Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (6): 1079-1085. doi: 10.19723/j.issn.1671-167X.2022.06.004
Previous Articles Next Articles
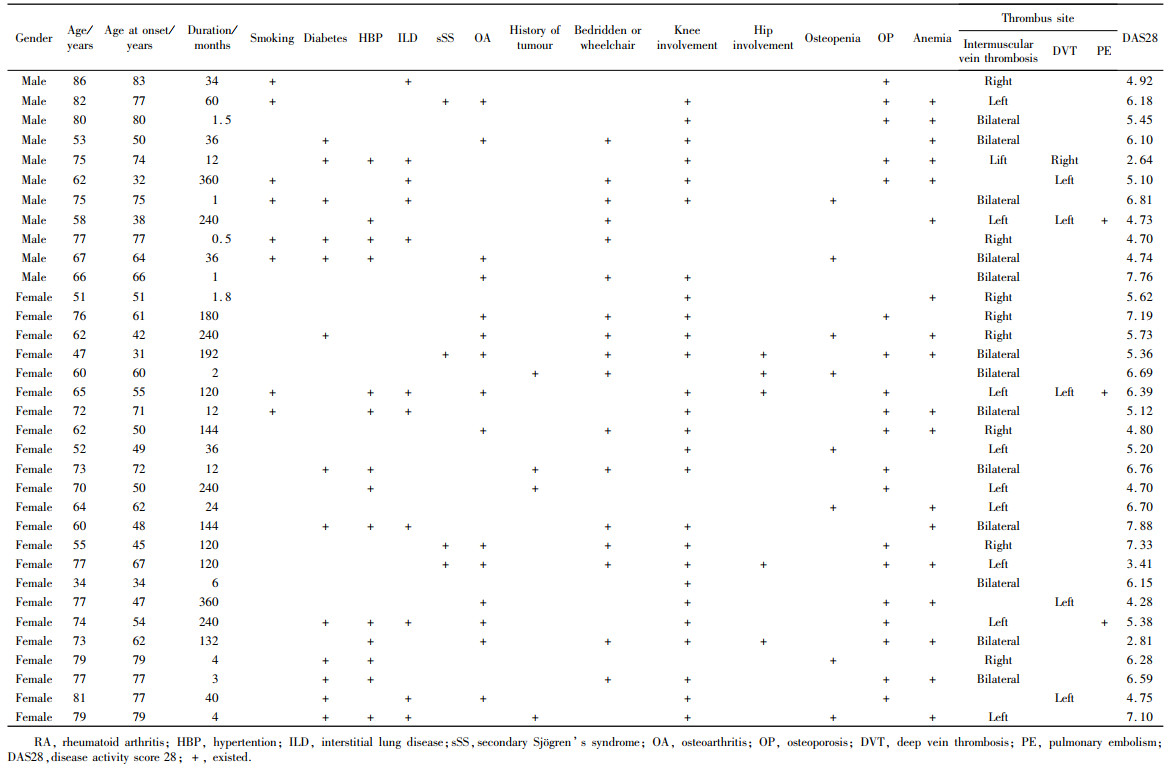
Clinical characteristics of patients with rheumatoid arthritis complicated with venous thrombosis of lower extremities
Rui LIU1,Jin-xia ZHAO1,*( ),Liang YAN1,2
),Liang YAN1,2
- 1. Department of Rheumatology and Immunology, Peking University Third Hospital, Beijing 100191, China
2. Department of Emergency, Yan'an Branch of Peking University Third Hospital (Traditional Chinese Medicine Hospital of Yan'an), Yan'an 716000, Shaanxi, China
CLC Number:
- R593.2
| 1 |
Li LY , Lu N , Avina-Galindo AM , et al. The risk and trend of pulmonary embolism and deep vein thrombosis in rheumatoid arthritis: A general population-based study[J]. Rheumatology (Oxford), 2021, 60 (1): 188- 195.
doi: 10.1093/rheumatology/keaa262 |
| 2 |
Matta F , Singala R , Yaekoub AY , et al. Risk of venous thromboembolism with rheumatoid arthritis[J]. Thromb Haemost, 2009, 101 (1): 134- 138.
doi: 10.1160/TH08-08-0551 |
| 3 |
Arnett FC , Edworthy SM , Bloch DA , et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis[J]. Arthritis Rheum, 1988, 31 (3): 315- 324.
doi: 10.1002/art.1780310302 |
| 4 |
Britsemmer K , Ursum J , Gerritsen M , et al. Validation of the 2010 ACR/EULAR classification criteria for rheumatoid arthritis: Slight improvement over the 1987 ACR criteria[J]. Ann Rheum Dis, 2011, 70 (8): 1468- 1470.
doi: 10.1136/ard.2010.148619 |
| 5 |
Chopard R , Albertsen IE , Piazza G . Diagnosis and treatment of lower extremity venous thromboembolism: A review[J]. JAMA, 2020, 324 (17): 1765- 1776.
doi: 10.1001/jama.2020.17272 |
| 6 |
Arshad N , Isaksen T , Hansen JB , et al. Time trends in incidence rates of venous thromboembolism in a large cohort recruited from the general population[J]. Eur J Epidemiol, 2017, 32 (4): 299- 305.
doi: 10.1007/s10654-017-0238-y |
| 7 |
Meng K , Hu X , Peng X , et al. Incidence of venous thromboembolism during pregnancy and the puerperium: A systematic review and meta-analysis[J]. J Matern Fetal Neonatal Med, 2015, 28 (3): 245- 253.
doi: 10.3109/14767058.2014.913130 |
| 8 | Croles FN , Nasserinejad K , Duvekot JJ , et al. Pregnancy, thrombophilia, and the risk of a first venous thrombosis: systematic review and Bayesian meta-analysis[J]. BMJ, 2017, 359, j4452. |
| 9 | Crous-Bou M , de Vivo I , Camargo CA Jr. , et al. Interactions of established risk factors and a GWAS-based genetic risk score on the risk of venous thromboembolism[J]. Thromb Haemost, 2016, 116 (4): 705- 713. |
| 10 | Heit JA , Ashrani A , Crusan DJ , et al. Reasons for the persistent incidence of venous thromboembolism[J]. ThrombHaemost, 2017, 117 (2): 390- 400. |
| 11 |
Mean M , Limacher A , Stalder O , et al. Do factor V Leiden and prothrombin G20210A mutations predict recurrent venous thromboembolism in older patients?[J]. Am J Med, 2017, 130 (10): 1220.e17- 1220.e22.
doi: 10.1016/j.amjmed.2017.05.026 |
| 12 |
Gregson J , Kaptoge S , Bolton T , et al. Cardiovascular risk factors associated with venous thromboembolism[J]. JAMA Cardiol, 2019, 4 (2): 163- 173.
doi: 10.1001/jamacardio.2018.4537 |
| 13 |
Peng YH , Lin YS , Chen CH , et al. Type 1 diabetes is associated with an increased risk of venous thromboembolism: A retrospective population-based cohort study[J]. PLoS One, 2020, 15 (1): e0226997.
doi: 10.1371/journal.pone.0226997 |
| 14 |
Riva N , Donadini MP , AgenoW . Epidemiology and pathophysiology of venous thromboembolism: Similarities with atherothrombosis and the role of inflammation[J]. Thromb Haemost, 2015, 113 (6): 1176- 1183.
doi: 10.1160/TH14-06-0563 |
| 15 |
Chen CY , Liao KM . The incidence of deep vein thrombosis in Asian patients with chronic obstructive pulmonary disease[J]. Medicine (Baltimore), 2015, 94 (44): e1741.
doi: 10.1097/MD.0000000000001741 |
| 16 |
Ogdie A , McGill NK , Shin DB , et al. Risk of venous thromboembolism in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: A general population-based cohort study[J]. Eur Heart J, 2018, 39 (39): 3608- 3614.
doi: 10.1093/eurheartj/ehx145 |
| 17 |
Lurie JM , Png CYM , Subramaniam S , et al. Virchow's triad in "silent" deep vein thrombosis[J]. J Vasc Surg Venous Lymphat Disord, 2019, 7 (5): 640- 645.
doi: 10.1016/j.jvsv.2019.02.011 |
| 18 | Broussard J , Berlinger M , Lauret D . A clot (possibly): Due to loss of TNF-α supression[J]. J La State Med Soc, 2017, 169 (2): 52. |
| 19 |
Mease P , Charles-Schoeman C , Cohen S , et al. Incidence of venous and arterial thromboembolic events reported in the tofacitinib rheumatoid arthritis, psoriasis and psoriatic arthritis development programmes and from real-world data[J]. Ann Rheum Dis, 2020, 79 (11): 1400- 1413.
doi: 10.1136/annrheumdis-2019-216761 |
| 20 |
Arshad N , Isaksen T , Hansen JB , et al. Time trends in incidence rates of venous thromboembolism in a large cohort recruited from the general population[J]. Eur J Epidemiol, 2017, 32 (4): 299- 305.
doi: 10.1007/s10654-017-0238-y |
| [1] | Dongwu LIU, Jie CHEN, Mingli GAO, Jing YU. Rheumatoid arthritis with Castleman-like histopathology in lymph nodes: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 928-931. |
| [2] | Huina HUANG,Jing ZHAO,Xiangge ZHAO,Ziran BAI,Xia LI,Guan WANG. Regulatory effect of lactate on peripheral blood CD4+ T cell subsets in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 519-525. |
| [3] | Xiaofei TANG,Yonghong LI,Qiuling DING,Zhuo SUN,Yang ZHANG,Yumei WANG,Meiyi TIAN,Jian LIU. Incidence and risk factors of deep vein thrombosis in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 279-283. |
| [4] | Xue ZOU,Xiao-juan BAI,Li-qing ZHANG. Effectiveness of tofacitinib combined with iguratimod in the treatment of difficult-to-treat moderate-to-severe rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1013-1021. |
| [5] | Qi WU,Yue-ming CAI,Juan HE,Wen-di HUANG,Qing-wen WANG. Correlation between dyslipidemia and rheumatoid arthritis associated interstitial lung disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 982-992. |
| [6] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Correlation analysis between body mass index and clinical characteristics of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 993-999. |
| [7] | Yin-ji JIN,Lin SUN,Jin-xia ZHAO,Xiang-yuan LIU. Significance of IgA isotype of anti-v-raf murine sarcoma viral oncogene homologue B1 antibody in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 631-635. |
| [8] | Li-jia MA,Pan-pan HU,Xiao-guang LIU. Spinal metastases combined with leptomeningeal metastasis: A case report [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 563-566. |
| [9] | Wen-xin CAI,Shi-cheng LI,Yi-ming LIU,Ru-yu LIANG,Jing LI,Jian-ping GUO,Fan-lei HU,Xiao-lin SUN,Chun LI,Xu LIU,Hua YE,Li-zong DENG,Ru LI,Zhan-guo LI. A cross-sectional study on the clinical phenotypes of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1068-1073. |
| [10] | Fang CHENG,Shao-ying YANG,Xing-xing FANG,Xuan WANG,Fu-tao ZHAO. Role of the CCL28-CCR10 pathway in monocyte migration in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1074-1078. |
| [11] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Cross-sectional study on quality of life and disease activity of rheumatoid arthritis patients [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1086-1093. |
| [12] | Er-shu BO,Peng HONG,Yu ZHANG,Shao-hui DENG,Li-yuan GE,Min LU,Nan LI,Lu-lin MA,Shu-dong ZHANG. Clinicopathological features and prognostic analysis of papillary renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 615-620. |
| [13] | GAO Chao,CHEN Li-hong,WANG Li,YAO Hong,HUANG Xiao-wei,JIA Yu-bo,LIU Tian. Validation of the Pollard’s classification criteria (2010) for rheumatoid arthritis patients with fibromyalgia [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 278-282. |
| [14] | LOU Xue,LIAO Li,LI Xing-jun,WANG Nan,LIU Shuang,CUI Ruo-mei,XU Jian. Methylation status and expression of TWEAK gene promoter region in peripheral blood of patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1020-1025. |
| [15] | ZHONG Hua,XU Li-ling,BAI Ming-xin,SU Yin. Effect of chemokines CXCL9 and CXCL10 on bone erosion in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1026-1031. |
|
||