion [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 62-69. |
| [13] | Yu WANG,Hui-min ZHANG,Xue-rong DENG,Wei-wei LIU,Lu CHEN,Ning ZHAO,Xiao-hui ZHANG,Zhi-bo SONG,Yan GENG,Lan-lan JI,Yu WANG,Zhuo-li ZHANG. Diagnostic values of urinary citrate for kidney stones in patients with primary gout [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1134-1140. |
| [14] | Juan GAO,Hang-miao LV,Hui-min MA,Yi-jiao ZHAO,Xiao-tong LI. Evaluation of root resorption after surgical orthodontic treatment of skeletal Class Ⅲ malocclusion by three-dimensional volumetric measurement with cone-beam CT [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 719-726. |
| [15] | WANG Shu-lei,GAO Yang-xu,ZHANG Hong-wu,YANG Hai-bo,LI Hui,LI Yu,SHEN Li-xue,YAO Hong-xin. Clinical analysis of 30 cases of basal ganglia germinoma in children [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 222-226. |
|
||