北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (4): 646-652. doi: 10.19723/j.issn.1671-167X.2019.04.009
肾输尿管全长切除术两种不同术式的双中心疗效对比
吴进锋1,林榕城2,林友成1,蔡旺海1,朱庆国1,方冬2,熊耕砚2,张雷2,周利群2,叶烈夫1,△( ),李学松2,△(
),李学松2,△( )
)
- 1. 福建医科大学省立临床医学院,福建省立医院,福建省立金山医院泌尿外科, 福州 350001
2. 北京大学第一医院泌尿外科,北京大学泌尿外科研究所,国家泌尿男性生殖系肿瘤研究中心, 北京 100034
Comparison of efficacy and safety between two different methods of nephroureterectomy in two centers
Jin-feng WU1,Rong-cheng LIN2,You-cheng LIN1,Wang-hai CAI1,Qing-guo ZHU1,Dong FANG2,Geng-yan XIONG2,Lei ZHANG2,Li-qun ZHOU2,Lie-fu YE1,△( ),Xue-song LI2,△(
),Xue-song LI2,△( )
)
- 1. Department of Urology, Provincial Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fujian Provicial Jinshan Hospital,Fuzhou, 350001, China
2. Department of Urology, Peking University First Hospital; Institute of Urology, Peking University; National Urological Cancer Center, Beijing 100034, China
摘要:
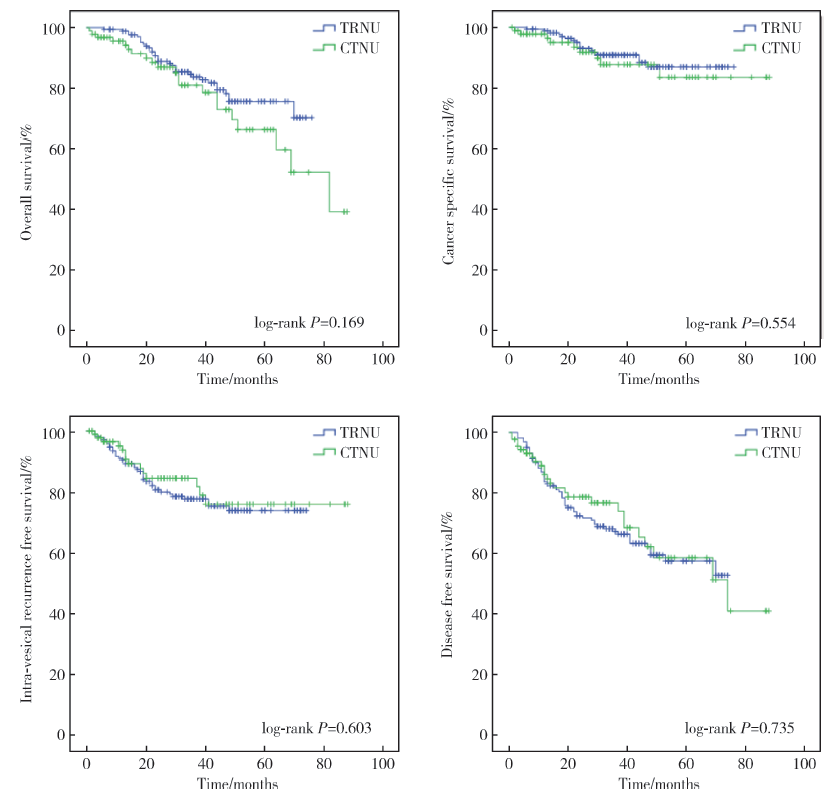
目的:比较经腹完全腹腔镜肾输尿管全长切除术(complete transperitoneal laparoscopic nephroureterectomy, CTNU)和传统后腹腔镜肾输尿管全长切除术(traditional retroperitoneoscopic nephroureterectomy, TRNU)治疗上尿路尿路上皮癌(upper urinary tract urothelial carcinoma, UTUC)的手术安全性和疗效。方法:收集2011年1月至2018年12月期间在北京大学第一医院泌尿外科和福建省立医院泌尿外科接受CTNU和TRNU手术治疗的UTUC病例,比较两种手术方式患者在临床资料、围术期参数、术后随访结果等方面的差异。结果:最终共纳入病例266例,其中CTNU组94例,TRNU组172例。与CTNU组相比,TRNU组左侧病变比例更大(P<0.05)。两组患者年龄、性别分布、体重指数(body mass index,BMI)、美国麻醉医师学会评分(American society of anesthesiologists score, ASA score)、肿瘤所在侧别等方面均差异无统计学意义(P>0.05)。所有病例均完成手术,TRNU中有1例因左肾动脉损伤加行开放血管修补术。CTNU组手术时间为(202.9±76.7) min、术中出血量(68.4±73.3) mL、术后引流管留置天数(3.9±1.5) d、引流液总量(181.7±251.5) mL、术后住院天数(7.8±4.1) d;TRNU组手术时间为(203.5±68.7) min、术中出血量(130.2±252.1) mL、术后引流管留置天数(4.3±1.6) d、引流液总量(179.1±167.5) mL、术后住院天数(8.2±3.7) d。CTNU组术中出血量少于TRNU组,且差异有统计学意义(P=0.005)。中位随访时间39个月(1~88个月),TRNU组的5年总体生存率(overall survival, OS)、肿瘤特异性生存率(cancer specific survival, CSS)、无膀胱复发生存率(intra-vesical recurrence free survival, IvRFS)、无病生存率(disease free survival, DFS)分别为75.6%、86.9%、73.8%、57.5%;CTNU组的5年OS、CSS、IvRFS、DFS分别为66.3%、83.5%、75.9%、58.6%,两组间差异均无统计学意义。结论:CTNU手术是一种安全有效的手术治疗方式,但尚需更进一步的前瞻性随机对照研究加以证实。
中图分类号:
- R737.11
| [1] | Siegel RL, Miller KD, Jemal A , et al. Cancer statistics, 2016[J]. CA Cancer J Clin, 2016,66(1):7-30. |
| [2] | Roupret M, Babjuk M, Comperat E , et al. European association of urology guidelines on upper urinary tract urothelial carcinoma: 2017 update[J]. Eur Urol, 2017,73(1):111-122. |
| [3] | 刘荣耀, 赵鹏举, 李学松 , 等. 经腹腔完全腹腔镜肾输尿管全长切除术治疗上尿路尿路上皮癌[J]. 北京大学学报(医学版), 2011,43(4):531-534. |
| [4] | 李学松, 洪鹏, 丁光璞 , 等. 经腹完全腹腔镜肾输尿管全长切除术的关键技术总结(附光盘)[J]. 现代泌尿外科杂志, 2018,23(10):728-731. |
| [5] | Clayman RV, Kavoussi LR, Figenshau RS , et al. Laparoscopic nephroureterectomy: initial clinical case report[J]. J Laparoendosc Surg, 1991,1(6):343-349. |
| [6] | Ni S, Tao W, Chen Q , et al. Laparoscopic versus open nephroureterectomy for the treatment of upper urinary tract urothelial carcinoma: a systematic review and cumulative analysis of comparative studies[J]. Eur Urol, 2012,61(6):1142-1153. |
| [7] | Ghazi A, Shefler A, Gruell M , et al. A novel approach for a complete laparoscopic nephroureterectomy with bladder cuff excision[J]. J Endourol, 2010,24(3):415-419. |
| [8] | Mcdonald DF . Intussusception ureterectomy: a method of removal of the ureteral stump at time of nephrectomy without an additional incision[J]. Surg Gynecol Obstet, 1953,97(5):565-568. |
| [9] | Gill IS, Soble JJ, Miller SD , et al. A novel technique for management of the en bloc bladder cuff and distal ureter during laparoscopic nephroureterectomy[J]. J Urol, 1999,161(2):430-434. |
| [10] | Gill IS, Sung GT, Hobart MG , et al. Laparoscopic radical nephroureterectomy for upper tract transitional cell carcinoma: the cleveland clinic experience[J]. J Urol, 2000,164(5):1513-1522. |
| [11] | Tsivian A, Benjamin S, Sidi AA . A sealed laparoscopic nephroureterectomy: a new technique[J]. Eur Urol, 2007,52(4):1015-1019. |
| [12] | Jarrett TW, Chan DY, Cadeddu JA , et al. Laparoscopic nephroureterectomy for the treatment of transitional cell carcinoma of the upper urinary tract[J]. Urology, 2001,57(3):448-453. |
| [13] | Yoshino Y, Ono Y, Hattori R , et al. Traditional retroperitoneoscopic nephroureterectomy for transitional cell carcinoma of the renal pelvis and ureter: Nagoya experience[J]. Urology, 2003,61(3):533-538. |
| [14] | Hsi RS, Saint-Elie DT, Zimmerman GJ , et al. Mechanisms of hemostatic failure during laparoscopicnephrectomy: review of Food and Drug Administration database[J]. Urology, 2007,70(5):888-892. |
| [15] | Liu P, Fang D, Xiong G , et al. A novel and simple modification for management of distal ureter during laparoscopic nephroureterectomy without patient repositioning a bulldog clamp technique and description of modified port placement[J]. J Endourol, 2016,30(2):195-200. |
| [16] | Abe T, Shinohara N, Harabayashi T , et al. The role of lymph-node dissection in the treatment of upper urinary tract cancer: a multi-institutional study[J]. BJU Int, 2008,102(5):576-580. |
| [17] | Kondo T, Tanabe K . Role of lymphadenectomy in the management of urothelial carcinoma of the bladder and the upper urinary tract[J]. Int J Urol, 2012,19(8):710-721. |
| [1] | 陈思鹭, 王海菊, 吴宇财, 李志华, 黄燕波, 何宇辉, 许洋洋, 李学松, 贯华. 成人肾积水病因分析:一项单中心横断面研究[J]. 北京大学学报(医学版), 2024, 56(5): 913-918. |
| [2] | 左炜,高菲,袁昌巍,熊盛炜,李志华,张雷,杨昆霖,李新飞,刘靓,魏来,张鹏,王冰,谷亚明,朱宏建,赵峥,李学松. 基于多中心数据库的10年上尿路修复手术术式及术型变化趋势[J]. 北京大学学报(医学版), 2022, 54(4): 692-698. |
| [3] | 李志华,徐纯如,刘颖,贯华,张萌,车新艳,唐琦,黄燕波,李学松,周利群. 饮水习惯与上尿路尿路上皮癌病理特征的相关性分析[J]. 北京大学学报(医学版), 2022, 54(4): 621-627. |
| [4] | 戴翔,王飞,杜依青,宋宇轩,徐涛. 上尿路尿路上皮癌组织中脂肪因子表达与临床病理特征及预后的相关性[J]. 北京大学学报(医学版), 2022, 54(4): 605-614. |
| [5] | 张崔建,何志嵩,周利群. 上尿路尿路上皮癌的淋巴清扫[J]. 北京大学学报(医学版), 2022, 54(4): 592-594. |
| [6] | 程嗣达,李新飞,熊盛炜,樊书菠,王杰,朱伟杰,李子奡,丁光璞,俞婷,李万强,孙永明,杨昆霖,张雷,郝瀚,李学松,周利群. 机器人辅助腹腔镜上尿路修复手术:单一术者108例经验总结[J]. 北京大学学报(医学版), 2020, 52(4): 771-779. |
| [7] | 张军晖,蒋一航,蒋宇光,张际青,康宁. 双侧同步内镜手术治疗双侧上尿路结石的临床效果[J]. 北京大学学报(医学版), 2020, 52(4): 672-677. |
| [8] | 黄炳伟,王杰,张鹏,李喆,毕泗成,王强,岳才博,杨昆霖,李学松,周利群. 吲哚菁绿在复杂上尿路修复手术中的应用[J]. 北京大学学报(医学版), 2020, 52(4): 651-656. |
| [9] | 关豹,翁迈,凡航,彭鼎,方冬,熊耕砚,李学松,周利群. 术前贫血对上尿路尿路上皮癌预后的影响: 单中心686例患者回顾性研究[J]. 北京大学学报(医学版), 2019, 51(6): 1056-1061. |
| [10] | 程嗣达,李万强,穆莉,丁光璞,张博,谌诚,应泽伟,杨昆霖,郝瀚,李学松,周利群. 全腹膜外途径膀胱瓣肾盂吻合自体肾移植术在上尿路尿路上皮癌治疗中的应用[J]. 北京大学学报(医学版), 2019, 51(4): 758-763. |
| [11] | 马闰卓,夏海缀,陆敏,张智荧,张启鸣,卢剑,王国良,马潞林. 输尿管镜活体组织检查对上尿路尿路上皮癌根治性手术的影响[J]. 北京大学学报(医学版), 2019, 51(4): 665-672. |
| [12] | 丁光璞,程嗣达,方冬,杨昆霖,李学松,周辉霞,张骞,叶雄俊,周利群. 上尿路微创手术的技术改良[J]. 北京大学学报(医学版), 2019, 51(4): 610-614. |
| [13] | 马闰卓,邱敏,何为,杨斌,夏海缀,邹达,陆敏,马潞林,卢剑. 输尿管镜活检可协助上尿路尿路上皮癌危险分层[J]. 北京大学学报(医学版), 2017, 49(4): 632-637. |
| [14] | 关豹,曹振朋,彭鼎,李一帆,詹永豪,刘漓波,何世明,熊耕砚,李学松,周利群. T2N0M0期上尿路尿路上皮癌患者预后相关因素分析:单中心235例患者回顾性研究[J]. 北京大学学报(医学版), 2017, 49(4): 603-607. |
| [15] | 柳家园,彭翔,宁向辉,李腾,彭双鹤,王江宜,刘圣杰,丁义,蔡林,龚侃. 尿脱落细胞荧光原位杂交检查阳性在尿路上皮癌中的临床价值[J]. 北京大学学报(医学版), 2017, 49(4): 585-589. |
|
||