Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (4): 796-802. doi: 10.19723/j.issn.1671-167X.2025.04.027
Previous Articles Next Articles
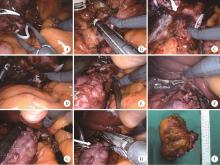
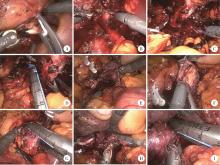
Robot-assisted laparoscopic inferior vena cava segmental resection for renal tumor with tumor thrombus invading the vascular wall
Shuai LIU, Zhuo LIU, Yunhe GUAN, Guoliang WANG, Xiaojun TIAN, Hongxian ZHANG, Lei LIU, Lulin MA, Shudong ZHANG*( )
)
- Department of Urology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.11
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
叶剑飞, 马潞林, 赵磊, 等. 腔静脉节段切除术在处理侵犯腔静脉的肾肿瘤瘤栓中的应用[J]. 北京大学学报(医学版), 2018, 50 (1): 183- 187.
doi: 10.3969/j.issn.1671-167X.2018.01.031 |
| 7 |
刘茁, 王国良, 田晓军, 等. 下腔静脉节段性切除术在肾癌伴下腔静脉癌栓中的应用[J]. 现代泌尿外科杂志, 2018, 23 (9): 677- 681.
|
| 8 |
|
| 9 |
|
| 10 |
|
| 11 |
|
| 12 |
|
| 13 |
|
| 14 |
赵勋, 颜野, 黄晓娟, 等. 癌栓粘连血管壁对非转移性肾细胞癌合并下腔静脉癌栓患者手术及预后的影响[J]. 北京大学学报(医学版), 2021, 53 (4): 665- 670.
doi: 10.19723/j.issn.1671-167X.2021.04.007 |
| 15 |
|
| 16 |
|
| 17 |
|
| 18 |
|
| 19 |
|
| 20 |
|
| 21 |
|
| 22 |
|
| 23 |
|
| 24 |
|
| 25 |
|
| 26 |
|
| 27 |
|
| 28 |
|
| [1] | Boda GUO, Min LU, Guoliang WANG, Hongxian ZHANG, Lei LIU, Xiaofei HOU, Lei ZHAO, Xiaojun TIAN, Shudong ZHANG. Clinicopathological and prognostic differences between clear cell and non-clear cell renal cell carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 644-649. |
| [2] | Zhanyi ZHANG, Min LU, Yuehao SUN, Jinghan DONG, Xiaofei HOU, Chunlei XIAO, Guoliang WANG, Xiaojun TIAN, Lulin MA, Hongxian ZHANG, Shudong ZHANG. Clinicopathological features and survival analysis of TFE3-rearranged renal cell carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 650-661. |
| [3] | Zonghan LI, Yangyue HUANG, Ning LI, Minglei LI, Hongcheng SONG, Weiping ZHANG, Chao LIU. Preliminary application of domestic single-port serpentine arm robotic surgical system in children's pyeloplasty [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 662-665. |
| [4] | Qiming ZHANG, Zebo CHEN, Yu TIAN, Dameng PAN, Lei LIU, Hongxian ZHANG, Lei ZHAO, Shudong ZHANG, Lulin MA, Xiaofei HOU. Experience summary of robot-assisted laparoscopic transplant nephrectomy [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 666-669. |
| [5] | Shihao LIU, Liqing XU, Xinfei LI, Kunlin YANG, Zhaoying LI, Zibo ZHANG, Xiang WANG, Wei-xiao FU, Zhihua LI, Xuesong LI. Evaluation of the feasibility and safety of a Chinese developed modular surgical robotic system for robot-assisted pyeloplasty [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 779-783. |
| [6] | Huanrui WANG, Shicong LAI, Haopu HU, Zehua DING, Tao XU, Hao HU. Efficacy analysis of laparoscopy combined with flexible ureteroscope in the treatment of complex ureteral stricture [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 784-788. |
| [7] | Kewei CHEN,Zhuo LIU,Shaohui DENG,Fan ZHANG,Jianfei YE,Guoliang WANG,Shudong ZHANG. Clinical diagnosis and treatment of renal angiomyolipoma with inferior vena cava tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 617-623. |
| [8] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [9] | Jie YANG,Jieli FENG,Shudong ZHANG,Lulin MA,Qing ZHENG. Clinical effects of transesophageal echocardiography in different surgical methods for nephrectomy combined with Mayo Ⅲ-Ⅳ vena tumor thrombectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 631-635. |
| [10] | Binshuai WANG,Min QIU,Qianjin ZHANG,Maofeng TIAN,Lei LIU,Guoliang WANG,Min LU,Xiaojun TIAN,Shudong ZHANG. Experience in diagnosis and treatment of 6 cases of renal Ewing's sarcoma with venous thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 636-639. |
| [11] | Yicen YING,Yicong DU,Zhihua LI,Yiming ZHANG,Xinfei LI,Bing WANG,Peng ZHANG,Hongjian ZHU,Liqun ZHOU,Kunlin YANG,Xuesong LI. Robot-assisted laparoscopic ureteroplasty with buccal mucosa graft for complex ureteral stricture [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 640-645. |
| [12] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [13] | Dong LAN,Zhuo LIU,Yu-xuan LI,Guo-liang WANG,Xiao-jun TIAN,Lu-lin MA,Shu-dong ZHANG,Hong-xian ZHANG. Risk factors for massive hemorrhage after radical nephrectomy and removal of venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 825-832. |
| [14] | Min QIU,You-long ZONG,Bin-shuai WANG,Bin YANG,Chu-xiao XU,Zheng-hui SUN,Min LU,Lei ZHAO,Jian LU,Cheng LIU,Xiao-jun TIAN,Lu-lin MA. Treatment outcome of laparoscopic partial nephrectomy in patients with renal tumors of moderate to high complexity [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 833-837. |
| [15] | Wei ZUO,Fei GAO,Chang-wei YUAN,Sheng-wei XIONG,Zhi-hua LI,Lei ZHANG,Kun-lin YANG,Xin-fei LI,Liang LIU,Lai WEI,Peng ZHANG,Bing WANG,Ya-ming GU,Hong-jian ZHU,Zheng ZHAO,Xue-song LI. Trends in upper urinary tract reconstruction surgery over a decade based on a multi-center database [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 692-698. |
|
||