北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (4): 697-703. doi: 10.19723/j.issn.1671-167X.2021.04.013
机器人辅助前列腺癌根治术后患者的控尿恢复时间
郝瀚,刘越,陈宇珂,司龙妹,张萌,范宇,张中元,唐琦,张雷,吴士良,宋毅,林健,赵峥,谌诚( ),虞巍,韩文科
),虞巍,韩文科
- 北京大学第一医院泌尿外科,北京大学泌尿外科研究所,国家泌尿、男性生殖系肿瘤研究中心,北京 100034
Evaluating continence recovery time after robot-assisted radical prostatectomy
HAO Han,LIU Yue,CHEN Yu-ke,SI Long-mei,ZHANG Meng,FAN Yu,ZHANG Zhong-yuan,TANG Qi,ZHANG Lei,WU Shi-liang,SONG Yi,LIN Jian,ZHAO Zheng,SHEN Cheng( ),YU Wei,HAN Wen-ke
),YU Wei,HAN Wen-ke
- National Urological Cancer Center, Beijing 100034, China
摘要:
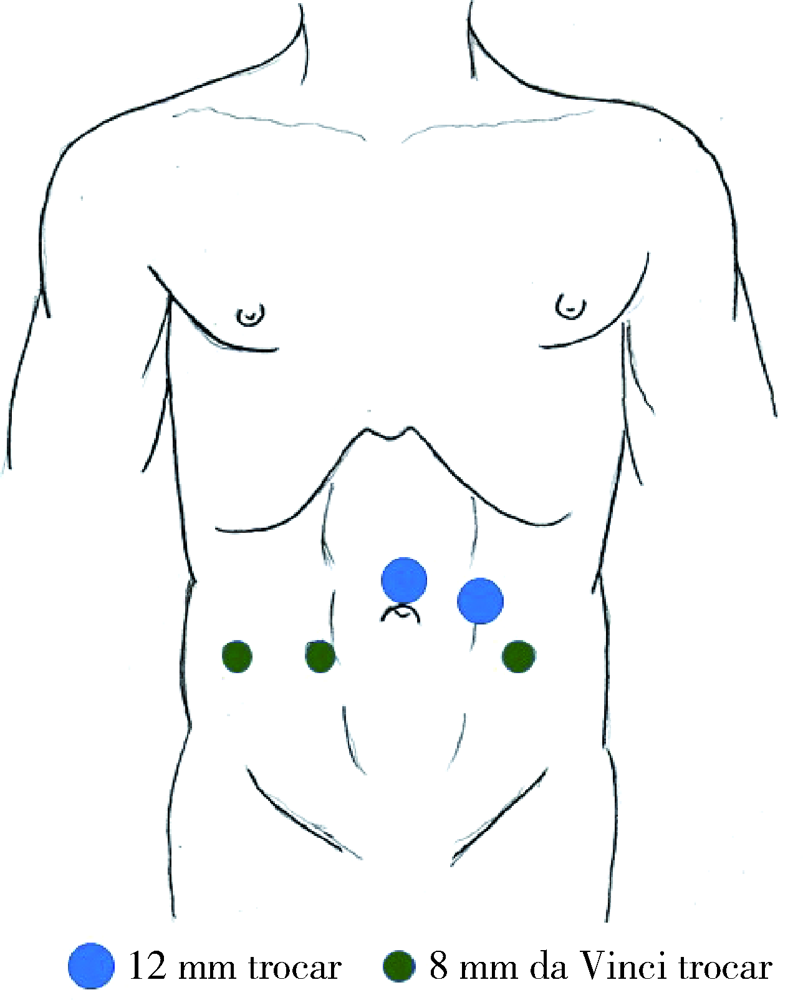
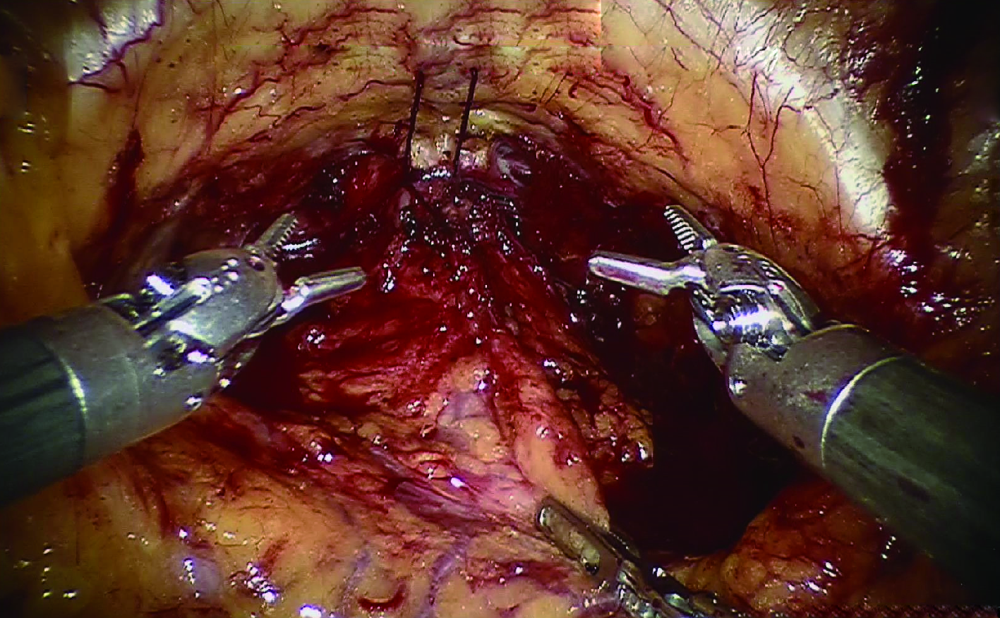
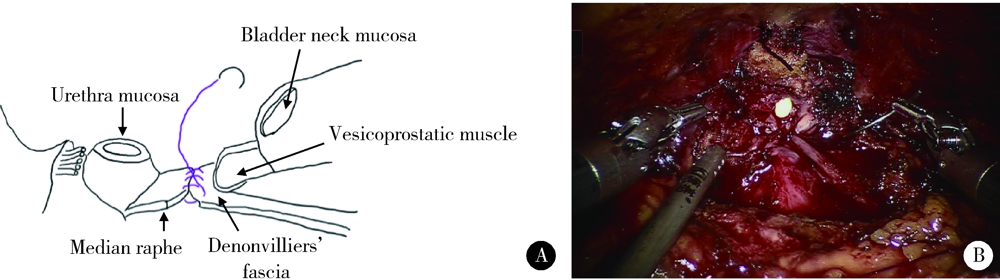
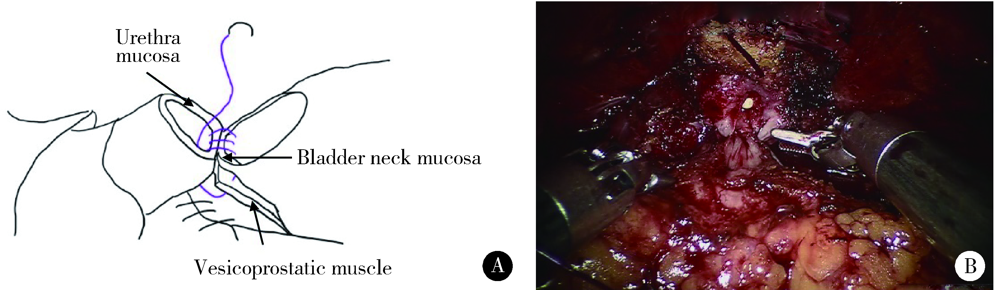
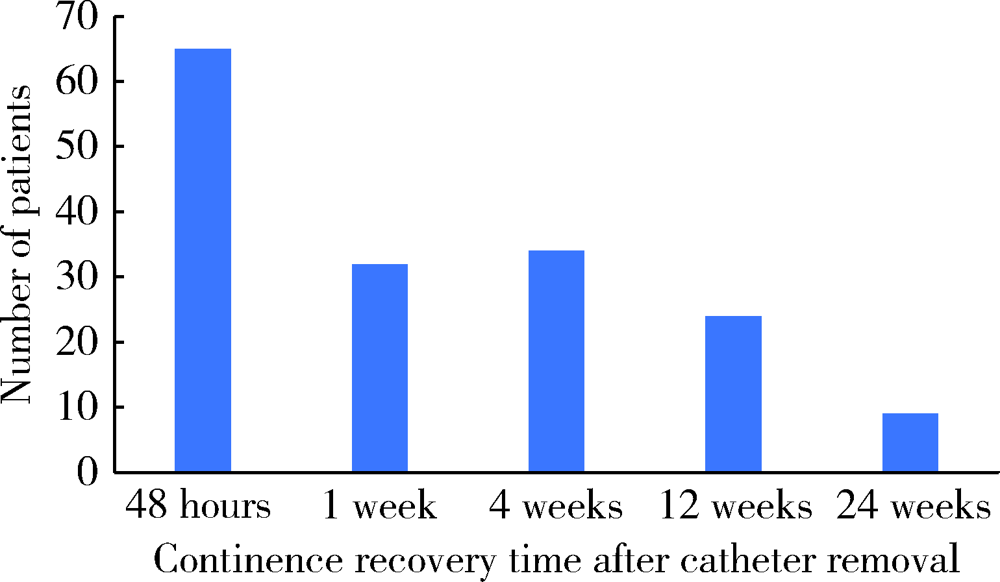
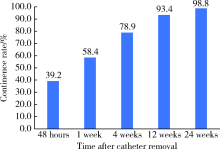
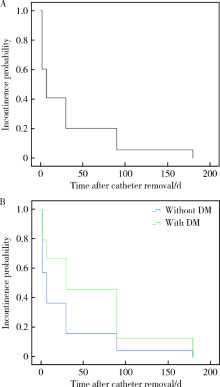
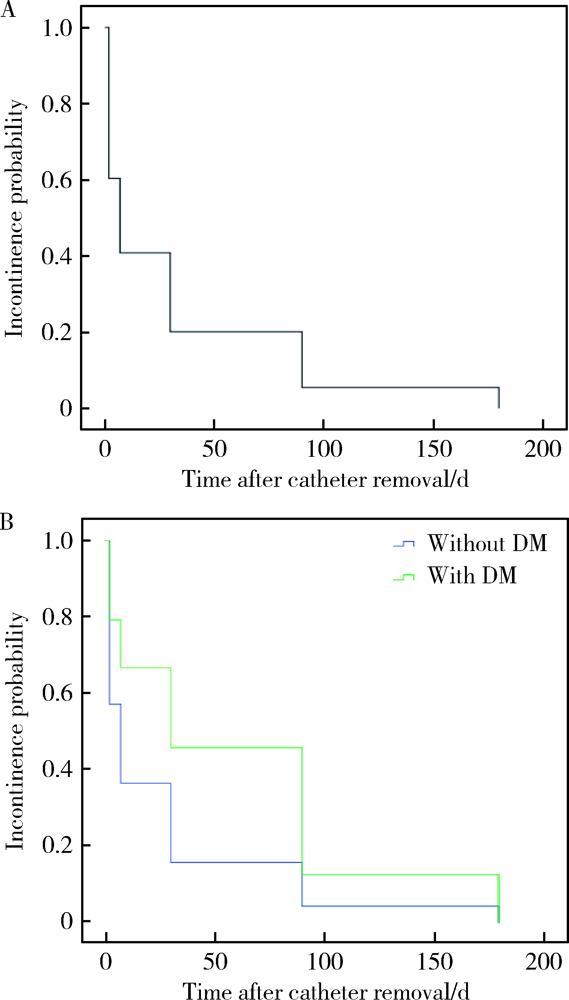
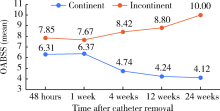
目的: 探讨机器人辅助前列腺癌根治术后控尿恢复时间及影响控尿恢复的危险因素。方法: 2019年1月至2021年1月,前瞻性收集北京大学第一医院泌尿外科单一术者行机器人辅助下前列腺癌根治及尿道周围全重建术的患者资料,纳入临床分期为cT1~T3、cN0、cM0的局限性前列腺癌患者。对于高危患者,常规行双侧盆腔淋巴结清扫。记录患者拔除尿管之后48 h、1周、4周、12周、24周后的控尿情况及相应时间节点的国际前列腺症状评分(international prostatic symptoms score,IPSS)和膀胱过度活动症状评分(overactive bladder symptom score,OABSS)。将24 h使用尿垫≤1片或24 h漏尿量≤20 g定义为完全自主控尿,记录患者拔除尿管之后至达到完全自主控尿的时间,并分析影响控尿恢复时间的危险因素。结果: 共有166例患者纳入本研究,入组患者平均年龄(66.2±6.7)岁,中位前列腺特异抗原(prostate specific antigen, PSA) 8.51 μg/L(4.69~13.20 μg/L)。共59例(35.5%)行双侧淋巴清扫,28例(16.9%)行保留性神经的手术。术后病理情况:pT1期1例(0.6%),pT2期77例(46.4%),pT3期86例(51.8%),28例患者切缘阳性(16.9%)。在所有行淋巴结清扫的患者中,有7例(11.9%)发现淋巴结转移。控尿情况:患者恢复控尿的中位时间为1周,65例(39.2%)患者在拔除尿管48 h之内即实现控尿,32例(19.3%)于术后1周内恢复控尿,34例(20.5%)于术后4周内恢复控尿,24例(14.5%)于术后12周内恢复控尿,9例(5.4%)术后24周内恢复控尿,有2例(1.2%)在术后24周时仍未恢复控尿。在拔除尿管后48 h、1周、4周、12周及24周时控尿率分别为39.2%、58.4%、78.9%、93.4%和98.8%。单因素COX回归分析显示,患者是否合并糖尿病是影响控尿恢复时间的危险因素(OR=1.589,95%CI:1.025~2.462,P=0.038)。在拔除尿管后48 h、4周、12周和24周时能够控尿组患者的平均OABSS均显著低于不能控尿组。结论: 机器人前列腺癌根治术后患者能够获得满意的早期控尿,糖尿病是影响术后控尿恢复时间的危险因素,拔除尿管后膀胱过度活动症状与能否控尿存在相关性。
中图分类号:
- R737.25
| [1] | 韩苏军, 张思维, 陈万青, 等. 中国前列腺癌发病现状和流行趋势分析 [J]. 临床肿瘤学杂志, 2013, 18(4):330-334. |
| [2] |
Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy [J]. Eur Urol, 2012, 62(3):405-417.
doi: 10.1016/j.eururo.2012.05.045 |
| [3] |
Patel VR, Abdul-Muhsin HM, Schatloff O, et al. Critical review of “pentafecta” outcomes after robot-assisted laparoscopic prostatectomy in high-volume centres [J]. BJU Int, 2011, 108(6 Pt 2):1007-1017.
doi: 10.1111/j.1464-410X.2011.10521.x |
| [4] |
Jeong SJ, Yi J, Chung MS, et al. Early recovery of urinary continence after radical prostatectomy: Correlation with vesico-urethral anastomosis location in the pelvic cavity measured by postoperative cystography [J]. Int J Urol, 2011, 18(6):444-451.
doi: 10.1111/j.1442-2042.2011.02760.x |
| [5] |
Skolarus TA, Hedgepeth RC, Zhang Y, et al. Does robotic technology mitigate the challenges of large prostate size? [J]. Urology, 2010, 76(5):1117-1121.
doi: 10.1016/j.urology.2010.03.060 pmid: 20708781 |
| [6] |
Link BA, Nelson R, Josephson DY, et al. The impact of prostate gland weight in robot assisted laparoscopic radical prostatectomy [J]. J Urol, 2008, 180(3):928-932.
doi: 10.1016/j.juro.2008.05.029 |
| [7] |
Shikanov S, Desai V, Razmaria A, et al. Robotic radical prostatectomy for elderly patients: probability of achieving continence and potency 1 year after surgery [J]. J Urol, 2010, 183(5):1803-1807.
doi: 10.1016/j.juro.2010.01.016 pmid: 20299041 |
| [8] |
Novara G, Ficarra V, D'Ella C, et al. Evaluating urinary continence and preoperative predictors of urinary continence after robot assisted laparoscopic radical prostatectomy [J]. J Urol, 2010, 184(3):1028-1033.
doi: 10.1016/j.juro.2010.04.069 pmid: 20643426 |
| [9] |
Porpiglia F, Bertolo R, Manfredi M, et al. Total anatomical reconstruction during robot-assisted radical prostatectomy: Implications on early recovery of urinary continence [J]. Eur Urol, 2016, 69(3):485-495.
doi: 10.1016/j.eururo.2015.08.005 |
| [10] |
Jønler M, Madsen FA, Rhodes PR, et al. A prospective study of quantification of urinary incontinence and quality of life in patients undergoing radical retropubic prostatectomy [J]. Urology, 1996, 48(3):433-440.
pmid: 8804498 |
| [11] |
Porpiglia F, Morra I, Lucci Chiarissi M, et al. Randomised controlled trial comparing laparoscopic and robot-assisted radical prostatectomy [J]. Eur Urol, 2013, 63(4):606-614.
doi: 10.1016/j.eururo.2012.07.007 |
| [12] |
Patel VR, Coelho RF, Palmer KJ, et al. Periurethral suspension stitch during robot-assisted laparoscopic radical prostatectomy: Description of the technique and continence outcomes [J]. Eur Urol, 2009, 56(3):472-478.
doi: 10.1016/j.eururo.2009.06.007 |
| [13] |
Sugimura Y, Hioki T, Yamada Y, et al. An anterior urethral stitch improves urinary incontinence following radical prostatectomy [J]. Int J Urol, 2001, 8(4):153-157.
pmid: 11260346 |
| [14] |
Noguchi M, Noda S, Nakashima O, et al. Suspension technique improves rapid recovery of urinary continence following radical retropubic prostatectomy [J]. Kurume Med J, 2004, 51(3/4):245-251.
doi: 10.2739/kurumemedj.51.245 |
| [15] |
Patel VR, Thaly R, Shan K. Robotic radical prostatectomy: Outcomes of 500 cases [J]. BJU Int, 2007, 99(5):1109-1112.
doi: 10.1111/bju.2007.99.issue-5 |
| [16] |
Rocco F, Carmignani L, Acquati P, et al. Early continence reco-very after open radical prostatectomy with restoration of the posterior aspect of the rhabdosphincter [J]. Eur Urol, 2007, 52(2):376-383.
doi: 10.1016/j.eururo.2007.01.109 |
| [17] |
Cakmak S, Canda AE, Ener K, et al. Does type 2 diabetes mellitus have an impact on postoperative early, mid-term and late-term urinary continence after robot-assisted radical prostatectomy? [J]. J Endourol, 2019, 33(3):201-206.
doi: 10.1089/end.2018.0822 |
| [18] | Huang J, Wang Y, An Y, et al. Impact of diabetes mellitus on urinary continence recovery after radical prostatectomy: A systematic review and meta-analysis [J]. Urol J, 2020, 18(2):136-143. |
| [1] | 张树栋,谢睿扬. 机器人手术时代的肾癌合并腔静脉瘤栓治疗策略[J]. 北京大学学报(医学版), 2024, 56(4): 562-564. |
| [2] | 邢念增,王明帅,杨飞亚,尹路,韩苏军. 前列腺免活检创新理念的临床实践及其应用前景[J]. 北京大学学报(医学版), 2024, 56(4): 565-566. |
| [3] | 于书慧,韩佳凝,钟丽君,陈聪语,肖云翔,黄燕波,杨洋,车新艳. 术前盆底肌电生理参数对前列腺癌根治性切除术后早期尿失禁的预测价值[J]. 北京大学学报(医学版), 2024, 56(4): 594-599. |
| [4] | 李雨清,王飚,乔鹏,王玮,关星. 经耻骨后尿道中段悬吊带术治疗女性复发性压力性尿失禁的中长期疗效[J]. 北京大学学报(医学版), 2024, 56(4): 600-604. |
| [5] | 应沂岑,杜毅聪,李志华,张一鸣,李新飞,王冰,张鹏,朱宏建,周利群,杨昆霖,李学松. 机器人辅助腹腔镜下颊黏膜补片输尿管成形术治疗复杂输尿管狭窄[J]. 北京大学学报(医学版), 2024, 56(4): 640-645. |
| [6] | 毛海,张帆,张展奕,颜野,郝一昌,黄毅,马潞林,褚红玲,张树栋. 基于MRI前列腺腺体相关参数构建腹腔镜前列腺癌术后尿失禁的预测模型[J]. 北京大学学报(医学版), 2023, 55(5): 818-824. |
| [7] | 张展奕,张帆,颜野,曹财广,李长剑,邓绍晖,孙悦皓,黄天亮,管允鹤,李楠,陆敏,胡振华,张树栋. 近红外荧光靶向探针用于前列腺神经血管束术中成像[J]. 北京大学学报(医学版), 2023, 55(5): 843-850. |
| [8] | 许素环,王蓓蓓,庞秋颖,钟丽君,丁炎明,黄燕波,车新艳. 等体温膀胱冲洗对经尿道前列腺电切术患者干预效果的meta分析[J]. 北京大学学报(医学版), 2023, 55(4): 676-683. |
| [9] | 周利群,徐纯如. 机器人时代中央型肾肿瘤的手术治疗策略[J]. 北京大学学报(医学版), 2022, 54(4): 587-591. |
| [10] | 左炜,高菲,袁昌巍,熊盛炜,李志华,张雷,杨昆霖,李新飞,刘靓,魏来,张鹏,王冰,谷亚明,朱宏建,赵峥,李学松. 基于多中心数据库的10年上尿路修复手术术式及术型变化趋势[J]. 北京大学学报(医学版), 2022, 54(4): 692-698. |
| [11] | 张帆,陈曲,郝一昌,颜野,刘承,黄毅,马潞林. 术前及术后膜性尿道长度与腹腔镜根治性前列腺切除术后控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2022, 54(2): 299-303. |
| [12] | 张帆,黄晓娟,杨斌,颜野,刘承,张树栋,黄毅,马潞林. 前列腺尖部深度与腹腔镜前列腺癌根治术后早期控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2021, 53(4): 692-696. |
| [13] | 程嗣达,李新飞,熊盛炜,樊书菠,王杰,朱伟杰,李子奡,丁光璞,俞婷,李万强,孙永明,杨昆霖,张雷,郝瀚,李学松,周利群. 机器人辅助腹腔镜上尿路修复手术:单一术者108例经验总结[J]. 北京大学学报(医学版), 2020, 52(4): 771-779. |
| [14] | 刘献辉,张维宇,胡浩,王起,王涛,贺永新,许克新. 耻骨后和经闭孔尿道中段悬吊术对不同分型压力性尿失禁疗效的长期随访[J]. 北京大学学报(医学版), 2019, 51(4): 694-697. |
| [15] | 车新艳,吴士良,陈宇珂,黄燕波,杨洋. 女性医务人员尿失禁及其对生活质量影响的现况调查[J]. 北京大学学报(医学版), 2019, 51(4): 706-710. |
|
||