Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (2): 338-344. doi: 10.19723/j.issn.1671-167X.2024.02.022
Previous Articles Next Articles
Preliminarily study of arthrocentesis combined with liquid phase concentrated growth factor injection in the treatment of unilateral temporomandibular joint osteoarthritis
Hongguang LI1,Weihua HAN1,Xun WU1,Jiling FENG2,Gang LI2,Juanhong MENG1,3,*( )
)
- 1. Department of Oral and Maxillofacial Surgery, Beijing 100081, China
2. Department of Oral and Maxillofacial Radiology, Beijing 100081, China
3. Center for Temporomandibular Joint Disorder and Orofacial Pain, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R782.6
| 1 |
Cömert Kiliç S , Güngörmüȿ M , Sümbüllü MA . Is arthrocentesis plus platelet-rich plasma superior to arthrocentesis alone in the treatment of temporomandibular joint osteoarthritis? A randomized clinical trial[J]. J Oral Maxillofac Surg, 2015, 73 (8): 1473- 1483.
doi: 10.1016/j.joms.2015.02.026 |
| 2 |
Bergstrand S , Ingstad HK , Møystad A , et al. Long-term effectiveness of arthrocentesis with and without hyaluronic acid injection for treatment of temporomandibular joint osteoarthritis[J]. J Oral Sci, 2019, 61 (1): 82- 88.
doi: 10.2334/josnusd.17-0423 |
| 3 |
Sikora M , Czerwińska-Niezabitowska B , Chęciński MA , et al. Short-term effects of intra-articular hyaluronic acid administration in patients with temporomandibular joint disorders[J]. J Clin Med, 2020, 9 (6): 1749.
doi: 10.3390/jcm9061749 |
| 4 |
Lee HM , Shen EC , Shen JT , et al. Tensile strength, growth factor content and proliferation activities for two platelet concentrates of platelet-rich fibrin and concentrated growth factor[J]. J Dent Sci, 2020, 15 (2): 141- 146.
doi: 10.1016/j.jds.2020.03.011 |
| 5 |
Tabatabaei F , Aghamohammadi Z , Tayebi L . In vitro and in vivo effects of concentrated growth factor on cells and tissues[J]. J Biomed Mater Res A, 2020, 108 (6): 1338- 1350.
doi: 10.1002/jbm.a.36906 |
| 6 | 汪淼, 程飚. 浓缩血小板在医学美容与组织再生中的临床应用[M]. 北京: 北京大学医学出版社, 2020: 272- 295. |
| 7 |
Chung PY , Lin MT , Chang HP . Effectiveness of platelet-rich plasma injection in patients with temporomandibular joint osteoarthritis: A systematic review and meta-analysis of randomized controlled trials[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2019, 127 (2): 106- 116.
doi: 10.1016/j.oooo.2018.09.003 |
| 8 |
Yang JW , Huang YC , Wu SL , et al. Clinical efficacy of a centric relation occlusal splint and intra-articular liquid phase concen-trated growth factor injection for the treatment of temporomandibular disorders[J]. Medicine, 2017, 96 (11): 6302- 6308.
doi: 10.1097/MD.0000000000006302 |
| 9 |
Rodella LF , Favero G , Boninsegna R , et al. Growth factors, CD34 positive cells, and fibrin network analysis in concentrated growth factors fraction[J]. Microsc Res Tech, 2011, 74 (8): 772- 777.
doi: 10.1002/jemt.20968 |
| 10 |
傅开元. 2014年新版国际颞下颌关节紊乱病分类及诊断标准解读[J]. 中华口腔医学杂志, 2017, 52 (6): 374- 376.
doi: 10.3760/cma.j.issn.1002-0098.2017.06.010 |
| 11 | 孟娟红, 甘业华, 马绪臣. 颞下颌关节骨关节炎发病的分子机制及相关治疗的实验研究[J]. 北京大学学报(医学版), 2013, 45 (1): 5- 8. |
| 12 |
Cömert Kiliç S , Güngörmüȿ M . Is arthrocentesis plus platelet-rich plasma superior to arthrocentesis plus hyaluronic acid for the treatment of temporomandibular joint osteoarthritis: A randomized clinical trial[J]. Int J Oral Maxillofac Surg, 2016, 45 (12): 1538- 1544.
doi: 10.1016/j.ijom.2016.06.009 |
| 13 |
Kopp S , Wenneberg B , Haraldson T , et al. The short-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint pain and dysfunction[J]. J Oral Maxillofac Surg, 1985, 43 (6): 429- 435.
doi: 10.1016/S0278-2391(85)80050-1 |
| 14 |
Guarda-Nardini L , Cadorin C , Frizziero A , et al. Comparison of 2 hyaluronic acid drugs for the treatment of temporomandibular joint osteoarthritis[J]. J Oral Maxillofac Surg, 2012, 70 (11): 2522- 2530.
doi: 10.1016/j.joms.2012.07.020 |
| 15 |
Gurung T , Singh RK , Mohammad S , et al. Efficacy of arthrocentesis versus arthrocentesis with sodium hyaluronic acid in temporomandibular joint osteoarthritis: A comparison[J]. Natl J Maxillofac Surg, 2017, 8 (1): 41- 49.
doi: 10.4103/njms.NJMS_84_16 |
| 16 |
Li C , Long X , Deng M , et al. Osteoarthritic changes after superior and inferior joint space injection of hyaluronic acid for the treatment of temporomandibular joint osteoarthritis with anterior disc displacement without reduction: A cone-beam computed tomographic evaluation[J]. J Oral Maxillofac Surg, 2015, 73 (2): 232- 244.
doi: 10.1016/j.joms.2014.08.034 |
| 17 |
Cömert Kiliç S . Does glucosamine, chondroitin sulfate, and methylsulfonylmethane supplementation improve the outcome of temporomandibular joint osteoarthritis management with arthrocentesis plus intraarticular hyaluronic acid injection. A randomized clinical trial[J]. J Craniomaxillofac Surg, 2021, 49 (8): 711- 718.
doi: 10.1016/j.jcms.2021.02.012 |
| 18 |
Altman RD , Manjoo A , Fierlinger A , et al. The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: A systematic review[J]. BMC Musculoskelet Disord, 2015, 16 (1): 321- 330.
doi: 10.1186/s12891-015-0775-z |
| 19 |
Ferreira N , Masterson D , Lopes de Lima R , et al. Efficacy of viscosupplementation with hyaluronic acid in temporomandibular disorders: A systematic review[J]. J Craniomaxillofac Surg, 2018, 46 (11): 1943- 1952.
doi: 10.1016/j.jcms.2018.08.007 |
| 20 | Lin SL , Tsai CC , Wu SL , et al. Effect of arthrocentesis plus platelet-rich plasma and platelet-rich plasma alone in the treatment of temporomandibular joint osteoarthritis: A retrospective matched cohort study (A STROBE-compliant article)[J]. Medicine (Baltimore), 2018, 97 (16): 477- 484. |
| 21 |
Gokçe Kutuk S , Gökçe G , Arslan M , et al. Clinical and radiological comparison of effects of platelet-rich plasma, hyaluronic acid, and corticosteroid injections on temporomandibular joint osteoarthritis[J]. J Craniofac Surg, 2019, 30 (4): 1144- 1148.
doi: 10.1097/SCS.0000000000005211 |
| 22 | Zotti F , Albanese M , Rodella LF , et al. Platelet-rich plasma in treatment of temporomandibular joint dysfunctions: Narrative review[J]. Int J Mol Sci, 2019, 20 (2): 277- 290. |
| 23 |
Marx RE , Harrell DB . Translational research: The CD34+ cell is crucial for large-volume bone regeneration from the milieu of bone marrow progenitor cells in craniomandibular reconstruction[J]. Int J Oral Maxillofac Implants, 2014, 29 (2): 201- 209.
doi: 10.11607/jomi.te56 |
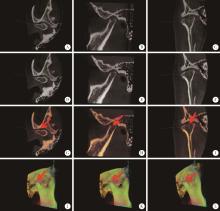
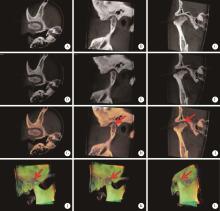
| 24 | Feng JL , Ma RH , Du H , et al. Diagnostic accuracy of fused CBCT images in the evaluation of temporomandibular joint condylar bone resorption[J]. Clin Oral Invest, 2023, 27 (3): 1277- 1288. |
| 25 | 李红光, 吴训, 彭慧钰, 等. 基于CBCT的单侧颞下颌关节骨关节炎临床表现与髁突骨质改变类型的相关性分析[J]. 现代口腔医学杂志, 2022, 36 (3): 148- 152. |
| [1] | Hao WU,Li-ping PAN,Heng LIU,Hong-bin WANG,Tai-guo NING,Yong-ping CAO. Effect of posterior tibial slope on the short-term outcome in mobile-bearing unicompartmental knee arthroplasty [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 877-882. |
| [2] | WU Jun-hui,CHEN Hong-bo,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,WANG Meng-ying,WANG Si-yue,WANG Xiao-wen,WANG Jia-ting,YU Huan,HU Yong-hua. Prevalence and risk factors of osteoarthritis in patients with type 2 diabetes in Beijing, China from 2015 to 2017 [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 518-522. |
| [3] | ZHOU Jing,LIU Yi. Cone-beam CT evaluation of temporomandibular joint in skeletal class Ⅱ female adolescents with different vertical patterns [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 109-119. |
| [4] | KE Yan,ZHANG Qiang,MA Yun-qing,LI Ru-jun,TAO Ke,GUI Xian-ge,LI Ke-peng,ZHANG Hong,LIN Jian-hao. Short-term outcomes of total hip arthroplasty in the treatment of Tönnis grade 3 hip osteoarthritis in patients with spondyloepiphyseal dysplasia [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 175-182. |
| [5] | HAN Wei-hua,LUO Hai-yan,GUO Chuan-bin,NING Qi,MENG Juan-hong. Expression of cartilage oligomeric matrix protein in the synovial chondromatosis of the temporomandibular joint [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 34-39. |
| [6] | Fei LI,Jing QIAO,Jin-yu DUAN,Yong ZHANG,Xiu-jing WANG. Effect of concentrated growth factors combined with guided tissue regeneration in treatment of classⅡ furcation involvements of mandibular molars [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 346-352. |
| [7] | Shuo CHEN,Yang HE,Jin-gang AN,Yi ZHANG. Application of computer-aided virtual mandibular position in the simultaneous treatment of children with temporomandibular joint ankylosis and jaw deformity [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 954-958. |
| [8] | Ming-zhe LI,Xiao-xia WANG,Zi-li LI,Biao YI,Cheng LIANG,Wei HE. Accuracy analysis of computer assisted navigation for condylectomy via intraoral approach [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 182-186. |
| [9] | Xiao-ying ZHANG,Jia-jing PENG,Chuan-hui LIU,Xiao-yan CAI,Jiang-lin ZHANG,Yi-fang MEI,Hong-tao JIN,Xiao-fei WANG,Hong MO,Zhan-guo LI. A multi-center cross-sectional survey of medicine application in patients with osteoarthritis in China [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1044-1048. |
| [10] | WANG Dan-dan, GAN Ye-hua, MA Xu-chen, MENG Juan-hong. Association between ADAMTS14 gene polymorphism and the temporomandibular joint osteoarthritis in Chinese Han females [J]. Journal of Peking University(Health Sciences), 2018, 50(2): 279-283. |
| [11] | QIAO Jing, DUAN Jin-yu, CHU Yi, SUN Chang-zhou. Effect of concentrated growth factors on the treatment of degree Ⅱ furcation involvements of mandibular molars [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 36-042. |
| [12] | MENG Juan-hong, GUO Yu-xing, LUO Hai-yan, GUO Chuan-bin, MA Xu-chen. Diagnosis and treatment of diffuse tenosynovial giant cell tumor arising from temporomandibular joints [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 1049-1054. |
| [13] | CHEN Fei, PAN Shao-xia, FENG Hai-lan. Distribution and content of transforming growth factor-β1 and vascular endothelial growth factor in each layer of concentrated growth factors [J]. Journal of Peking University(Health Sciences), 2016, 48(5): 860-865. |
| [14] | LEI Jie,LIU Mu-qing,FU Kai-yuan. Disturbedsleep, anxiety and stress are possible risk indicators for temporomandibular disorders with myofascialpain [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 692-696. |
| [15] | LI Zhi-chang, JIANG Long, ZHANG Shu, QIN Xue-ying, Daniel K. White PT,HOU Yun-fei, ZHOU Zhi-wei, LIN Jian-hao. Evaluation of physical function for the end-stage osteoarthritis patient waiting for the total knee replacement [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 257-262. |
|
||