Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (4): 719-726. doi: 10.19723/j.issn.1671-167X.2022.04.022
Previous Articles Next Articles
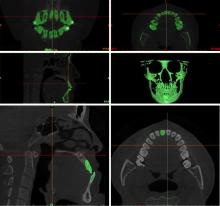
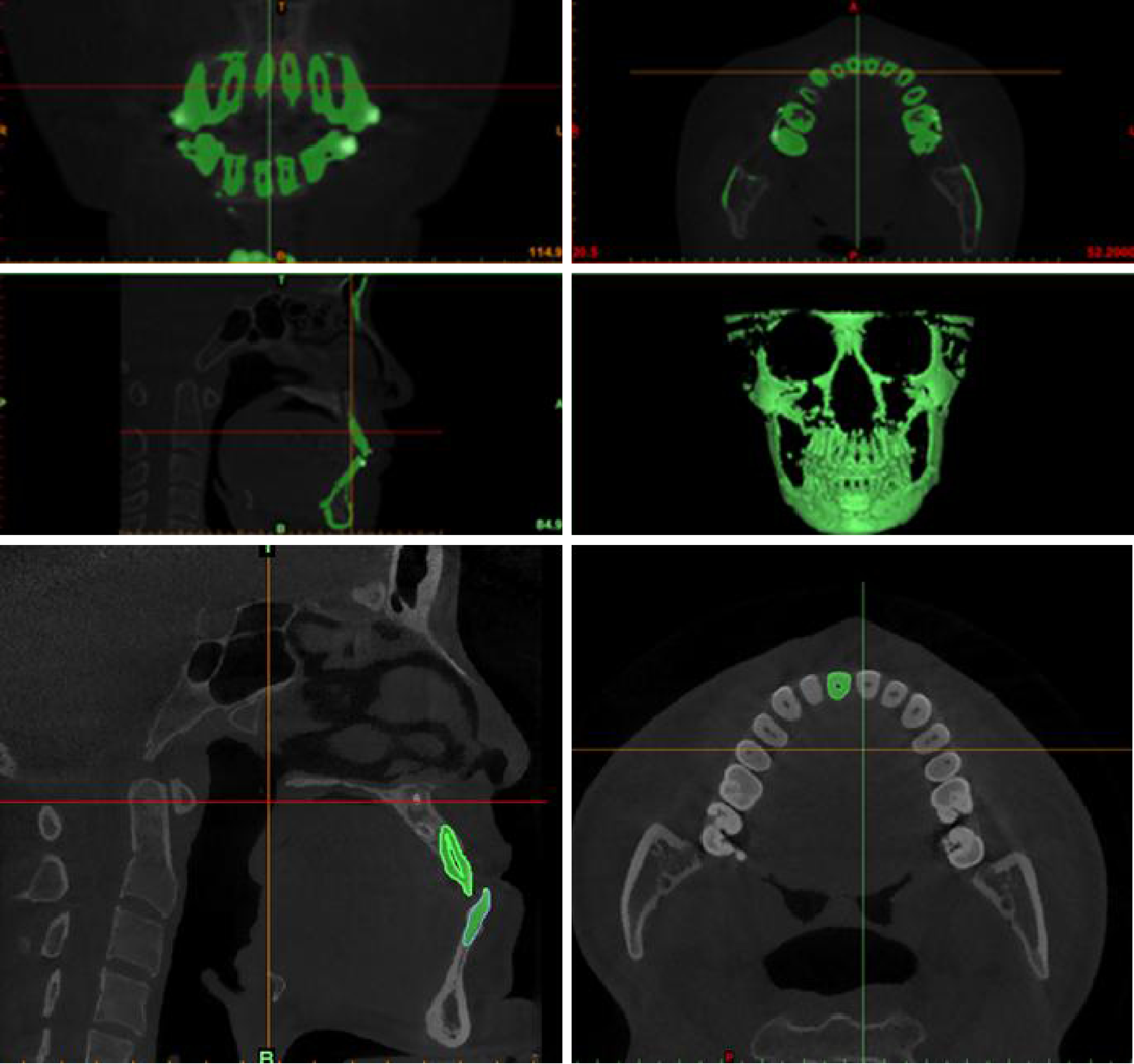
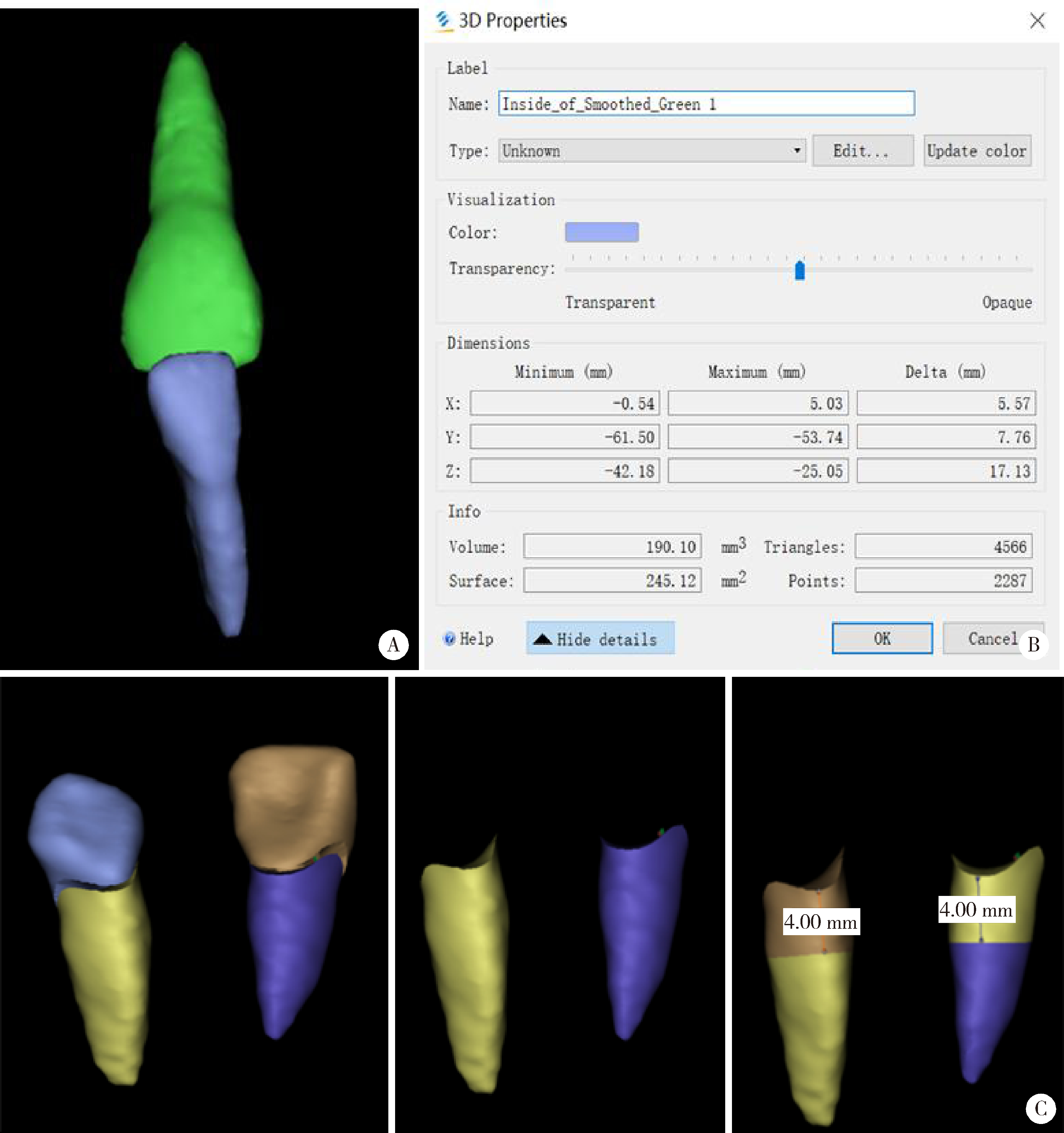
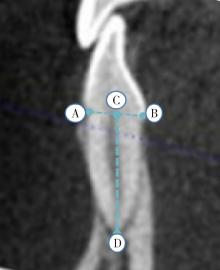
Evaluation of root resorption after surgical orthodontic treatment of skeletal Class Ⅲ malocclusion by three-dimensional volumetric measurement with cone-beam CT
Juan GAO1,2,Hang-miao LV1,Hui-min MA1,Yi-jiao ZHAO3,Xiao-tong LI1,*( )
)
- 1. Department of Orthodontics, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry, Beijing 100081, China
2. Department of Orthodontics, Guiyang Stomatological Hospital, Guiyang 550002, China
3. Digital Technology of Stomatology, Peking University School and Hospital of Stomatology, Beijing 100081, China
CLC Number:
- R783.5
| 1 |
Weltman B , Vig KW , Fields HW , et al. Root resorption associated with orthodontic tooth movement: A systematic review[J]. Am J Orthod Dentofacial Orthop, 2010, 137 (4): 462- 476.
doi: 10.1016/j.ajodo.2009.06.021 |
| 2 | 赵志河. 口腔正畸学[M]. 7版 北京: 人民卫生出版社, 2020. |
| 3 | Sawicka M , Bedini R , Pecci R , et al. The application of X-ray microtomography for the assessement of root resorption caused by the orthodontic treatment of premolars[J]. Ann Ist Super Sanita, 2012, 48 (1): 71- 74. |
| 4 | Zahed Zahedani S , Oshagh M , Momeni Danaei S , et al. Roeinpeikar SMM: A comparison of apical root resorption in incisors after fixed orthodontic treatment with standard edgewise and straight wire (MBT) method[J]. J Dent Shiraz Univ Med Sci, 2013, 14 (3): 103- 110. |
| 5 |
Hodges RJ , Atchison KA , White SC . Impact of cone-beam computed tomography on orthodontic diagnosis and treatment planning[J]. Am J Orthod Dentofacial Orthop, 2013, 143 (5): 665- 674.
doi: 10.1016/j.ajodo.2012.12.011 |
| 6 |
张婕, 李小彤. 骨性安氏Ⅲ类手术患者前牙区的牙槽骨厚度[J]. 北京大学学报(医学版), 2016, 48 (1): 111- 115.
doi: 10.3969/j.issn.1671-167X.2016.01.020 |
| 7 |
Giudice AL , Quinzi V , Ronsivalle V , et al. Evaluation of imaging software accuracy for 3-dimensional analysis of the mandibular condyle. A comparative study using a surface-to-surface matching technique[J]. Int J Environ Res Public Health, 2020, 17 (13): 4789.
doi: 10.3390/ijerph17134789 |
| 8 |
Deng Y , Sun Y , Xu T . Evaluation of root resorption after comprehensive orthodontic treatment using cone beam computed tomography (CBCT): A meta-analysis[J]. BMC Oral Health, 2018, 18 (1): 116.
doi: 10.1186/s12903-018-0579-2 |
| 9 |
熊再道, 赵桂芝, 柯杰, 等. 上颌快速扩弓后牙根吸收变化的三维测量研究[J]. 实用口腔医学杂志, 2018, 34 (1): 65- 68.
doi: 10.3969/j.issn.1001-3733.2018.01.014 |
| 10 |
Yildirim M , Akin M . Comparison of root resorption after bone-borne and tooth-borne rapid maxillary expansion evaluated with the use of microtomography[J]. Am J Orthod Dentofacial Orthop, 2019, 155 (2): 182- 190.
doi: 10.1016/j.ajodo.2018.03.021 |
| 11 | Lo Giudice A , Galletti C , Gay-Escoda C , et al. CBCT assessment of radicular volume loss after rapid maxillary expansion: A syste-matic review[J]. J Clin Exp Dent, 2018, 10 (5): e484- e494. |
| 12 |
Puttaravuttiporn P , Wongsuwanlert M , Charoemratrote C , et al. Volumetric evaluation of root resorption on the upper incisors using cone beam computed tomography after 1 year of orthodontic treatment in adult patients with marginal bone loss[J]. Angle Orthod, 2018, 88 (6): 710- 718.
doi: 10.2319/121717-868.1 |
| 13 |
Aras I , Unal I , Huniler G , et al. Root resorption due to orthodontic treatment using self-ligating and conventional brackets: A cone-beam computed tomography study[J]. J Orofac Orthop, 2018, 79 (3): 181- 190.
doi: 10.1007/s00056-018-0133-5 |
| 14 |
Ma H , Li W , Xu L , et al. Morphometric evaluation of the alveolar bone around central incisors during surgical orthodontic treatment of high-angle skeletal Class Ⅲ malocclusions[J]. Orthod Craniofac Res, 2021, 24 (1): 87- 95.
doi: 10.1111/ocr.12408 |
| 15 |
Kook YA , Kim G , Kim Y . Comparison of alveolar bone loss around incisors in normal occlusion samples and surgical skeletal Class Ⅲ patients[J]. Angle Orthod, 2012, 82 (4): 645- 652.
doi: 10.2319/070111-424.1 |
| 16 |
吕航苗, 高娟, 马慧敏, 等. 锥束CT三维重建技术应用于骨性Ⅲ类错患者上前牙牙根吸收的研究[J]. 中华口腔正畸学杂志, 2020, 27 (3): 129- 133.
doi: 10.3760/cma.j.cn115797-20200407-20303 |
| 17 | 王芳, 王建国, 张锡忠. 成人骨性Ⅲ类错术前正畸后切牙牙根吸收的CBCT研究[J]. 天津医药, 2015, 43 (4): 390- 392. |
| 18 |
Suteerapongpun P , Sirabanchongkran S , Wattanachai T , et al. Root surface areas of maxillary permanent teeth in anterior normal overbite and anterior open bite assessed using cone-beam computed tomography[J]. Imaging Sci Dent, 2017, 47 (4): 241- 246.
doi: 10.5624/isd.2017.47.4.241 |
| 19 |
Bartley N , Türk T , Colak C , et al. Physical properties of root cementum: Part 17. Root resorption after the application of 2. 5° and 15° of buccal root torque for 4 weeks: A microcomputed tomography study[J]. Am J Orthod Dentofacial Orthop, 2011, 139 (4): e353- e360.
doi: 10.1016/j.ajodo.2010.01.033 |
| 20 |
Hohmann A , Wolfram U , Geiger M , et al. Periodontal ligament hydrostatic pressure with areas of root resorption after application of a continuous torque moment[J]. Angle Orthod, 2007, 77 (4): 653- 659.
doi: 10.2319/060806-234 |
| 21 |
Segal GR , Schiffman PH , Tuncay OC . Meta analysis of the treatment-related factors of external apical root resorption[J]. Orthod Craniofac Res, 2004, 7 (2): 71- 78.
doi: 10.1111/j.1601-6343.2004.00286.x |
| 22 |
Martins DR , Tibola D , Janson G , et al. Effects of intrusion combined with anterior retraction on apical root resorption[J]. Eur J Orthod, 2012, 34 (2): 170- 175.
doi: 10.1093/ejo/cjq178 |
| 23 |
Li X , Xu J , Yin Y , et al. Association between root resorption and tooth development: A quantitative clinical study[J]. Am J Orthod Dentofacial Orthop, 2020, 157 (5): 602- 610.
doi: 10.1016/j.ajodo.2019.11.011 |
| 24 | 马宁, 李巍然, 陈晓红, 等. 上切牙内收前后的牙根吸收研究[J]. 现代口腔医学杂志, 2015, 29 (6): 330- 334. |
|
||
 ,正畸正颌治疗,锥形束CT,牙根吸收," />
,正畸正颌治疗,锥形束CT,牙根吸收," />