北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (6): 1144-1151. doi: 10.19723/j.issn.1671-167X.2021.06.023
不同转流标准对颈动脉内膜切除术后脑梗死的影响
白鹏1,王涛2,周阳1,陶立元3,李刚1,李正迁1,郭向阳1,△( )
)
- 1.北京大学第三医院 麻醉科, 北京 100191
2.北京大学第三医院 神经外科, 北京 100191
3.北京大学第三医院 临床流行病研究中心,北京 100191
Effect of different shunt strategies on cerebral infarction after carotid endarterectomy
BAI Peng1,WANG Tao2,ZHOU Yang1,TAO Li-yuan3,LI Gang1,LI Zheng-qian1,GUO Xiang-yang1,△( )
)
- 1. Department of Anesthesiology, Peking University Third Hospital, Beijing 100191, China
2. Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
3. Clinical Epidemiology Research Center, Peking University Third Hospital, Beijing 100191, China
摘要:
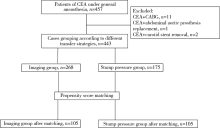
目的:颈动脉内膜切除术 (carotid endarterectomy, CEA)的麻醉管理要点是颈动脉阻断期间维持足够的颅脑灌注,放置转流管是外科常用方法之一,分析CEA手术不同转流标准对术后脑梗死的影响。方法:回顾收集2年内全身麻醉下接受CEA手术的443例患者,根据不同转流标准分为影像组 (以术前影像学资料作为是否转流的依据)和残端压组 (以术中残端压作为是否转流的依据)。分析患者术前人口学资料、既往病史、颈部血管狭窄程度、围术期各时间点血压情况、血管阻断时间、是否放置转流管、术后住院时间、住院期间脑梗死和其他不良事件,进行组间对比,在此基础上对组间差异有统计学意义的术前、术中情况进行倾向性评分匹配,分析不同转流标准对术后发生脑梗死的影响。结果:影像组患者268例、残端压组患者175例均接受全身麻醉下CEA手术,两组间基本情况和各时间点血压差异有统计学意义。经倾向性评分匹配后,匹配出影像组和残端压组各105例患者,两组患者的术前基本情况、各时间点血压差异无统计学意义。两组患者术后脑梗死发生率差异无统计学意义 (1.9% vs. 1.0%,P>0.999), 影像组术中转流率明显低于残端压组 (0 vs. 22.9%, P<0.001),影像组患者术后住院时间8 (7, 8) d明显长于残端压组5 (4, 6) d (P<0.001)。结论:依据术前影像学检查决定是否转流的患者组中,术中转流管使用率低于依据术中残端压决定是否转流的患者组,两组患者术后住院期间脑梗死的发生率差异无统计学意义,不同转流标准对患者脑梗死的影响有待于进一步深入研究。
中图分类号:
- R651.12
| [1] |
Petty GW, Brown RD Jr, Whisnant JP, et al. Ischemic stroke subtypes: A population-based study of incidence and risk factors[J]. Stroke, 1999, 30(12):2513-2516.
pmid: 10582970 |
| [2] |
Kret MR, Young B, Moneta GL, et al. Results of routine shunting and patch closure during carotid endarterectomy[J]. Am J Surg, 2012, 203(5):613-617.
doi: 10.1016/j.amjsurg.2011.12.005 |
| [3] |
Aburahma AF, Mousa AY, Stone PA. Shunting during carotid endarterectomy[J]. J Vasc Surg, 2011, 54(5):1502-1510.
doi: 10.1016/j.jvs.2011.06.020 pmid: 21906905 |
| [4] |
Samson RH, Cline JL, Showalter DP, et al. Contralateral carotid artery occlusion is not a contraindication to carotid endarterectomy even if shunts are not routinely used[J]. J Vasc Surg, 2013, 58(4):935-940.
doi: 10.1016/j.jvs.2013.04.011 |
| [5] |
Aburahma AF, Stone PA, Hass SM, et al. Prospective rando-mized trial of routine versus selective shunting in carotid endarterectomy based on stump pressure[J]. J Vasc Surg, 2010, 51(5):1133-1138.
doi: 10.1016/j.jvs.2009.12.046 pmid: 20347544 |
| [6] | Rerkasem K, Rothwell PM. Routine or selective carotid artery shunting for carotid endarterectomy and different methods of monitoring in selective shunting[J]. Stroke, 2010, 41(1):e53-e54 |
| [7] |
Lichtman JH, Jones MR, Leifheit EC, et al. Carotid endarterectomy and carotid artery stenting in the US medicare population, 1999-2014[J]. JAMA, 2017, 318(11):1035-1046.
doi: 10.1001/jama.2017.12882 pmid: 28975306 |
| [8] |
Wiske C, Arhuidese I, Malas M, et al. Comparing the efficacy of shunting approaches and cerebral monitoring during carotid endarterectomy using a national database[J]. J Vasc Surg, 2018, 68(2):416-425.
doi: S0741-5214(18)30035-1 pmid: 29571621 |
| [9] |
Banga PV, Varga A, Csobay-Novák C, et al. Incomplete circle of Willis is associated with a higher incidence of neurologic events during carotid eversion endarterectomy without shunting[J]. J Vasc Surg, 2018, 68(6):1764-1771.
doi: 10.1016/j.jvs.2018.03.429 |
| [10] | 中华医学会外科学分会血管外科学组. 颈动脉狭窄诊治指南[J]. 中国血管外科杂志, 2017, 9(3):169-175. |
| [11] |
Kolkert JLP, Groenwold RHH, Leijdekkers VJ, et al. Cost-effectiveness of two decision strategies for shunt use during carotid endarterectomy[J]. World J Surg, 2017, 41(11):2959-2967.
doi: 10.1007/s00268-017-4085-5 pmid: 28623598 |
| [12] | 李攀峰, 王兵, 崔文军, 等. 对侧颈动脉狭窄程度对颈动脉内膜剥脱术中转流管应用的影响[J]. 实用医学杂志, 2015, 31(10):1639-1641. |
| [13] |
Huibers A, Calvet D, Kennedy F, et al. Mechanism of procedural stroke following carotid endarterectomy or carotid artery stenting within the International Carotid Stenting Study (ICSS) randomised trial[J]. Eur J Vasc Endovasc Surg, 2015, 50(3):281-288.
doi: 10.1016/j.ejvs.2015.05.017 |
| [14] |
Spagnoli LG, Mauriello A, Sangiorgi G, et al. Extracranial thrombotically active carotid plaque as a risk factor for ischemic stroke[J]. JAMA, 2004, 292(15):1845-1852.
pmid: 15494582 |
| [15] | 刁永鹏, 刘昌伟, 宋小军, 等. 颈动脉内膜剥脱术治疗老年颈动脉狭窄患者的危险因素分析[J]. 中华普通外科杂志, 2014, 29(6):448-451. |
| [1] | 李晋娜,许丽娜,李敏,宋怡,张静,贾龙斌. 急性脑梗死患者血清BDNF、IL-18、hs-CRP水平与血管性认知障碍的相关性[J]. 北京大学学报(医学版), 2024, 56(4): 708-714. |
| [2] | 范常锋,黄亚平,李霞,陈芸,李真,乔淑冬. 以发作性体位性视物双影为前期症状的后循环卒中1例[J]. 北京大学学报(医学版), 2023, 55(4): 762-765. |
| [3] | 刘颖,霍然,徐慧敏,王筝,王涛,袁慧书. 磁共振血管壁成像评估颈动脉中重度狭窄患者斑块特征与脑血流灌注的相关性[J]. 北京大学学报(医学版), 2023, 55(4): 646-651. |
| [4] | 贾子昌,李选,郑梅,栾景源,王昌明,韩金涛. 复合手术治疗无残端的症状性长段颈内动脉慢性闭塞[J]. 北京大学学报(医学版), 2020, 52(1): 177-180. |
| [5] | 赵海燕,樊东升,韩金涛. 重度颈内动脉狭窄伴未破裂动脉瘤的治疗策略[J]. 北京大学学报(医学版), 2019, 51(5): 829-834. |
| [6] | 李金勇,孙宏亮,叶志东,樊雪强,刘鹏. 颈动脉斑块成分和体积的多排螺旋计算机断层扫描血管成像技术评价[J]. 北京大学学报(医学版), 2018, 50(5): 833-839. |
| [7] | 韩金涛,李选,和清源,赵海燕,叶珊,董国祥,栾景源,王昌明. 脑动脉串联病变的同期腔内治疗[J]. 北京大学学报(医学版), 2016, 48(1): 149-153. |
| [8] | 王云云,孙葳,黄一宁. 颈椎病误诊为脑梗死1例[J]. 北京大学学报(医学版), 2015, 47(5): 883-884. |
| [9] | 韩金涛,赵海燕,李选,和清源,叶珊,董国祥,傅军,栾景源,王昌明,李天润. 颈动脉支架成形术血流动力学损害的相关因素分析[J]. 北京大学学报(医学版), 2015, 47(5): 804-808. |
| [10] | 韩金涛, 李选, 郑梅, 傅军, 王昌明, 董国祥, 和清源. 大脑中动脉成形术治疗中、重度残疾的皮质下分水岭梗死的临床观察[J]. 北京大学学报(医学版), 2014, 46(4): 606-611. |
| [11] | 梁建涛, 王振宇. 脑动脉狭窄患者血清中炎性因子干扰素-γ、白细胞介素-6和肿瘤坏死因子-α的水平分析[J]. 北京大学学报(医学版), 2011, 43(6): 837-840. |
| [12] | 杨敏, 宋莉, 王健, 佟小强, 邹英华. 颈动脉支架术伴重度低血流动力学状态患者的药物治疗[J]. 北京大学学报(医学版), 2009, 41(3): 373-375. |
| [13] | 吕鹤, 姚生, 张巍, 王朝霞, 黄一宁, 牛小媛, 张茁, 袁云. 4个常染色体显性遗传性脑动脉病伴皮层下梗死和白质脑病(CADASIL)家族的临床表现[J]. 北京大学学报(医学版), 2004, 36(5): 496-500. |
| [14] | 赵淑清, 肖卫忠, 李坚, 张新宇, 王宏利, 孙庆利, 张俊. 急性脑梗死合并SARS 1例报告[J]. 北京大学学报(医学版), 2003, 35(z1): 142-142. |
|
||