Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (4): 615-620. doi: 10.19723/j.issn.1671-167X.2022.04.006
Previous Articles Next Articles
Clinicopathological features and prognostic analysis of papillary renal cell carcinoma
Er-shu BO1,Peng HONG1,Yu ZHANG1,Shao-hui DENG1,Li-yuan GE1,Min LU2,Nan LI3,Lu-lin MA1,Shu-dong ZHANG1,*( )
)
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Department of Pathology, Peking University Third Hospital, Beijing 100191, China
3. Research Centre of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.11
| 1 |
Siegel RL , Miller KD , Jemal A . Cancer statistics, 2019[J]. CA Cancer J Clin, 2019, 69 (1): 7- 34.
doi: 10.3322/caac.21551 |
| 2 |
Qu Y , Chen H , Gu W , et al. Age-dependent association between sex and renal cell carcinoma mortality: A population-based analysis[J]. Sci Rep, 2015, 5 (1): 9160.
doi: 10.1038/srep09160 |
| 3 |
Znaor A , Lortet-Tieulent J , Laversanne M , et al. International variations and trends in renal cell carcinoma incidence and mortality[J]. Eur Urol, 2015, 67 (3): 519- 530.
doi: 10.1016/j.eururo.2014.10.002 |
| 4 |
Akhtar M , Al-Bozom IA , Al Hussain T . Papillary renal cell carcinoma (PRCC): An update[J]. Adv Anat Pathol, 2019, 26 (2): 124- 132.
doi: 10.1097/PAP.0000000000000220 |
| 5 |
Mir MC , Derweesh I , Porpiglia F , et al. Partial nephrectomy versus radical nephrectomy for clinical T1b and T2 renal tumors: A systematic review and meta-analysis of comparative studies[J]. Eur Urol, 2017, 71 (4): 606- 617.
doi: 10.1016/j.eururo.2016.08.060 |
| 6 |
Mancilla-Jimenez R , Stanley RJ , Blath RA , et al. Papillary renal cell carcinoma a clinical, radiologic, and pathologic study of 34 cases[J]. Cancer, 1976, 38 (6): 2469- 2480.
doi: 10.1002/1097-0142(197612)38:6<2469::AID-CNCR2820380636>3.0.CO;2-R |
| 7 |
Thoenes W , Störkel S , Rumpelt HJ . Histopathology and classification of renal cell tumors (adenomas, oncocytomas and carcinomas): The basic cytological and histopathological elements and their use for diagnostics[J]. Pathol Res Pract, 1986, 181 (2): 125- 143.
doi: 10.1016/S0344-0338(86)80001-2 |
| 8 | Delahunt B , Eble JN . Papillary renal cell carcinoma: A clinicopathologic and immunohistochemical study of 105 tumors[J]. Mod Pathol, 1997, 10 (6): 537- 544. |
| 9 |
Aron M , Nguyen MM , Stein RJ , et al. Impact of gender in renal cell carcinoma: An analysis of the SEER database[J]. Eur Urol, 2008, 54 (1): 133- 140.
doi: 10.1016/j.eururo.2007.12.001 |
| 10 |
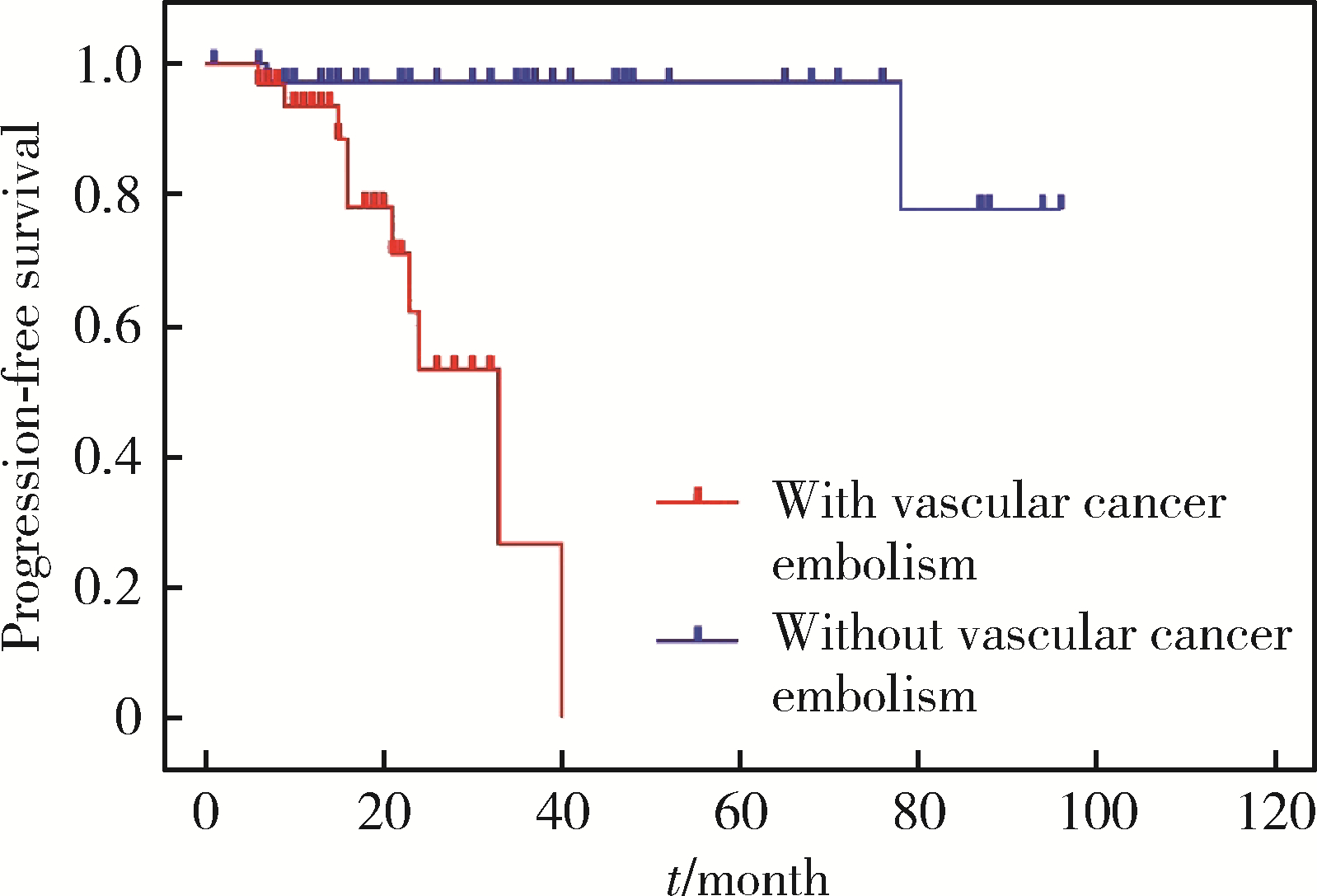
Hong B , Hou H , Chen L , et al. The clinicopathological features and prognosis in patients with papillary renal cell carcinoma: A multicenter retrospective study in Chinese population[J]. Front Oncol, 2021, 11, 753690.
doi: 10.3389/fonc.2021.753690 |
| 11 |
Bigot P , Bernhard JC , Gill IS , et al. The subclassification of papillary renal cell carcinoma does not affect oncological outcomes after nephron sparing surgery[J]. World J Urol, 2016, 34 (3): 347- 352.
doi: 10.1007/s00345-015-1634-0 |
| 12 |
洪保安, 侯惠民, 陈凌霄, 等. 乳头状肾细胞癌的临床病理特征及预后分析[J]. 中华泌尿外科杂志, 2020, 41 (12): 896- 900.
doi: 10.3760/cma.j.cn112330-20200502-00350 |
| 13 | 董樑, 黄吉炜, 奚倩雯, 等. 乳头状肾细胞癌的临床病理特征和预后分析[J]. 中华泌尿外科杂志, 2015, 36 (3): 183- 187. |
| 14 |
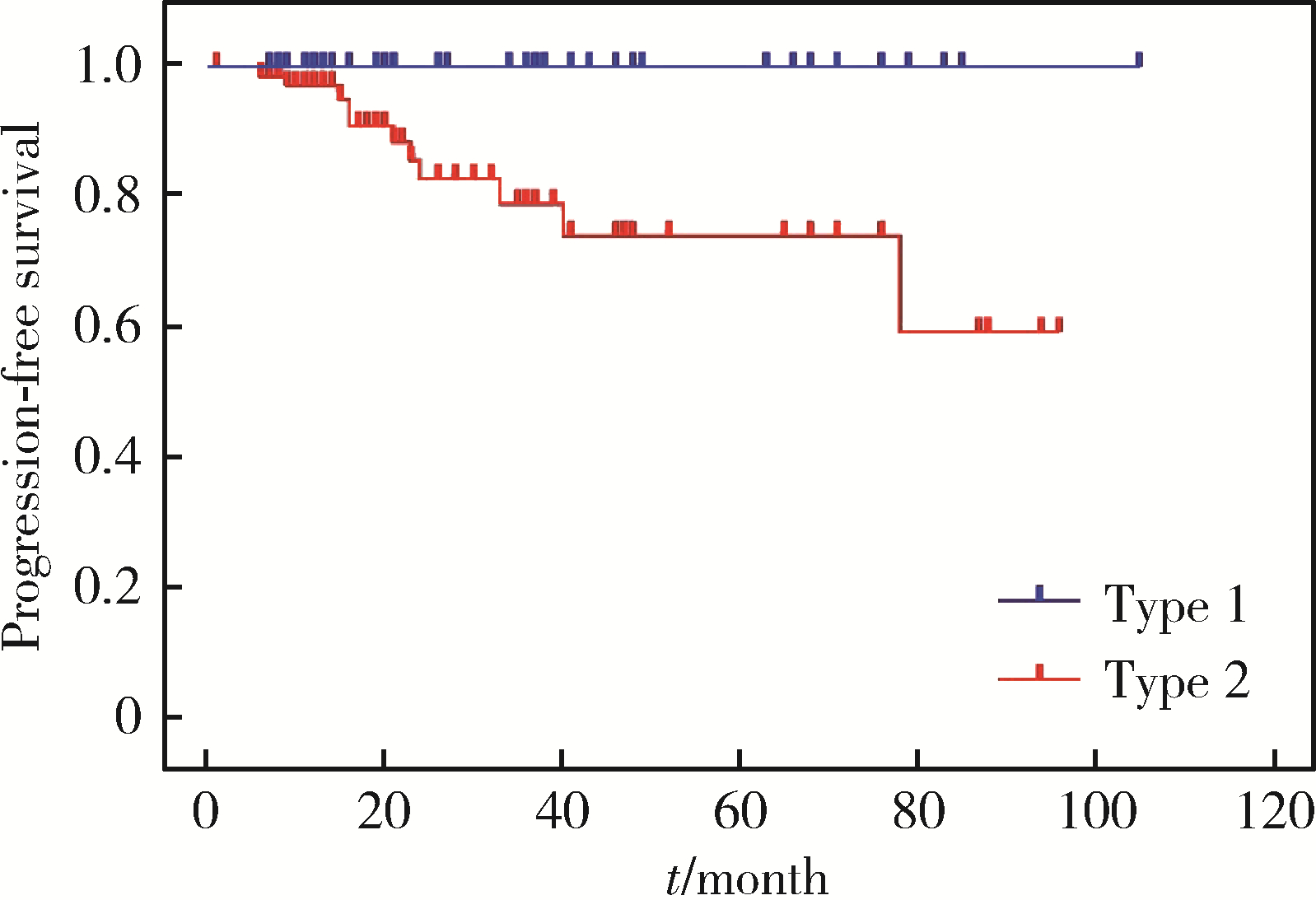
Ha YS , Chung JW , Choi SH , et al. Clinical significance of subclassification of papillary renal cell carcinoma: Comparison of cli-nicopathologic parameters and oncologic outcomes between papillary histologic subtypes 1 and 2 using the Korean renal cell carcinoma database[J]. Clin Genitourin Cancer, 2017, 15 (2): e181- e186.
doi: 10.1016/j.clgc.2016.07.020 |
| 15 |
Pan H , Ye L , Zhu Q , et al. The effect of the papillary renal cell carcinoma subtype on oncological outcomes[J]. Sci Rep, 2020, 10 (1): 21073.
doi: 10.1038/s41598-020-78174-9 |
| 16 |
Sukov WR , Lohse CM , Leibovich BC , et al. Clinical and pathological features associated with prognosis in patients with papillary renal cell carcinoma[J]. J Urol, 2012, 187 (1): 54- 59.
doi: 10.1016/j.juro.2011.09.053 |
| 17 |
Ku JH , Moon KC , Kwak C , et al. Is there a role of the histologic subtypes of papillary renal cell carcinoma as a prognostic factor?[J]. Jpn J Clin Oncol, 2009, 39 (10): 664- 670.
doi: 10.1093/jjco/hyp075 |
| 18 | 黄健. 中国泌尿外科和男科疾病诊断治疗指南(2019版)[M]. 北京: 科学出版社, 2020: 6- 8. |
| 19 |
Fernandes DS , Lopes JM . Pathology, therapy and prognosis of papillary renal carcinoma[J]. Future Oncol, 2015, 11 (1): 121- 132.
doi: 10.2217/fon.14.133 |
| 20 |
Begg CB , Cramer LD , Hoskins WJ . Impact of hospital volume on operative mortality for major cancer surgery[J]. JAMA, 1998, 280 (20): 1747- 1751.
doi: 10.1001/jama.280.20.1747 |
| [1] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [2] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [3] | Le YU,Shaohui DENG,Fan ZHANG,Ye YAN,Jianfei YE,Shudong ZHANG. Clinicopathological characteristics and prognosis of multilocular cystic renal neoplasm of low malignant potential [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 661-666. |
| [4] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [5] | Yangyi FANG,Qiang LI,Zhigao HUANG,Min LU,Kai HONG,Shudong ZHANG. Well-differentiated papillary mesothelial tumour of the tunica vaginalis: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 741-744. |
| [6] | Yuanyuan ZENG,Yun XIE,Daonan CHEN,Ruilan WANG. Related factors of euthyroid sick syndrome in patients with sepsis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 526-532. |
| [7] | Jian-bin LI,Meng-na LYU,Qiang CHI,Yi-lin PENG,Peng-cheng LIU,Rui WU. Early prediction of severe COVID-19 in patients with Sjögren’s syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1007-1012. |
| [8] | Huan-rui LIU,Xiang PENG,Sen-lin LI,Xin GOU. Risk modeling based on HER-2 related genes for bladder cancer survival prognosis assessment [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 793-801. |
| [9] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [10] | Han LU,Jian-yun ZHANG,Rong YANG,Le XU,Qing-xiang LI,Yu-xing GUO,Chuan-bin GUO. Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 702-707. |
| [11] | Yun-fei SHI,Hao-jie WANG,Wei-ping LIU,Lan MI,Meng-ping LONG,Yan-fei LIU,Yu-mei LAI,Li-xin ZHOU,Xin-ting DIAO,Xiang-hong LI. Analysis of clinicopathological and molecular abnormalities of angioimmunoblastic T-cell lymphoma [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 521-529. |
| [12] | Li-jia MA,Pan-pan HU,Xiao-guang LIU. Spinal metastases combined with leptomeningeal metastasis: A case report [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 563-566. |
| [13] | Xiao-juan ZHU,Hong ZHANG,Shuang ZHANG,Dong LI,Xin LI,Ling XU,Ting LI. Clinicopathological features and prognosis of breast cancer with human epidermal growth factor receptor 2 low expression [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 243-253. |
| [14] | Yu-mei LAI,Zhong-wu LI,Huan LI,Yan WU,Yun-fei SHI,Li-xin ZHOU,Yu-tong LOU,Chuan-liang CUI. Clinicopathological features and prognosis of anorectal melanoma: A report of 68 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 262-269. |
| [15] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
|
||