北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (1): 97-102. doi: 10.19723/j.issn.1671-167X.2020.01.015
β-磷酸三钙用于下颌第三磨牙拔除术后骨缺损修复的自身对照研究
- 北京大学口腔医学院·口腔医院,口腔颌面外科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100081
Application of β-TCP for bone defect restore after the mandibular third molars extraction: A split-mouth clinical trial
Chang CAO,Fei WANG,En-bo WANG( ),Yu LIU(
),Yu LIU( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
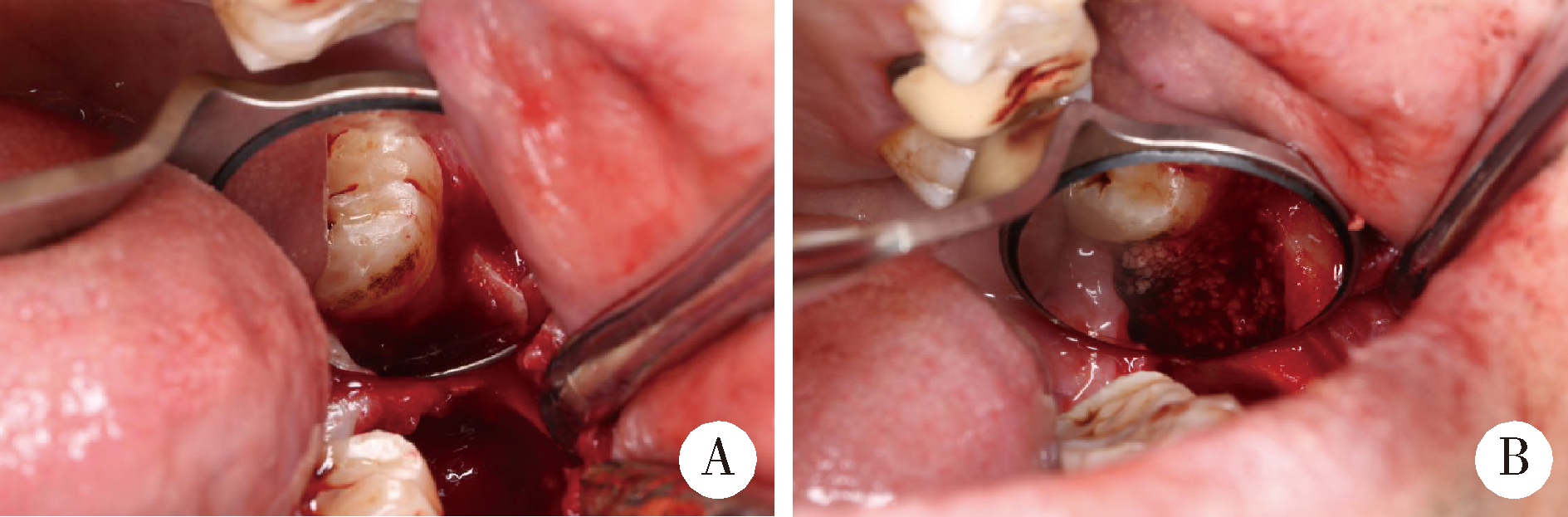
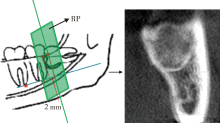
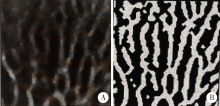
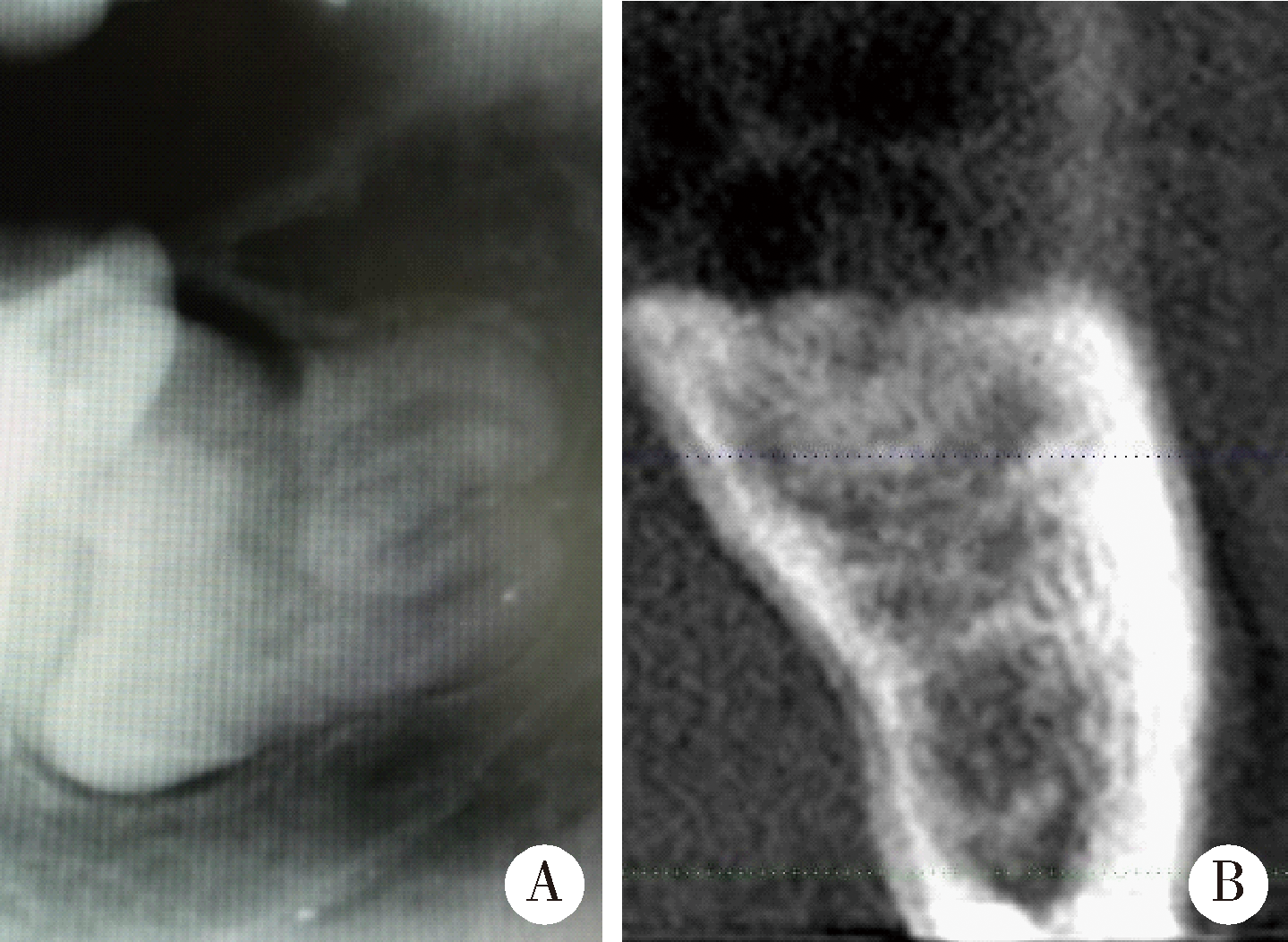
目的:评价β-磷酸三钙在下颌第三磨牙拔除后牙槽窝内的成骨效果,同时评价其对于第二磨牙远中牙周的预后效果。方法:选择2017年2月至6月在北京大学口腔医院口腔颌面外科就诊的15例双侧下颌第三磨牙水平阻生需拔除的患者,拔牙同时随机选择在一侧拔牙窝内植入β-磷酸三钙(easy-graft TMCLASSIC)作为实验组,另一侧自然愈合作为对照组。在拔牙术后1 d及术后6个月拍摄锥形束CT(cone beam computed tomography, CBCT), 比较试验组和对照组牙槽骨高度的变化,并利用MCTIPS软件计算形成新生骨的体积分数,术后6个月进行第二磨牙远中牙周探诊,记录远中颊侧探诊深度并进行统计学分析。结果:CBCT测量试验组新生骨体积分数为63.3%±2.2%, 对照组为50.1%±1.9%, 组间比较差异有统计学意义(P<0.05)。试验组牙槽骨高度变化量为(5.53±0.39) mm, 对照组牙槽骨高度变化量为(1.53±0.27) mm, 组间比较差异有统计学意义(P<0.05)。术后6个月,试验组第二磨牙远中颊角探诊深度为(3.0±0.7) mm,对照组为(6.6±0.8) mm,组间比较差异有统计学意义(P<0.05)。结论:应用β-磷酸三钙进行下颌第三磨牙拔除术后骨缺损修复可以显著增加下颌第二磨牙远中牙槽骨高度,并能促进拔牙窝内新生骨的形成,降低第二磨牙远中牙周袋探诊深度,具有良好的临床效果。
中图分类号:
- R782.1
| [1] | Kugelberg CF . Impacted lower third molars and periodontal health. An epidemiological, methodological, retrospective and prospective clinical study[J]. Swed Dent J Suppl, 1990,68:1-52. |
| [2] | Martin R, Louvrier A, Meyer C . Consequences of impacted wisdom teeth extraction on the periodontal environment of second molars, a pilot study[J]. J Stomatol Oral Maxillofac Surg, 2017,118(2):78-83 |
| [3] | Hassan KS, Marei HF, Alagl AS . Does grafting of third molar extraction sockets enhance periodontal measures in 30- to 35-year-old patients[J]. J Oral Maxillofac Surg, 2012,70(4):757-764. |
| [4] | Kanr P, Maria A . Eficacy of platelet rich plasma and hydroxyapatite crystals in bone regeneration after surgical removal of mandibular third molars[J]. Maxillofac Oral Surg, 2013,12(1):51-59. |
| [5] | Barbato L, Kalemaj Z, Buti J , et al. Effect of surgical intervention for removal of mandibular third molar on periodontal healing of adjacent mandibular second molar: a systematic review and bayesian network meta-analysis[J]. J Periodontol, 2016,87(3):291-302. |
| [6] | Tabrizi R . Use of lincomycin-impregnated demineralized freeze-dried bone allograft in the periodontal defect after third molar surgery[J]. J Oral Maxillofac Surg, 2014,72(5):850-857. |
| [7] | 刘树铭, 张祖燕, 李居朋 , 等. 健康青年人髁突松质骨结构锥形束CT分析[J]. 中华口腔医学杂志, 2007,42(6):357-360. |
| [8] | Kan KW, Liu JK, Lo EC , et al. Residual periodontal defects distal to the mandibular second molar 6-36 months after impacted third molar extraction[J]. J Clin Periodontol, 2002,29(11):1004-1011. |
| [9] | Leung WK, Corbet EF, Kan KW , et al. A regimen of systematic periodontal care after removal of impacted mandibular third molars manages periodontal pockets associated with the mandibular second molars[J]. J Clin Periodontol, 2005,32(7):725-731. |
| [10] | Qu HL, Tian BM, Chen FM , et al. Effect of asymptomatic visible third molars on periodontal health of adjacent second molars: a cross-sectional study.[J] J Oral Maxillofac Surg, 2017,75(10):2048-2057 |
| [11] | Faria AI, Gallas-Torreira M, Lσpez-Ratσn M . Mandibular second molar periodontal healing after impacted third molar extraction in young adults[J]. J Oral Maxillofac Surg, 2012,70(12):2732-2741. |
| [12] | Zimmerer RM, Jehn P, Kokemüller H , et al. In vivo tissue engineered bone versus autologous bone: stability and structure[J]. Int J Oral Maxillofac Surg, 2017,46(3):385-393. |
| [13] | Jensen T, Schou S, Stavropoulos A , et al. Maxillary sinus floor augmentation with Bio-Oss or Bio-Oss mixed with autogenous bone as graft: a systematic review[J]. Clin Oral Implants Res, 2012,23(3):263-273. |
| [14] | Ge J, Yang C, Zheng JW . Autogenous bone grafting for treatment of osseous defect after impacted mandibular third molar extraction: a randomized controlled trial[J]. Clin Implant Dent Relat Res, 2017,19(3):572-580. |
| [15] | Drosos GI, Kazakos KI, Kouzoumpasis P , et al. Safety and eficacy of commercially available demineralised bone matrix preparations: a critical review of clinical studies[J]. Injury, 2007,38(Suppl 41):S13-21. |
| [16] | Allen BA, Moudi E, Majidi MS , et al. A histologic, histomorphometric, and radiographic comparison between two complexes of CenoBoen/CenoMembrane and Bio-Oss/Bio-Gide in lateral ridge augmentation: a clinical trial[J]. Dent Res J (Isfahan), 2016,13(5):446-453. |
| [17] | Ogihara S, Tarnow DP . Efficacy of enamel matrix derivative with freeze-dried bone allograft or demineralized freeze-dried bone allograft in intrabony defects: a randomized trial[J]. J Periodontol, 2014,85(10):1351-1360. |
| [18] | Sammartino G, Tia M, Bucci T , et al. Prevention of mandibular third molar extraction-associated periodontal defects: a comparative study[J]. J Periodontol, 2009,80(3):389-396. |
| [19] | Miron RL, Sculean A, Cochran DL , et al. Twenty years of enamel matrix derivative: the past, the present and the future[J]. J Clin Periodontol, 2016,43(8):668-683. |
| [20] | Ho KN, Salamanca E, Chang KC , et al. A novel HA/β-TCP-collagen composite enhanced new bone formation for dental extraction socket preservation in beagle dogs[J]. Materials (Basel), 2016,9(3):191. |
| [21] | Arenaz-Búa J, Luaces-Rey R, Sironvalle-Soliva S , et al. A comparative study of platelet-rich plasma, hydroxyapatite, demineralized bone matrix and autologous bone to promote bone regeneration after mandibular impacted third molar extraction[J]. Med Oral Patol Oral Cir Bucal, 2010,15(3):e483-489. |
| [22] | Aloy-Prósper A, García-Mira B, Larrazabal-Morón C , et al. Distal probing depth and attachment level of lower second molars following surgical extraction of lower third molars: a literature review[J]. Med Oral Patol Oral Cir Bucal, 2010,15(5):e755-759. |
| [23] | Aimetti M, Romano F . Use of resorbable membranes in periodontal defects treatment after extraction of impacted mandibular third molars[J]. Minerva Stomatol, 2007,56(10):497-508. |
| [24] | Sammartino G, Tia M, Gentile E . Platelet-rich plasma and resorbable membrane for prevention of periodontal defects after deeply impacted lower third molar extraction[J]. J Oral Maxillofac Surg, 2009,67(11):2369-2373. |
| [25] | Moghe S, Saini N, Moghe A . Platelet-rich plasma in periodontal defect treatment after extraction of impacted mandibular third molars. Natl J Maxillofac Surg, 2012,3(2):139-143. |
| [26] | Montero J, Mazzaglia G . Effect of removing an impacted mandibular third molar on the periodontal status of the mandibular second molar[J]. J Oral Maxillofac Surg, 2011,69(11):2691-2697. |
| [27] | Kugelberg CF, Ahlström U, Ericson S , et al. The influence of anatomical, pathophysiological and other factors on periodontal healing after impacted lower third molar surgery a multiple regression analysis[J]. J Clin Periodontol, 1991,18(1):37-43. |
| [28] | Richardson DT, Dodson TB . Risk of periodontal defects after third molar surgery: an exercise in evidence-based clinical decision-making[J]. Oral Surg Oral Med Oral Path Oral Radiol Endod, 2005,100(2):133-137. |
| [29] | Osborne WH, Snyder AJ, Tempel TR . Attachment levels and crevicular depths at the distal of mandibular second molars following removal of adjacent third molars[J]. J Periodontol, 1982,53(2):93-95. |
| [30] | Chen YW, Lee CT, Chuang SK . Effect of flap design on periodontal healing after impacted third molar extraction: a systematic review and meta-analysis[J]. Int J Oral Maxillofac Surg, 2017,46(3):363-372. |
| [31] | Korkmaz YT, Mollaoglu N, Ozmeriç N . Does laterally rotated flap design influence the short-term periodontal status of second molars and postoperative discomfort after partially impacted third molar surgery[J]. J Oral Maxillofac Surg, 2015,73(6):1031-1041. |
| [32] | Kilinc A, Ataol M . How effective is collagen resorbable membrane placement after partially impacted mandibular third molar surgery on postoperative morbidity? A prospective randomized comparative study[J]. BMC Oral Health, 2017,17(1):126. |
| [1] | 薄士仕,高承志. 基于卷积神经网络实现锥形束CT牙齿分割及牙位标定[J]. 北京大学学报(医学版), 2024, 56(4): 735-740. |
| [2] | 黄莹,吴志远,周行红,蔡志刚,张杰. 股前外侧皮瓣修复上颌骨缺损术后面部软组织对称性感观分级[J]. 北京大学学报(医学版), 2023, 55(4): 708-715. |
| [3] | 章锦花,潘洁,孙志鹏,王霄. 不同根管内容物对口腔颌面锥形束CT诊断牙根纵裂准确性的影响[J]. 北京大学学报(医学版), 2023, 55(2): 333-338. |
| [4] | 潘孟乔,刘建,徐莉,徐筱,侯建霞,李小彤,王晓霞. 牙周-正畸-正颌联合治疗骨性安氏Ⅲ类错 |
| [5] | 叶佳学,梁宇红. 牙髓专科医师应用锥形束CT的现况调查[J]. 北京大学学报(医学版), 2023, 55(1): 114-119. |
| [6] | 高娟,吕航苗,马慧敏,赵一姣,李小彤. 锥形束CT三维体积测量评估骨性Ⅲ类错 |
| [7] | 刘伟涛,王怡然,王雪东,周彦恒. 锥形束CT研究上颌反复扩缩前方牵引后上颌骨缝的三维变化[J]. 北京大学学报(医学版), 2022, 54(2): 346-355. |
| [8] | 孟圆,张丽琪,赵雅宁,柳登高,张祖燕,高岩. 67例上颌根尖周囊肿的三维影像特点分析[J]. 北京大学学报(医学版), 2021, 53(2): 396-401. |
| [9] | 王京旗,王霄. 掺锶磷酸钙骨水泥材料生物学性能的动物实验[J]. 北京大学学报(医学版), 2021, 53(2): 378-383. |
| [10] | 康一帆,单小峰,张雷,蔡志刚. 游离腓骨瓣修复重建上颌骨术后腓骨瓣位置变化[J]. 北京大学学报(医学版), 2020, 52(5): 938-942. |
| [11] | 李博文,吴唯伊,唐琳,张一,刘玉华. 改良猪小肠黏膜下层可吸收膜在兔下颌骨缺损早期愈合中的作用[J]. 北京大学学报(医学版), 2019, 51(5): 887-892. |
| [12] | 谢晓艳,贾淑梅,孙志辉,张祖燕. 分辨率设置与锥形束CT检测牙根外吸收的可靠性[J]. 北京大学学报(医学版), 2019, 51(1): 75-79. |
| [13] | 赵一姣,刘怡,孙玉春,王勇. 一种基于曲率连续算法的冠、根三维数据融合方法[J]. 北京大学学报(医学版), 2017, 49(4): 719-723. |
| [14] | 章文博,于尧,王洋,刘筱菁,毛驰,郭传瑸,俞光岩,彭歆. 数字化外科技术在上颌骨缺损重建中的应用[J]. 北京大学学报(医学版), 2017, 49(1): 1-005. |
| [15] | 钟金晟, 欧阳翔英, 柳登高, 曹采方. 锥形束CT测量离体下颌磨牙Ⅱ°根分叉病变效果的评价[J]. 北京大学学报(医学版), 2010, 42(1): 41-45. |
|
||