Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (5): 896-901. doi: 10.19723/j.issn.1671-167X.2024.05.022
Previous Articles Next Articles
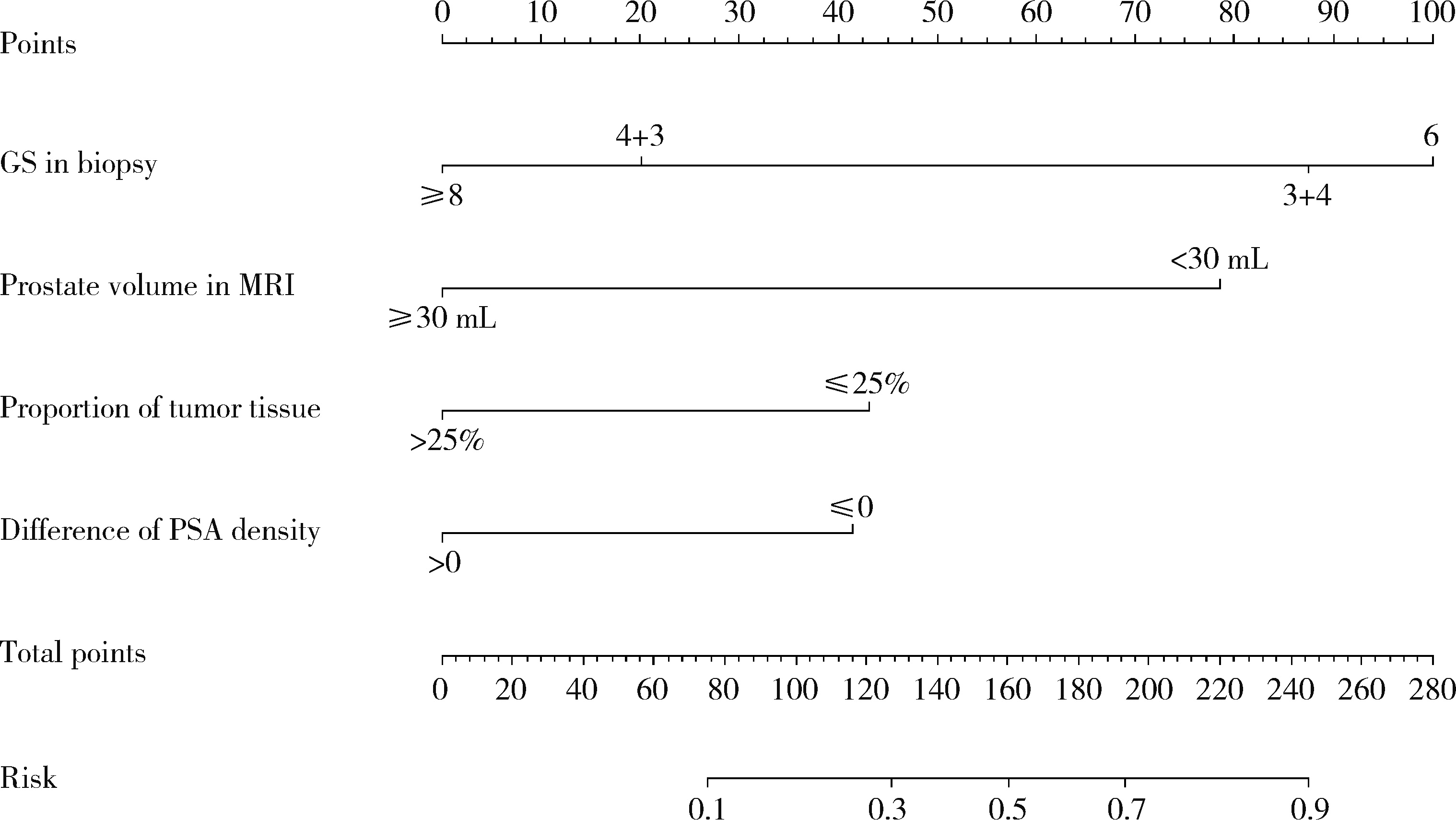
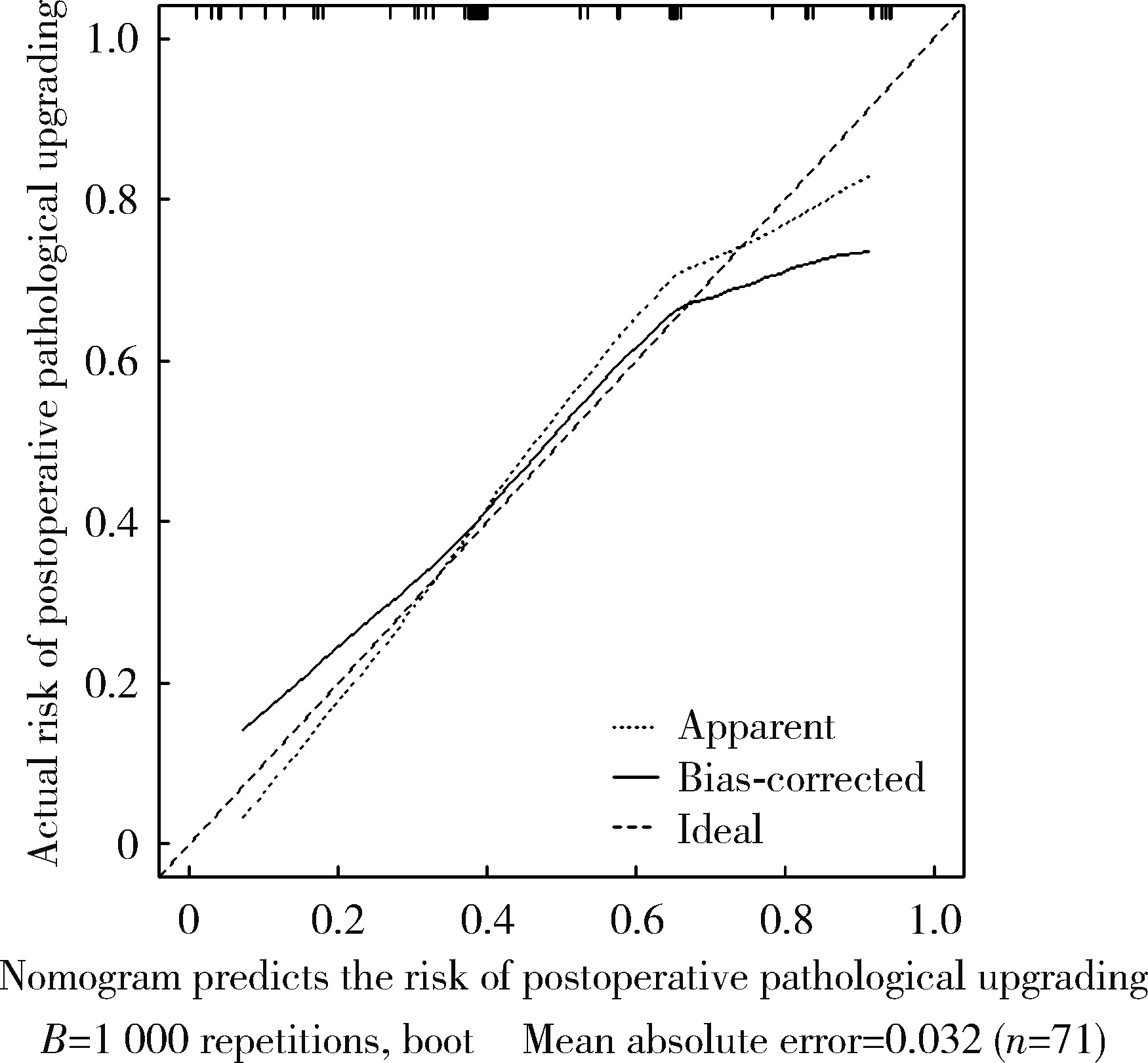
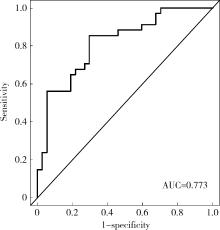
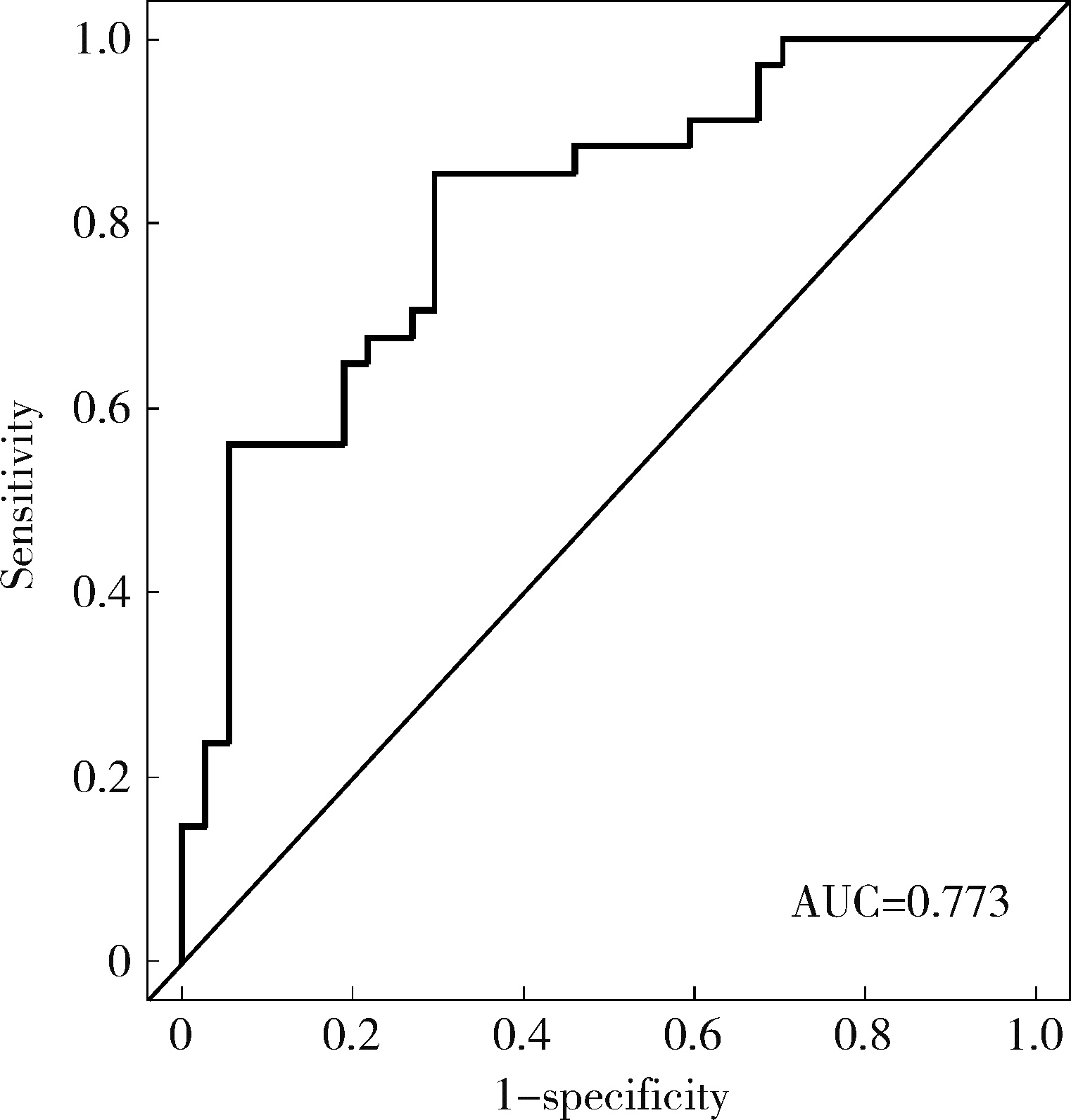
Risk factors analysis and nomogram model construction of postoperative pathological upgrade of prostate cancer patients with single core positive biopsy
Zhicun LI, Tianyu WU, Lei LIANG, Yu FAN, Yisen MENG*( ), Qian ZHANG*(
), Qian ZHANG*( )
)
- Department of Urology, Peking University First Hospital; Institution of Urology, Peking University; Beijing Key Laboratory of Urogenital Diseases (Male) Molecular Diagnosis and Treatment Center; National Urological Cancer Center, Beijing 100034, China
CLC Number:
- R737.25
| 1 | 郑荣寿, 陈茹, 韩冰峰, 等. 2022年中国恶性肿瘤流行情况分析[J]. 中华肿瘤杂志, 2024, 46 (3): 221- 231. |
| 2 |
Siegel RL , Miller KD , Jemal A . Cancer statistics, 2020[J]. CA Cancer J Clin, 2020, 70 (1): 7- 30.
doi: 10.3322/caac.21590 |
| 3 | 徐毅, 毛祺琦, 刘犇, 等. 穿刺单针阳性前列腺癌的术后病理特征分析[J]. 中华泌尿外科杂志, 2018, 39 (10): 757- 760. |
| 4 | 陈小豹, 张潮鸿, 江玮, 等. 前列腺穿刺单针阳性的临床特点[J]. 中国男科学杂志, 2019, 33 (3): 30- 33. |
| 5 | 唐超来, 唐贤富, 郑兴明. 前列腺穿刺活检单针阳性患者行前列腺根治性切除术后的病理特征[J]. 国际泌尿系统杂志, 2020, 40 (4): 587- 590. |
| 6 |
Goldstein NS , Bégin LR , Grody WW , et al. Minimal or no cancer in radical prostatectomy specimens. Report of 13 cases of the "vanishing cancer phenomenon"[J]. Am J Surg Pathol, 1995, 19 (9): 1002- 1009.
doi: 10.1097/00000478-199509000-00003 |
| 7 |
Ricardo Kupka da S , Dall'Oglio MF , Sant'Ana AC , et al. Can single positive core prostate cancer at biopsy be considered a low-risk disease after radical prostatectomy?[J]. Int Braz J Urol, 2013, 39 (6): 800- 807.
doi: 10.1590/S1677-5538.IBJU.2013.06.05 |
| 8 | 刘希高, 谌诚, 李健, 等. 前列腺穿刺活检单针阳性患者前列腺内癌灶分布特点[J]. 中华男科学杂志, 2012, 18 (2): 155- 159. |
| 9 | 杜少静, 贺慧颖. 穿刺单针阳性前列腺癌患者根治术后62例临床病理分析[J]. 中华病理学杂志, 2016, 45 (7): 446- 450. |
| 10 |
郝一昌, 颜野, 张帆, 等. 穿刺活检单针阳性的前列腺癌手术策略选择及经验总结[J]. 北京大学学报(医学版), 2020, 52 (4): 625- 631.
doi: 10.19723/j.issn.1671-167X.2020.04.005 |
| 11 | Dong F , Jones JS , Stephenson AJ , et al. Prostate cancer volume at biopsy predicts clinically significant upgrading[J]. J Urol, 2008, 179 (3): 896- 900. |
| 12 | Hwang I , Lim D , Jeong YB , et al. Upgrading and upstaging of low-risk prostate cancer among Korean patients: A multicenter study[J]. Asian J Androl, 2015, 17 (5): 811- 814. |
| [1] | Yukai LI, Hongyan WANG, Liang LUO, Yun LI, Chun LI. Clinical significance of antiphospholipid antibodies in Behcet disease with thrombosis [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1036-1040. |
| [2] | Yang TIAN, Yongzheng HAN, Jiao LI, Mingya WANG, Yinyin QU, Jingchao FANG, Hui JIN, Min LI, Jun WANG, Mao XU, Shenglin WANG, Xiangyang GUO. Incidence and risk factors of postoperative epidural hematoma following anterior cervical spine surgery [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1058-1064. |
| [3] | Mingrui WANG, Jinhui LAI, Jiaxiang JI, Xinwei TANG, Haopu HU, Qi WANG, Kexin XU, Tao XU, Hao HU. Risk factors for decreased quality of life in patients with kidney stones predicted by the Chinese version of Wisconsin stone quality of life questionnaire [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1069-1074. |
| [4] | Yuanmei LIU, Yicheng FU, Jingxin HAO, Fuchun ZHANG, Huilin LIU. Construction and validation of a nomogram for predicting in-hospital postoperative heart failure in elderly patients with hip fracture [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 874-883. |
| [5] | Yuxuan TIAN,Mingjian RUAN,Yi LIU,Derun LI,Jingyun WU,Qi SHEN,Yu FAN,Jie JIN. Predictive effect of the dual-parametric MRI modified maximum diameter of the lesions with PI-RADS 4 and 5 on the clinically significant prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 567-574. |
| [6] | Kaifeng YAO,Mingjian RUAN,Derun LI,Yuxuan TIAN,Yuke CHEN,Yu FAN,Yi LIU. Diagnostic efficacy of targeted biopsy combined with regional systematic biopsy in prostate cancer in patients with PI-RADS 4-5 [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 575-581. |
| [7] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [8] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [9] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [10] | Yan CHEN,Kuangmeng LI,Kai HONG,Shudong ZHANG,Jianxing CHENG,Zhongjie ZHENG,Wenhao TANG,Lianming ZHAO,Haitao ZHANG,Hui JIANG,Haocheng LIN. Retrospective study on the impact of penile corpus cavernosum injection test on penile vascular function [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 680-686. |
| [11] | Bo PANG,Tongjun GUO,Xi CHEN,Huaqi GUO,Jiazhang SHI,Juan CHEN,Xinmei WANG,Yaoyan LI,Anqi SHAN,Hengyi YU,Jing HUANG,Naijun TANG,Yan WANG,Xinbiao GUO,Guoxing LI,Shaowei WU. Personal nitrogen oxides exposure levels and related influencing factors in adults over 35 years old in Tianjin and Shanghai [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 700-707. |
| [12] | Jing HE,Zhongze FANG,Ying YANG,Jing LIU,Wenyao MA,Yong HUO,Wei GAO,Yangfeng WU,Gaoqiang XIE. Relationship between lipid metabolism molecules in plasma and carotid atheroscle-rotic plaques, traditional cardiovascular risk factors, and dietary factors [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 722-728. |
| [13] | Shan CAI,Yihang ZHANG,Ziyue CHEN,Yunfe LIU,Jiajia DANG,Di SHI,Jiaxin LI,Tianyu HUANG,Jun MA,Yi SONG. Status and pathways of factors influencing physical activity time among elementary and junior high school students in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 403-410. |
| [14] | Zuhong ZHANG,Tianjiao CHEN,Jun MA. Associations between puberty timing and cardiovascular metabolic risk factors among primary and secondary students [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 418-423. |
| [15] | Yuting LIN,Huali WANG,Yu TIAN,Litong GONG,Chun CHANG. Factors influencing cognitive function among the older adults in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 456-461. |
|
||