Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (2): 314-319. doi: 10.19723/j.issn.1671-167X.2021.02.014
Previous Articles Next Articles
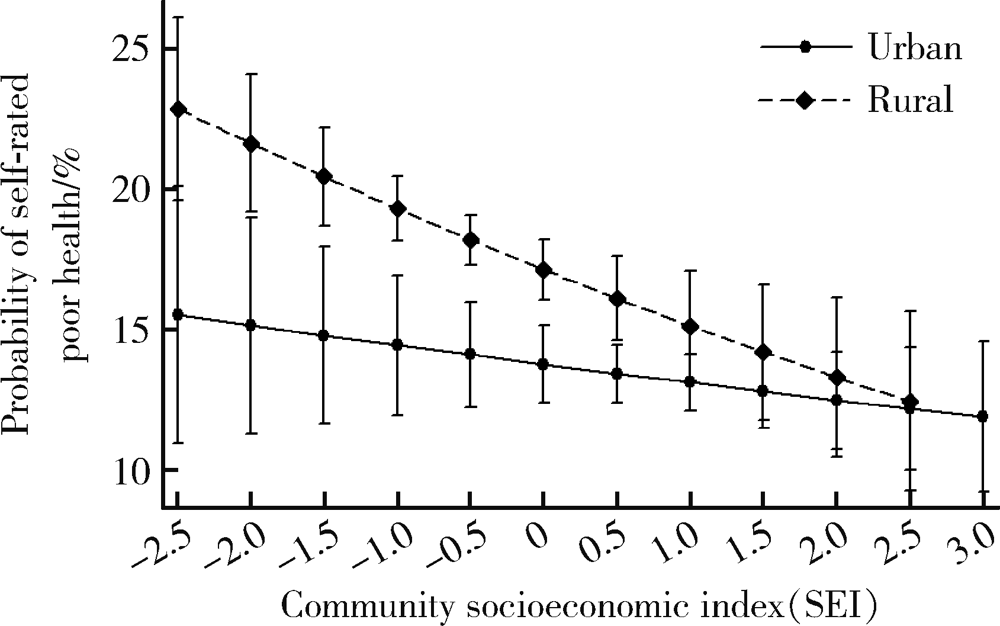
Association between community socioeconomic status and adults’ self-rated health in China
- Department of Health Policy and Management, Peking University School of Public Health, Beijing 100191, China
CLC Number:
- R19
| [1] | 中共中央国务院印发《“健康中国2030”规划纲要》. [EB/OL] (2016-10-25) [2019-03-25]. http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm. |
| [2] |
Tang S, Meng Q, Chen L, et al. Tackling the challenges to health equity in China[J]. Lancet, 2008,372(9648):1493-1501.
pmid: 18930531 |
| [3] |
Xu H, Xie Y. Socioeconomic inequalities in health in China: A reassessment with data from the 2010-2012 China Family Panel Studies[J]. Soc Indic Res, 2017,132(1):219-239.
pmid: 28694561 |
| [4] |
Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: A systematic subnational analysis for the Global Burden of Disease Study 2013[J]. Lancet, 2016,387(10015):251-272.
doi: 10.1016/S0140-6736(15)00551-6 pmid: 26510778 |
| [5] |
Wang Y, Li X, Zhou M, et al. Under-5 mortality in 2 851 Chinese counties, 1996-2012: A subnational assessment of achieving MDG 4 goals in China[J]. Lancet, 2016,387(10015):273-283.
doi: 10.1016/S0140-6736(15)00554-1 pmid: 26510780 |
| [6] | Noble M, Wright G, Smith G, et al. Measuring multiple deprivation at the small-area level[J]. Environ Plan A, 2006,38(1):169-185. |
| [7] |
Pickett KE, Pearl M. Multilevel analyses of neighbourhood socio-economic context and health outcomes: A critical review[J]. J Epidemiol Community Health, 2001,55(2):111-122.
doi: 10.1136/jech.55.2.111 pmid: 11154250 |
| [8] |
Daponte-Codina A, Bolivar-Munoz J, Toro-Cardenas S, et al. Area deprivation and trends in inequalities in self-rated health in Spain, 1987-2001[J]. Scand J Public Health, 2008,36(5):504-515.
pmid: 18567655 |
| [9] | Xiao Q, Berrigan D, Matthews CE. A prospective investigation of neighborhood socioeconomic deprivation and self-rated health in a large US cohort[J]. Health Place, 2017(44):70-76. |
| [10] |
Rejineveld S. The impact of individual and area characteristics on urban socioeconomic differences in health and smoking[J]. Int J Epidemiol, 1998,27(1):33-40.
pmid: 9563691 |
| [11] | Lei L. The impact of community context on children’s health and nutritional status in China[J]. Soc Sci Med, 2017(179):172-181. |
| [12] | 谢宇, 胡婧炜, 张春泥. 中国家庭追踪调查:理念与实践[J]. 社会, 2014(2):1-32. |
| [13] |
Xie Y, Lu P. The sampling design of the China family panel stu-dies (CFPS)[J]. Chin J Sociol, 2015,1(4):471-484.
pmid: 29854418 |
| [14] |
Xu H, Xie Y. Socioeconomic inequalities in health in China: A reassessment with data from the 2010-2012 China family panel studies[J]. Soc Indic Res, 2017,132(1):219-239.
pmid: 28694561 |
| [15] |
Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index[J]. J Urban Health, 2006,83(6):1041-1062.
pmid: 17031568 |
| [16] |
Desalvo KB, Bloser N, Reynolds K, et al. Mortality prediction with a single general self-rated health question. A meta-analysis[J]. J Gen Intern Med, 2006,21(3):267-275.
pmid: 16336622 |
| [17] |
Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model[J]. Soc Sci Med, 2009,69(3):307-316.
doi: 10.1016/j.socscimed.2009.05.013 pmid: 19520474 |
| [18] | Galster GC. The mechanism (s) of neighbourhood effects: Theory, evidence, and policy implications[M]// Neighbourhood effects research: New perspectives. Dordrecht, Holland: Springer, 2012: 23-56. |
| [19] | Zhang X, Fan S, Zhang L, et al. Local governance and public goods provision in rural China[J]. J Public Econ, 2004,88(12):2857-2871. |
| [20] |
Sylvia S, Shi Y, Xue H, et al. Survey using incognito stan-dardized patients shows poor quality care in China’s rural clinics[J]. Health Policy Plan, 2015,30(3):322-333.
pmid: 24653216 |
| [21] |
Hosseinpoor AR, Bergen N, Schlotheuber A, et al. Measuring health inequalities in the context of sustainable development goals[J]. Bull World Health Organ, 2018,96(9):654-659.
pmid: 30262947 |
| [22] | 关于实施健康扶贫工程的指导意见[EB/OL]. (2016-06-21) [2019-03-25]. http://www.gov.cn/xinwen/2016-06/21/content_5084195.htm. |
| [1] | Jiang JIN, Xue CHEN, Yan ZHAO, Jun JIA, Jianzhong ZHANG. The role and its regulatory significance of interleukin-25 in ovalbumin induced atopic dermatitis of mice [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 756-762. |
| [2] | Ting JING,Hua JIANG,Ting LI,Qianqian SHEN,Lan YE,Yindan ZENG,Wenxin LIANG,Gang FENG,Man-Yau Szeto Ignatius,Yumei ZHANG. Relationship between serum 25-hydroxyvitamin D and handgrip strength in middle-aged and elderly people in five cities of Western China [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 448-455. |
| [3] | Qingbo WANG,Hongqiao FU. Main characteristics and historical evolution of China' s health financing transition [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 462-470. |
| [4] | Jia-hui DENG,Xiao-lin HUANG,Xiao-xing LIU,Jie SUN,Lin LU. The past, present and future of sleep medicine in China [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 567-封三. |
| [5] | Zi-xiang GAO,Yong WANG,Ao-nan WEN,Yu-jia ZHU,Qing-zhao QIN,Yun ZHANG,Jing WANG,Yi-jiao ZHAO. Automatic determination of mandibular landmarks based on three-dimensional mandibular average model [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 174-180. |
| [6] | Ling-wei MENG,Xue LI,Sheng-han GAO,Yue LI,Rui-tao CAO,Yi ZHANG,Shao-xia PAN. Comparison of three methods for establishing rat peri-implantitis model [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 22-29. |
| [7] | Rui-jie CAO,Zhong-qiang YAO,Peng-qing JIAO,Li-gang CUI. Comparison of diagnostic efficacy of different classification criteria for Takayasu arteritis in Chinese patients [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1128-1133. |
| [8] | Zhe LIANG,Fang-fang FAN,Yan ZHANG,Xian-hui QIN,Jian-ping LI,Yong HUO. Rate and characteristics of H-type hypertension in Chinese hypertensive population and comparison with American population [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1028-1037. |
| [9] | Xiao-xuan LIU,Xiao-hui DUAN,Shuo ZHANG,A-ping SUN,Ying-shuang ZHANG,Dong-sheng FAN. Genetic distribution in Chinese patients with hereditary peripheral neuropathy [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 874-883. |
| [10] | Li ZHANG,Ji-fang GONG,Hong-ming PAN,Yu-xian BAI,Tian-shu LIU,Ying CHENG,Ya-chi CHEN,Jia-ying HUANG,Ting-ting XU,Fei-jiao GE,Wan-ling HSU,Jane SHI,Xi-chun HU,Lin SHEN. Atezolizumab therapy in Chinese patients with locally advanced or metastatic solid tumors: An open-label, phase Ⅰ study [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 971-980. |
| [11] | Yu-han DENG,Yong JIANG,Zi-yao WANG,Shuang LIU,Yu-xin WANG,Bao-hua LIU. Long short-term memory and Logistic regression for mortality risk prediction of intensive care unit patients with stroke [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 458-467. |
| [12] | Jia-he ZHANG,Jia-qi SHI,Zhang-jian CHEN,Guang JIA. Effects of nano titanium dioxide on gut microbiota based on human digestive tract microecology simulation system in vitro [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 468-476. |
| [13] | LIU Si-min,ZHAO Yi-jiao,WANG Xiao-yan,WANG Zu-hua. In vitro evaluation of positioning accuracy of trephine bur at different depths by dynamic navigation [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 146-152. |
| [14] | XU Ying, Ci-ren-yang-jin. Analysis of the relationship between high altitude polycythemia and peptic ulcer bleeding [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 161-165. |
| [15] | WANG Gui-hong,ZUO Ting,LI Ran,ZUO Zheng-cai. Effect of rebamipide on the acute gouty arthritis in rats induced by monosodium urate crystals [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 716-720. |
|
||