北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (1): 90-96. doi: 10.19723/j.issn.1671-167X.2020.01.014
Delaire头影测量分析法预测正颌手术患者上颌及颏部理想矢状向位置的可行性评估
- 北京大学口腔医学院·口腔医院,口腔颌面外科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室, 北京 100081
Feasibility of Delaire cephalometric analysis to predict the ideal sagittal position of the maxilla and chin for surgery-first patients in orthognathic surgery
Xian-tao SUN,Wei HE,Xiao-jing LIU,Zi-li LI( ),Xing WANG
),Xing WANG
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Disease & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
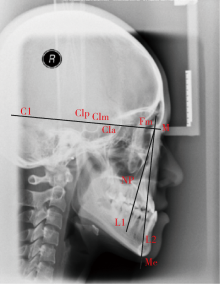
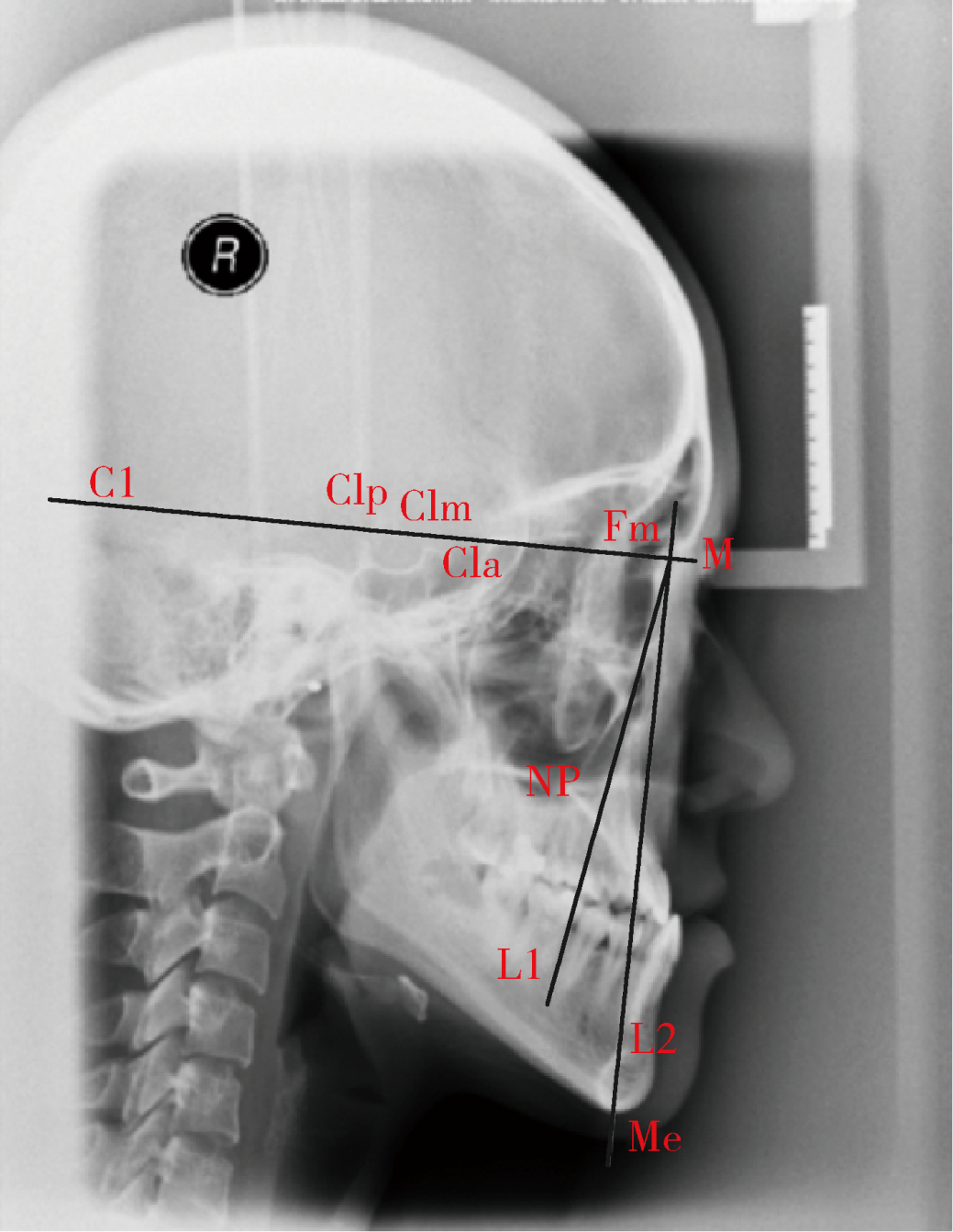
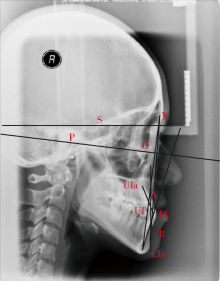
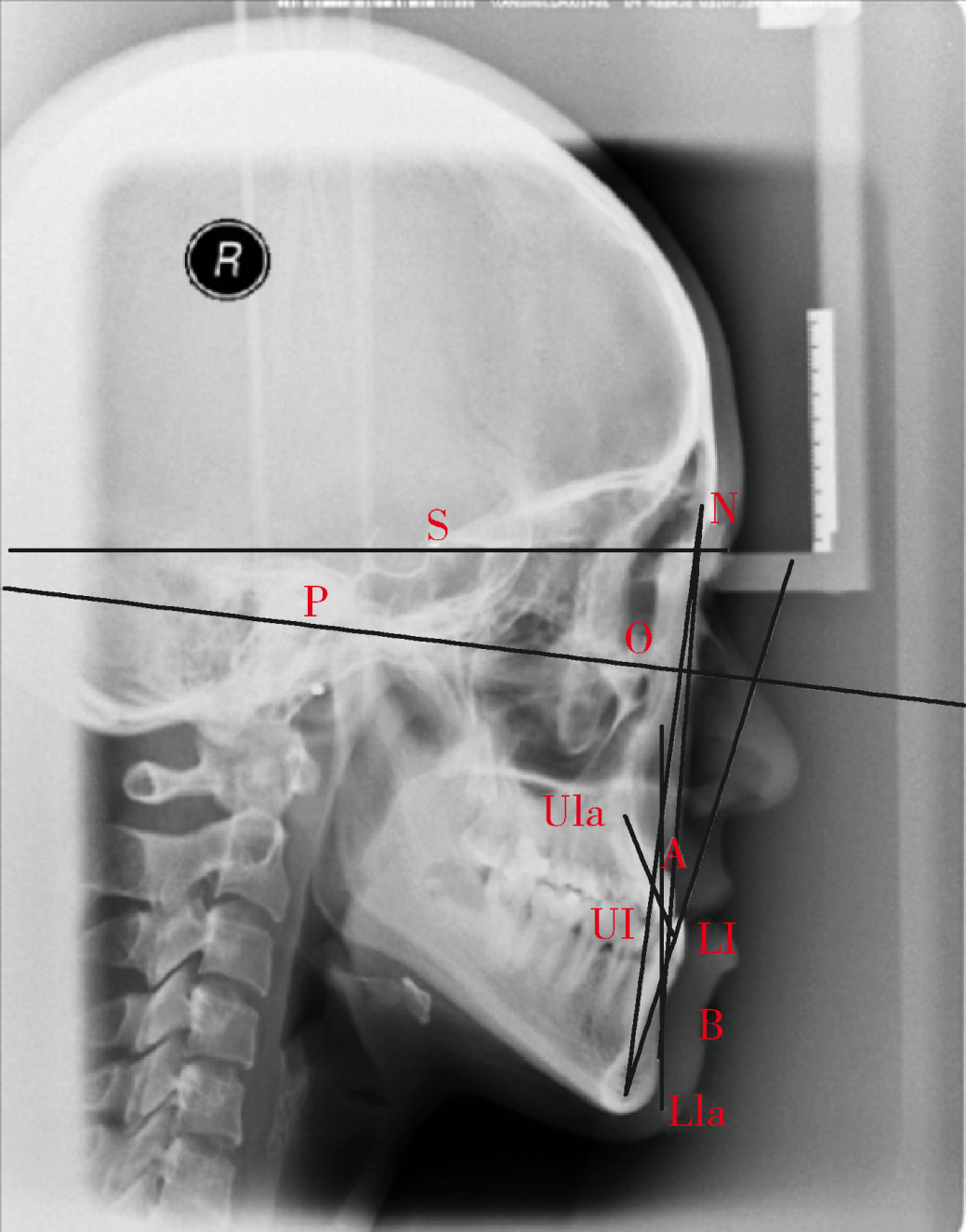
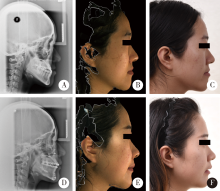
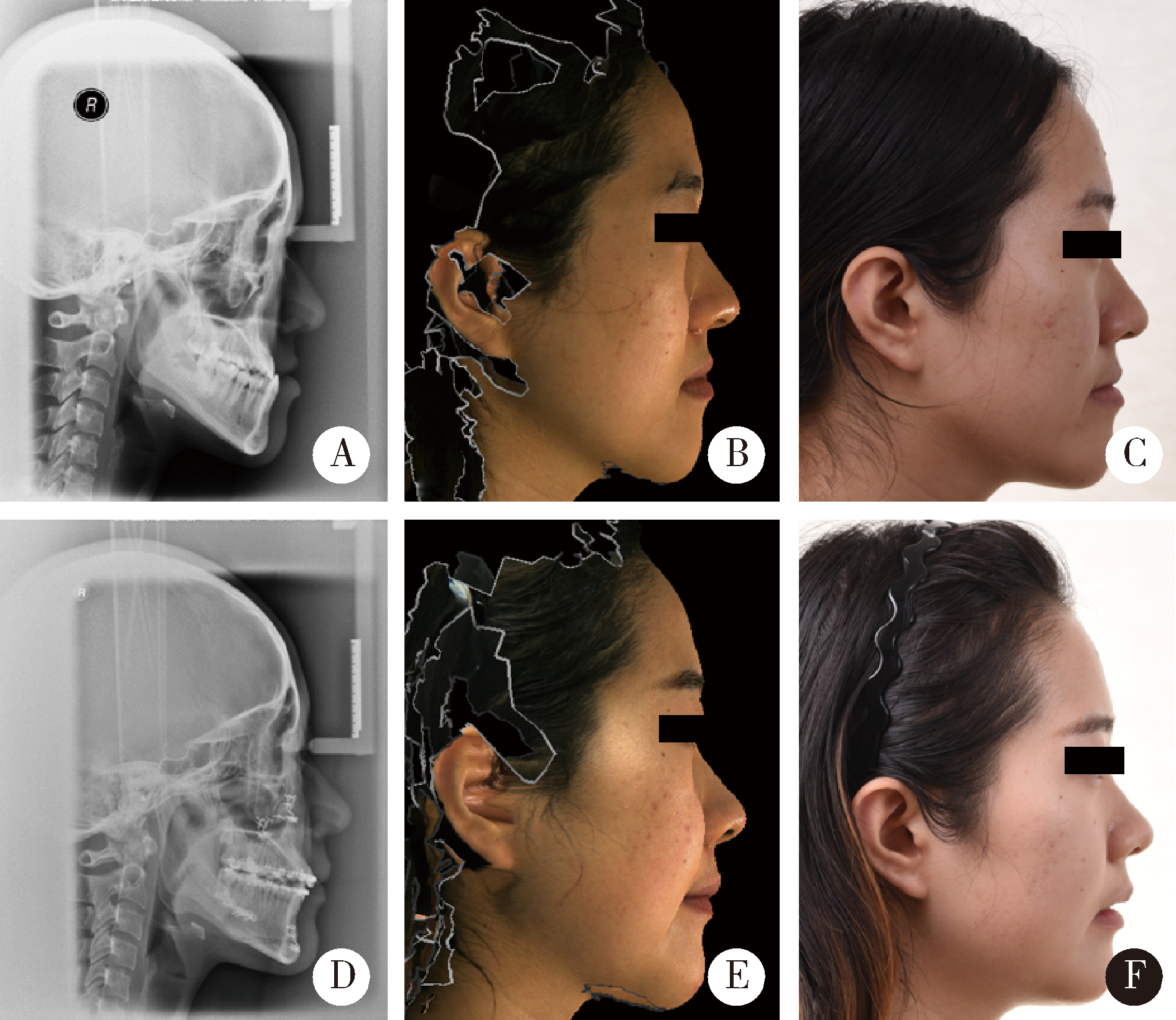
目的:对于使用传统头影测量分析法辅助、并采用手术优先方式治疗的骨性Ⅲ类畸形患者,本研究使用Delaire头影测量分析法回顾性分析患者治疗前后颌骨矢状向位置变化,评估Delaire头影测量分析法预测上颌骨及颏部矢状向理想位置的可行性。方法: 纳入符合标准的骨性Ⅲ类畸形患者共35例,收集治疗前(T0),治疗结束后(T1)的定位头颅侧位片、侧位面相和三维面部照片资料;使用Dolphin Imaging软件测量分析上颌鼻腭点(NP)、颏部颏下点(Me)矢状向位置参考线L1、L2与颅底前线(C1)的夹角∠C1-L1、∠C1-L2等头影测量数据;由正颌、正畸专业医生各4名,以及4名非医学专业大学生对患者侧貌美学以视觉模拟评分(visual analogue scale,VAS)的方式进行评分,对结果行统计学分析。结果: T0期男性:∠C1-L1=80.85°±3.81°,∠C1-L2=89.37°±4.10°;女性: ∠C1-L1=82.87°±4.25°,∠C1-L2=89.69°±4.95°;T1期男性:∠C1-L1=83.93°±2.99°,∠C1-L2=89.08°±2.48°,女性:∠C1-L1=85.67°±3.60°,∠C1-L2=88.30°±4.20°。男女患者T0期测量值与中国美貌人群参考值比较,差异均有统计学意义;T1期上颌NP点测量值与中国美貌人群比较,差异无统计学意义;T1期颏部Me点与中国美貌人群比较,相对靠前,差异具有统计学意义。侧貌美学评分结果,男性、女性T1期上颌、颏部和整体的评分均较T0期有提高,差异具有统计学意义。结论: Deliare头影测量分析法有助于更准确分析患者颌骨畸形状态,能够很好地反映患者治疗后上颌骨和颏部矢状向位置,可以帮助预测颌骨理想的矢状向位置,有望成为制定手术优先正颌手术方案的重要预测方法。
中图分类号:
- R782.2
| [1] | Hussels W, Nanda RS . Analysis of factors affecting angle ANB[J]. Am J Orthod, 1984,85(5):411-423. |
| [2] | Resnick CM, Kim S, Yorlets RR , et al. Evaluation of Andrews’ analysis as a predictor of ideal sagittal maxillary positioning in orthognathic surgery[J]. J Oral Maxillofac Surg, 2018,76(10):2169-2176. |
| [3] | Resnick CM, Daniels KM, Vlahos M . Does Andrews facial analysis predict esthetic sagittal maxillary position?[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2018,125(4):376-381. |
| [4] | Resnick CM, Calabrese CE, Resnick AS . Maxillary sagittal position in relation to the forehead: A target for orthognathic surgery[J]. J Craniofac Surg, 2018,29(3):688-691. |
| [5] | Jiang Z, Tan L, Hu L , et al. Clinician, dental student, and orthognathic patient perception of black-and-white silhouette lateral profile dimensions of ideal chin position in a Chinese population[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2018,125(1):e1-e7. |
| [6] | Ghaleb N, Bouserhal J, Bassil-Nassif N . Aesthetic evaluation of profile incisor inclination[J]. Eur J Orthod, 2011,33(3):228-235. |
| [7] | Webb MA, Cordray FE, Rossouw PE . Upper-incisor position as a determinant of the ideal soft-tissue profile[J]. J Clin Orthod, 2016,50(11):651-662. |
| [8] | Tourne LP, Bevis RL, Cavanaugh G . A validity test of cephalometric variables as a measure of clinical applicability in anteroposterior profile assessment[J]. Int J Adult Orthodon Orthognath Surg, 1993,8(2):95-112. |
| [9] | Tulloch C, Phillips C, Dann C . Cephalometric measures as indicators of facial attractiveness[J]. Int J Adult Orthodon Orthognath Surg, 1993,8(3):171-179. |
| [10] | 王涛 . Delaire颅颌面整体平衡理论与正颌外科策略[J]. 中国口腔颌面外科杂志, 2005,3(2):155-158. |
| [11] | Doğan S, Ertürk N . Delaire’s architectural and structural cranio-facial analysis in cephalometric evaluation[J]. Turkish J Orthod, 1989,2(1):103. |
| [12] | Bell WH, Ferraro JW . Modern practice in orthognathic and reconstructive surgery[J]. Plast Reconstr Surg, 1993,92(2):362. |
| [13] | Yang L, Xiao YD, Liang YJ , et al. Does the surgery-first approach produce better outcomes in orthognathic surgery? A systematic review and meta-analysis[J]. J Oral Maxillofac Surg, 2017,75(11):2422-2429. |
| [14] | Park JK, Choi JY, Yang IH , et al. Patient’s satisfaction in skeletal class Ⅲ cases treated with two-jaw surgery using orthognathic quality of life questionnaire: Conventional three-stage method versus surgery-first approach[J]. J Craniofac Surg, 2015,26(7):2086-2093. |
| [15] | Yamauchi K, Takahashi T, Yamaguchi Y , et al. Effect of “surgery first” orthognathic approach on temporomandibular symptoms and function: A comparison with “orthodontic first” approach[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2019,127(5):387-392. |
| [16] | Lo SH, Chen YA, Yao CF , et al. Is skeletal stability after bimaxillary surgery for skeletal class III deformity related to surgical occlusal contact?[J]. Int J Oral Maxillofac Surg, 2019,48(10):1329-1336. |
| [17] | Lee SH, Kil TJ, Park KR , et al. Three-dimensional architectural and structural analysis: A transition in concept and design from Delaire’s cephalometric analysis[J]. Int J Oral Maxillofac Surg, 2014,43(9):1154-1160. |
| [18] | 陈梦苇, 宋锦磷, 王涛 , 等. 重庆地区正常牙合人群颅颌面硬组织结构特征的Delaire头影测量初步研究[J]. 第三军医大学学报, 2008,30(4):351-354. |
| [19] | Tanaka JL, Ono E, Filho Medici E , et al. Influence of the facial pattern on ANB, AF-BF, and Wits appraisal[J]. World J Orthod, 2006,7(4):369-375. |
| [20] | 吴笑尘, 刘筱菁, 李自力 , 等. 一种头影测量分析法矢状向参考线在中国美貌人群中特点初探[J]. 中华口腔正畸学杂志, 2015,22(4):211-214. |
| [21] | Olate S, Zaror C, Blythe JN , et al. A systematic review of soft-to-hard tissue ratios in orthognathic surgery. Part Ⅲ: Double jaw surgery procedures[J]. J Craniomaxillofac Surg, 2016,44(10):1599-1606. |
| [22] | San Miguel Moragas J, Oth O, Buttner M , et al. A systematic review on soft-to-hard tissue ratios in orthognathic surgery part Ⅱ: Chin procedures[J]. J Craniomaxillofac Surg, 2015,43(8):1530-1540. |
| [1] | 蔡安东,王晓霞,周文娟,柳忠豪. 下颌前突畸形患者上颌骨及髁突虚拟位置与术后现实位置的比较[J]. 北京大学学报(医学版), 2024, 56(1): 74-80. |
| [2] | 徐心雨,吴灵,宋凤岐,李自力,张益,刘筱菁. 基于下颌运动轨迹的正颌外科术中下颌骨髁突定位方法及初步精度验证[J]. 北京大学学报(医学版), 2024, 56(1): 57-65. |
| [3] | 张雯,刘筱菁,李自力,张益. 基于解剖标志的鼻翼基底缩窄缝合术对正颌患者术后鼻唇部形态的影响[J]. 北京大学学报(医学版), 2023, 55(4): 736-742. |
| [4] | 吴灵,刘筱菁,李自力,王兴. 磨牙非中性关系与虚拟环境下拼对终末咬合精度[J]. 北京大学学报(医学版), 2018, 50(1): 154-159. |
| [5] | 王哲,朱榴宁,周琳,伊彪. 锥形束CT融合三维面像评估正颌术后软硬组织的变化[J]. 北京大学学报(医学版), 2016, 48(3): 544-549. |
| [6] | 何颖, 郭传瑸, 邓旭亮, 王兴, 王晓霞. 北方正常人群颅颌面三维比例测量及面部对称性分析[J]. 北京大学学报(医学版), 2015, 47(4): 708-713. |
| [7] | 陈硕, 刘筱菁, 李自力, 梁成, 王晓霞, 傅开元, 伊彪. 下颌后缩畸形患者正颌外科术后髁突改建的三维影像评价[J]. 北京大学学报(医学版), 2015, 47(4): 703-707. |
| [8] | 刘筱菁, 李倩倩, 田凯月, 王晓霞, 张益, 李自力. 陀螺仪记录转移自然头位系统的建立及其精度检测[J]. 北京大学学报(医学版), 2014, 46(1): 86-89. |
|
||