北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (6): 1032-1036. doi: 10.19723/j.issn.1671-167X.2021.06.004
类风湿关节炎合并角膜溃疡的临床特点和相关因素分析
- 1.北京大学人民医院风湿免疫科,北京 100044
2.重庆市中西医结合康复医院康复科,重庆 400013
3.河北以岭医院风湿免疫科,石家庄 050091
4.北京大学人民医院眼科,北京 100044
Clinical characteristics and risk factors of rheumatoid arthritis with ulcerative keratitis
LUO Liang1,2,HUO Wen-gang3,ZHANG Qin4,△( ),LI Chun1,△(
),LI Chun1,△( )
)
- 1. Department of Rheumatology and Immunology, Peking University People’s Hospital, Beijing 100044, China
2. Department of Rehabilitation, Chongqing Rehabilitation Hospital of Integrated Traditional and Western, Chongqing 400013, China
3. Department of Rheumatology and Immunology, Hebei Yiling Hospital, Shijiazhuang 050091, China
4. Department of Ophthalmology, Peking University People's Hospital, Beijing 100044, China
摘要:
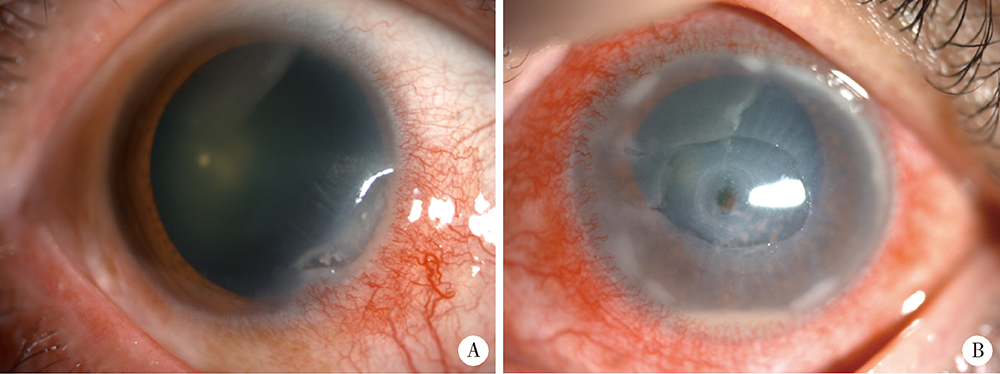
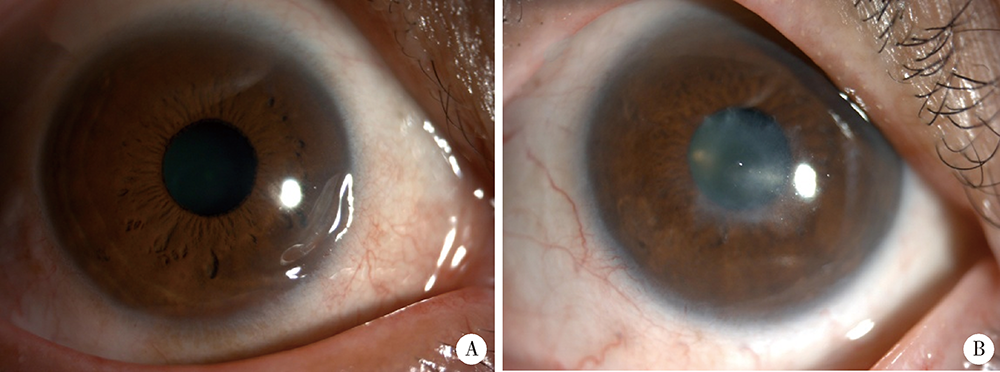
目的:探讨类风湿关节炎(rheumatoid arthritis,RA)合并角膜溃疡(ulcerative keratitis,UK)的临床特点、相关因素及临床转归。方法:选取2003年1月至2021年5月于北京大学人民医院住院的RA患者4 773例,筛选出合并UK的患者16例(UK组),通过倾向性评分匹配(propensity score matching,PSM), 选取无UK的对照组患者72例。对PSM后的两组患者的临床及实验室资料进行统计和分析。结果:RA合并UK表现为单纯边缘性UK 8例、边缘性UK伴穿孔5例、边缘性UK伴葡萄膜炎2例、中央性UK伴穿孔1例。UK组肿胀关节数显著高于对照组[6.0(2.5,23.0) vs. 3.0(1.0, 9.8),Z=-2.047,P=0.041],UK组继发干燥综合征(Sjögren syndrome,SS)的比例(37.5% vs. 6.9%, χ2=11.175,P=0.004)及间质性肺炎(interstitial lung disease,ILD,37.5% vs. 8.3%, χ2=9.456,P=0.008)的比例显著高于对照组,柳氮磺吡啶(12.5% vs. 48.6%, χ2=7.006,P=0.008)、来氟米特(31.3% vs. 63.9%, χ2=5.723,P=0.017)及金制剂(6.3% vs. 33.8%, χ2=4.841,P=0.032)的使用率显著低于对照组。回归分析显示肿胀关节数(OR=1.148)、继发SS(OR=79.118)、合并ILD(OR=6.596)及柳氮磺吡啶的使用(OR=0.037)与RA合并UK的发生存在独立相关性(P<0.05)。结论:UK为RA的少见并发症,多为边缘性UK。肿胀关节数、继发SS、合并ILD及柳氮磺吡啶的使用与RA合并UK发生存在独立相关性。
中图分类号:
- R593.22
| [1] | Jayaraj K, Alvin G, Charles S, et al. Correlation of ocular manifestations with the duration and activity of disease in patients with rheumatoid arthritis[J]. Int J Med Sci, 2017, 6(1):34-37. |
| [2] | Hamideh F, Prete P. Ophthalmologic manifestations of rheumatic diseases[J]. Semin Arthritis Rheum, 2001, 30(4):217-241. |
| [3] |
Foster CS, Forstot SL, Wilson LA. Mortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis: effects of systemic immune suppression[J]. Ophthalmology, 1984, 91(10):1253-1263.
pmid: 6514289 |
| [4] |
Zandavalli F, Castro G, Mazzucco M, et. al. Infliximab is effective in difficult-to-control peripheral ulcerative keratitis. A report of three cases[J]. Rev Bras Reumatol, 2015, 55(3):310-312.
doi: 10.1016/j.rbr.2014.05.006 pmid: 25440698 |
| [5] |
Aletaha D, Neogi T, Silman J, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology / European League Against Rheumatism Collaborative Initiative[J]. Arthritis Rheum, 2010, 62(9):2569-2581.
doi: 10.1002/art.27584 |
| [6] | Yoshida M, Hariya T, Yokokura S, et al. Concomitant herpes simplex keratitis and autoimmune-associated ulcerative keratitis in rheumatoid arthritis patients[J]. Am J Ophthalmol Case Rep, 2020, 18:100648. |
| [7] |
Artifoni M, Rothschild R, Brézin A, et al. Ocular inflammatory diseases associated with rheumatoid arthritis[J]. Nat Rev Rheumatol, 2014, 10(2):108-116.
doi: 10.1038/nrrheum.2013.185 pmid: 24323074 |
| [8] |
Watanabe R, Ishii T, Yoshida M, et al. Ulcerative keratitis in patients with rheumatoid arthritis in the modern biologic era: a series of eight cases and literature review[J]. Int J Rheum Dis, 2017, 20(2):225-230.
doi: 10.1111/1756-185X.12688 pmid: 26179634 |
| [9] |
Harrold R, Shan Y, Rebello S, et al. Prevalence of Sjögren’s syndrome associated with rheumatoid arthritis in the USA: an observational study from the Corrona registry[J]. Clin Rheumatol, 2020, 39(6):1899-1905.
doi: 10.1007/s10067-020-05004-8 pmid: 32130579 |
| [10] |
Singh S, Das V, Basu S. Ocular involvement in Sjögren syndrome: risk factors for severe visual impairment and vision-threatening corneal complications[J]. Am J Ophthalmol, 2021, 225:11-17.
doi: 10.1016/j.ajo.2020.12.019 |
| [11] |
Maseda D, Bonami R, Crofford L. Regulation of B lymphocytes and plasma cells by innate immune mechanisms and stromal cells in rheumatoid arthritis[J]. Expert Rev Clin Immunol, 2014, 10(6):747-762.
doi: 10.1586/1744666X.2014.907744 |
| [12] |
Galor A, Thorne J. Scleritis and peripheral ulcerative keratitis[J]. Rheum Dis Clin North Am, 2007, 33(4):835-854.
doi: 10.1016/j.rdc.2007.08.002 |
| [13] | Wang F, Misra L, Patel V. In vivo confocal microscopy of the human cornea in the assessment of peripheral neuropathy and systemic diseases[J]. Biomed Res Int, 2015, 2015:951081. |
| [14] |
Sainz M, Foster S, Jabbur S, et al. Ocular characteristics and disease associations in scleritis-associated peripheral keratopathy[J]. Arch Ophthalmol, 2002, 120(1):15-19.
doi: 10.1001/archopht.120.1.15 |
| [15] |
Knox NE, Tole DM, Georgoudis P, et al. Peripheral ulcerative keratitis and corneal melt: a 10-year single center review with historical comparison[J]. Cornea, 2014, 33(1):27-31.
doi: 10.1097/ICO.0000000000000008 |
| [16] | 祝磊, 王丽娅, 张俊杰, 等. 0.05%他克莫司滴眼液治疗难治性免疫相关角膜溃疡的疗效及安全性研究[J]. 中华实验眼科杂志, 2015, 33(9):823-827. |
| [17] | 杨纪忠, 李冰. 类风湿关节炎相关性边缘角膜溃疡临床分析[J]. 山西医药杂志, 2009, 38(8):748-749. |
| [18] |
Bonnet I, Rousseau A, Duraffour P, et al. Efficacy and safety of rituximab in peripheral ulcerative keratitis associated with rheumatoid arthritis[J]. RMD Open, 2021, 7(1):e001472.
doi: 10.1136/rmdopen-2020-001472 |
| [19] |
Lucia D, Lara S, Vanesa R, et al. Biologic therapy in severe and refractory peripheral ulcerative keratitis (PUK). Multicenter study of 34 patients[J]. Semin Arthritis Rheum, 2020, 50(4):608-615.
doi: 10.1016/j.semarthrit.2020.03.023 |
| [20] |
Puéchal X, Gottenberg E, Berthelot M, et al. Rituximab therapy for systemic vasculitis associated with rheumatoid arthritis: results from the autoimmunity and rituximab registry[J]. Arthritis Care Res, 2012, 64(3):331-339.
doi: 10.1002/acr.20689 |
| [21] |
Peter K, Dirk B, Susann A, et al. Rapid healing of peripheral ulcerative keratitis in rheumatoid arthritis with prednisone, methotrexate and adalimumab combination therapy[J]. Rheumatology (Oxford), 2017, 56(7):1094.
doi: 10.1093/rheumatology/kex007 |
| [22] |
Messmer M, Foster S. Vasculitic peripheral ulcerative keratitis[J]. Surv Ophthalmol, 1999, 43(5):379-396.
pmid: 10340557 |
| [23] |
Messmer M, Foster S. Destructive corneal and scleral disease associated with rheumatoid arthritis: medical and surgical management[J]. Cornea, 1995, 14(4):408-417.
pmid: 7671613 |
| [1] | 刘东武, 陈杰, 高明利, 于静. 类风湿关节炎伴发淋巴结Castleman样病理改变1例[J]. 北京大学学报(医学版), 2024, 56(5): 928-931. |
| [2] | 黄会娜,赵静,赵祥格,白自然,李霞,王冠. 乳酸对类风湿关节炎患者外周血CD4+T细胞亚群的调控作用[J]. 北京大学学报(医学版), 2024, 56(3): 519-525. |
| [3] | 汤晓菲,李永红,丁秋玲,孙卓,张阳,王育梅,田美伊,刘坚. 类风湿关节炎患者下肢深静脉血栓发病率及危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 279-283. |
| [4] | 邹雪,白小娟,张丽卿. 艾拉莫德联合托法替布治疗难治性中重度类风湿关节炎的疗效[J]. 北京大学学报(医学版), 2023, 55(6): 1013-1021. |
| [5] | 吴琦,蔡月明,何娟,黄文蒂,王庆文. 血脂异常与类风湿关节炎肺间质病变的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 982-992. |
| [6] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 体重指数与类风湿关节炎临床特征的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 993-999. |
| [7] | 金银姬,孙琳,赵金霞,刘湘源. 血清IgA型抗鼠科肉瘤病毒癌基因同源物B1抗体在类风湿关节炎中的意义[J]. 北京大学学报(医学版), 2023, 55(4): 631-635. |
| [8] | 蔡文心,李仕成,刘一鸣,梁如玉,李静,郭建萍,胡凡磊,孙晓麟,李春,刘栩,叶华,邓立宗,李茹,栗占国. 类风湿关节炎临床分层及其特征的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1068-1073. |
| [9] | 程昉,杨邵英,房星星,王璇,赵福涛. CCL28-CCR10通路在类风湿关节炎单核细胞迁移中的作用[J]. 北京大学学报(医学版), 2022, 54(6): 1074-1078. |
| [10] | 刘蕊,赵金霞,闫良. 类风湿关节炎合并下肢静脉血栓患者的临床特点[J]. 北京大学学报(医学版), 2022, 54(6): 1079-1085. |
| [11] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 类风湿关节炎患者生活质量与疾病活动度的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1086-1093. |
| [12] | 侯国进,周方,田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮. 外侧锁定接骨板治疗股骨远端骨折术后翻修的相关影响因素[J]. 北京大学学报(医学版), 2022, 54(6): 1172-1177. |
| [13] | 高超,陈立红,王莉,姚鸿,黄晓玮,贾语博,刘田. 类风湿关节炎合并纤维肌痛简易分类标准的临床验证[J]. 北京大学学报(医学版), 2022, 54(2): 278-282. |
| [14] | 娄雪,廖莉,李兴珺,王楠,刘爽,崔若玫,徐健. 类风湿关节炎患者外周血TWEAK基因启动子区甲基化状态及其表达[J]. 北京大学学报(医学版), 2021, 53(6): 1020-1025. |
| [15] | 钟华,徐丽玲,白明欣,苏茵. 类风湿关节炎患者趋化因子CXCL9和CXCL10在骨侵蚀中的作用[J]. 北京大学学报(医学版), 2021, 53(6): 1026-1031. |
|
||