北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (4): 705-711. doi: 10.19723/j.issn.1671-167X.2022.04.020
原发性干燥综合征合并甲状腺功能减退眼表状态评估
于昊哲1,曾唯珍1,吴文雨1,姚中强2,*( ),冯云1,*(
),冯云1,*( )
)
- 1. 北京大学第三医院眼科,北京 100191
2. 北京大学第三医院风湿免疫科,北京 100191
Evaluation of ocular surface status and function in primary Sjögren's syndrome with hypothyroidism
Hao-zhe YU1,Wei-zhen ZENG1,Wen-yu WU1,Zhong-qiang YAO2,*( ),Yun FENG1,*(
),Yun FENG1,*( )
)
- 1. Department of Ophthalmology, Peking University Third Hospital, Beijing 100191, China
2. Department of Rheumatology and Immunology, Peking University Third Hospital, Beijing 100191, China
摘要:
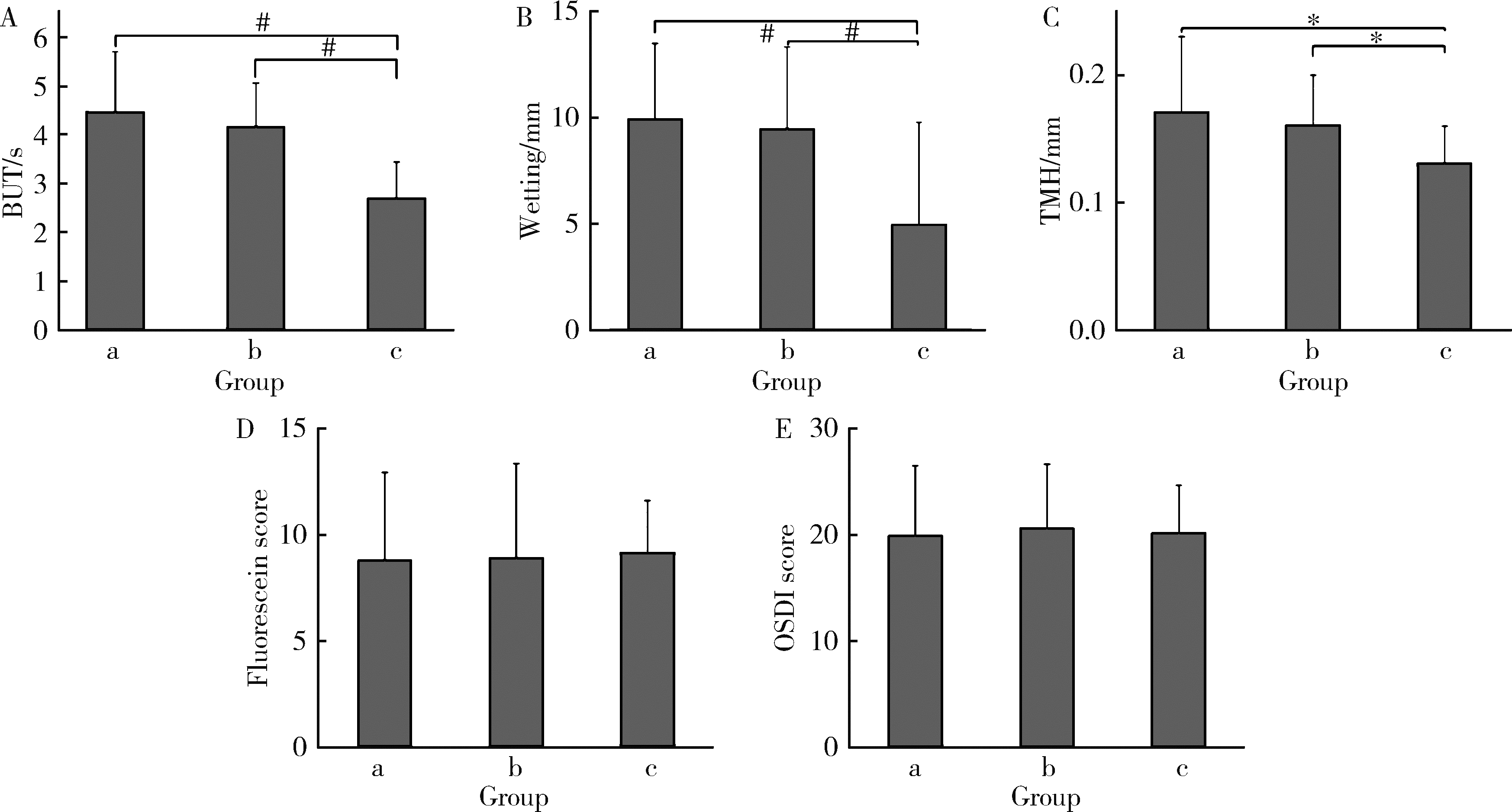
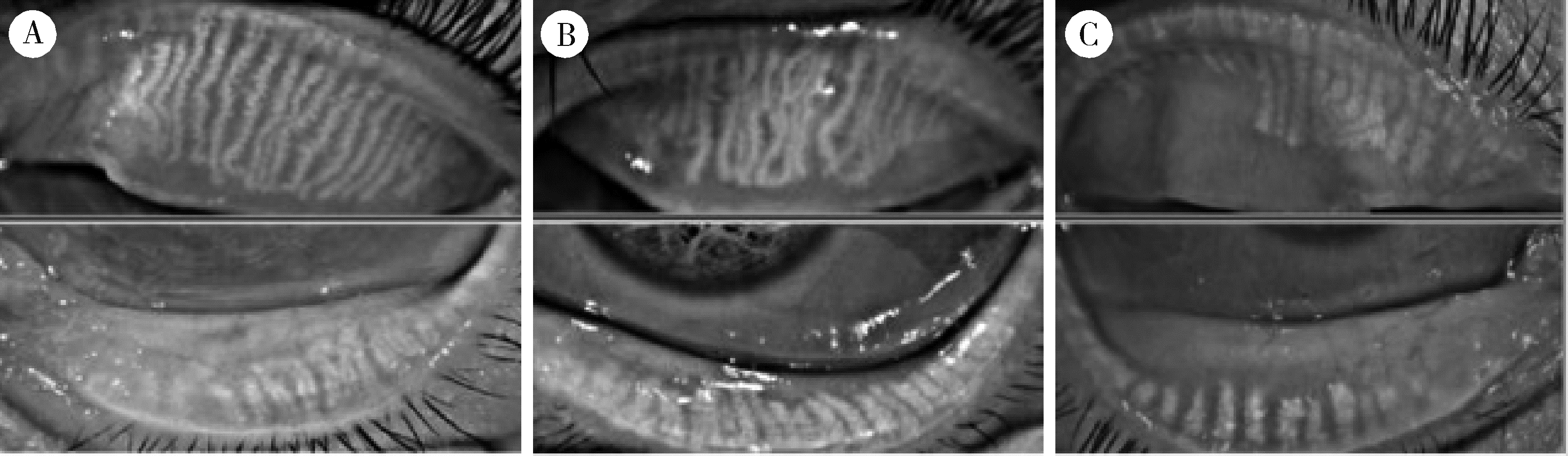
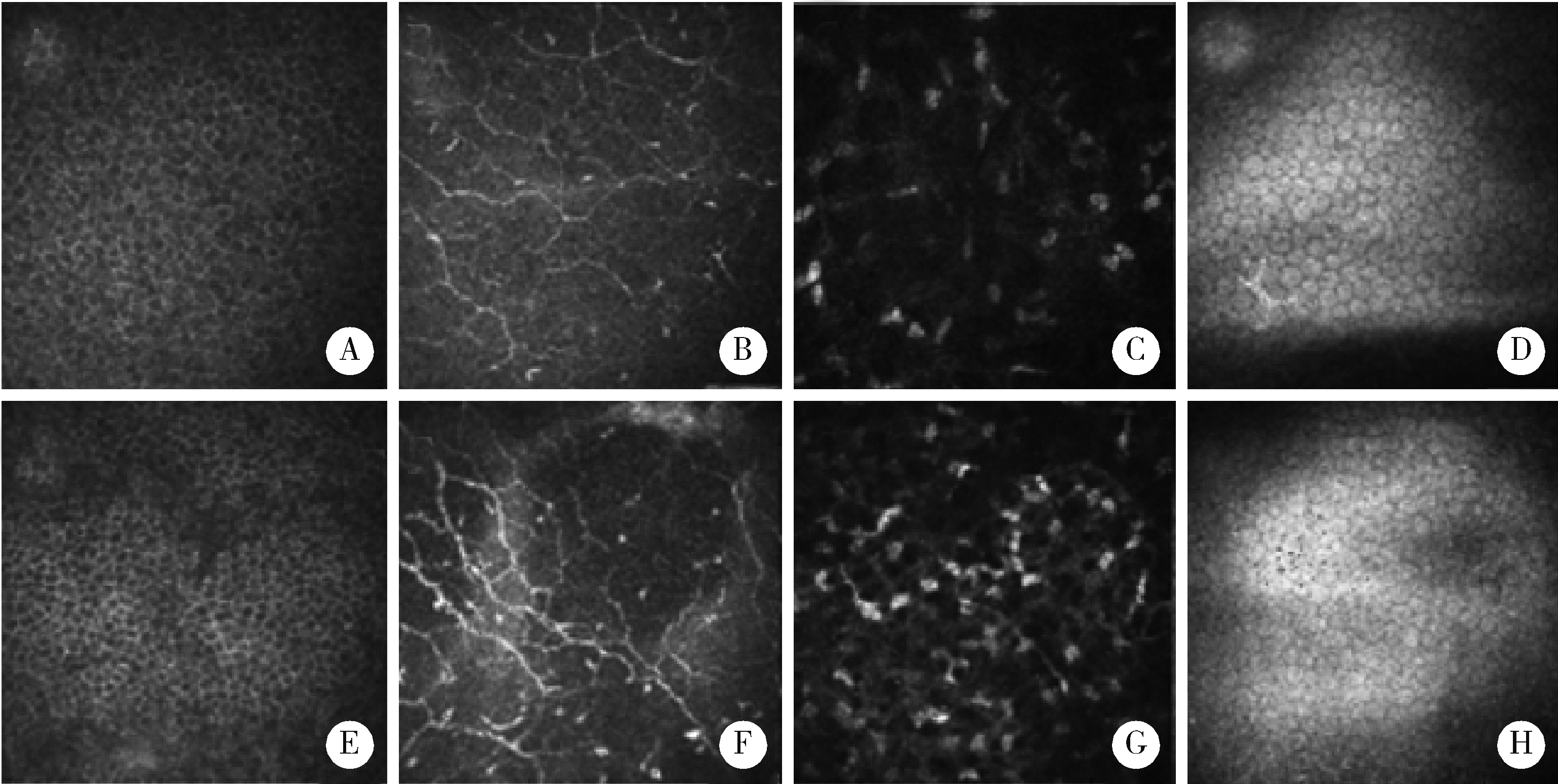
目的: 探讨合并甲状腺功能减退(hypothyroidism, HT)对原发性干燥综合征相关性干眼(primary Sjögren’ s syndrome related dry eye, pSS-DED)患者眼表状态的影响。方法: 采用横断面研究,选择2020年12月—2021年6月在北京大学第三医院眼科干眼门诊就诊的pSS-DED患者36例,其中合并HT的pSS-DED患者12例,并纳入同时期就诊的单纯干眼症(dry eye disease, DED)患者24例作为对照组。所有患者填写眼表疾病指数(ocular surface disease index, OSDI)问卷,并进行泪膜破裂时间(tear film break-up time, BUT)、泪液分泌Schirmer试验、泪河高度、角/结膜荧光素染色、睑板腺分泌能力、睑酯性状评估,以及共聚焦显微镜检查。结果: (1) 较pSS-DED及单纯DED患者,合并HT后pSS-DED患者的平均BUT[(2.7±0.8) s]、Schirmer试验结果[(4.9±4.8) mm]以及泪河高度[(0.13±0.03) mm]更低,差异具有统计学意义(F=12.43,P < 0.01;F=6.96,P < 0.01;F=3.31, P < 0.05)。(2)合并HT后pSS-DED患者的睑板腺分泌能力与睑酯性状评分较DED与pSS-DED患者多集中于高分区,3组患者的睑板腺分泌能力(χ2=10.72,P < 0.05)及睑酯性状评估分数分布(χ2=8.34,P < 0.05)差异具有统计学意义。(3)pSS-DED+HT患者血清总甲状腺素、血清游离甲状腺素水平与其BUT(r=0.60;0.60)、Schirmer试验(r=0.64;0.66),以及泪河高度(r=0.61;0.62)正相关(P < 0.05;P < 0.05),与睑板腺分泌能力无关;未发现促甲状腺激素、抗甲状腺球蛋白抗体、甲状腺过氧化物酶抗体与眼表状态存在明显相关性。(4)相较pSS-DED,合并HT后患者基底下神经丛纤维密度降低(t=2.06,P < 0.05),曲率评分增加(t=2.13,P < 0.05)。结论: 合并HT的pSS-DED患者较pSS-DED以及DED患者的眼表状况更差,主要表现为泪液分泌减少、泪膜稳定性下降、睑板腺分泌功能降低、睑酯性状变差、基底下神经丛纤维密度降低与曲率增加,其机制可能与甲状腺激素分泌减少有关。
中图分类号:
- R593.2
| 1 | Chowdhury F, Tappuni A, Bombardieri M. Biological therapy in primary Sjögren's syndrome: Effect on salivary gland function and inflammation[J/OL]. Front Med, 2021, 8: 707104[2021-07-01]. https://www.frontiersin.org/articles/10.3389/fmed.2021.707104/full. |
| 2 | Bron AJ , de Paiva CS , Chauhan SK , et al. TFOS DEWS Ⅱ pathophysiology report[J]. Ocul Surf, 2017, 15 (3): 438- 510. |
| 3 |
Villarreal-Gonzalez AJ , Rivera-Alvarado IJ , Rodriguez-Gutierrez LA , et al. Analysis of ocular surface damage and visual impact in patients with primary and secondary Sjögren syndrome[J]. Rheumatol Int, 2020, 40 (8): 1249- 1257.
doi: 10.1007/s00296-020-04568-7 |
| 4 |
Xu D , Zhao S , Li Q , et al. Characteristics of Chinese patients with primary Sjögren's syndrome: Preliminary report of a multi-centre registration study[J]. Lupus, 2020, 29 (1): 45- 51.
doi: 10.1177/0961203319889666 |
| 5 |
Wang TJ , Wang IJ , Hu CC , et al. Comorbidities of dry eye disease: A nationwide population-based study[J]. Acta Ophthalmol, 2012, 90 (7): 663- 668.
doi: 10.1111/j.1755-3768.2010.01993.x |
| 6 |
亚洲干眼协会中国分会, 海峡两岸医药卫生交流协会眼科学专业委员会眼表与泪液病学组中国医师协会眼科医师分会眼表与干眼学组. 中国干眼专家共识: 检查和诊断(2020年)[J]. 中华眼科杂志, 2020, 56 (10): 741- 747.
doi: 10.3760/cma.j.cn112142-20200714-00477 |
| 7 |
Shiboski CH , Shiboski SC , Seror R , et al. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for primary Sjögren's syndrome: A consensus and data-driven methodology involving three international patient cohorts[J]. Arthritis Rheumatol, 2017, 69 (1): 35- 45.
doi: 10.1002/art.39859 |
| 8 |
中华医学会内分泌学分会. 成人甲状腺功能减退症诊治指南[J]. 中华内分泌代谢杂志, 2017, 33 (2): 167- 180.
doi: 10.3760/cma.j.issn.1000-6699.2017.02.018 |
| 9 |
Oliveira-Soto L , Efron N . Morphology of corneal nerves using confocal microscopy[J]. Cornea, 2001, 20 (4): 374- 384.
doi: 10.1097/00003226-200105000-00008 |
| 10 | Sun X, Lu L, Li Y, et al. Increased risk of thyroid disease in patients with Sjögren's syndrome: A systematic review and meta-analysis[J/OL]. Peerj, 2019, 7: 6737[2021-07-01]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6430100/. |
| 11 |
Sepulveda JIR , Kvarnstrom M , Eriksson P , et al. Long-term follow-up in primary Sjögren's syndrome reveals differences in clinical presentation between female and male patients[J]. Biol Sex Differ, 2017, 8 (1): 25.
doi: 10.1186/s13293-017-0146-6 |
| 12 |
Jara LJ , Navarro C , Brito-Zerón MDP , et al. Thyroid disease in Sjögren's syndrome[J]. Clin Rheumatol, 2007, 26 (10): 1601- 1606.
doi: 10.1007/s10067-007-0638-6 |
| 13 |
Williams DL , Pierce V , Mellor P , et al. Reduced tear production in three canine endocrinopathies[J]. J Small Anim Pract, 2007, 48 (5): 252- 256.
doi: 10.1111/j.1748-5827.2007.00349.x |
| 14 |
Dias AC , MóDulo CM , Jorge ALG , et al. Influence of thyroid hormone on thyroid hormone receptor β-1 expression and lacrimal gland and ocular surface morphology[J]. Invest Ophth Vis Sci, 2007, 48 (7): 3038- 3042.
doi: 10.1167/iovs.06-1309 |
| 15 |
Kang YS , Lee HS , Li Y , et al. Manifestation of meibomian gland dysfunction in patients with Sjögren's syndrome, non-Sjögren's dry eye, and non-dry eye controls[J]. Int Ophthalmol, 2018, 38 (3): 1161- 1167.
doi: 10.1007/s10792-017-0577-4 |
| 16 |
Wang LX , Deng YP . Androgen and meibomian gland dysfunction: From basic molecular biology to clinical applications[J]. Int J Ophthalmol, 2021, 14 (6): 915- 922.
doi: 10.18240/ijo.2021.06.18 |
| 17 |
Satitpitakul V , Rattanaphong T , Pruksakorn V . Meibomian glands dropout in patients with inactive thyroid related orbitopathy[J]. PLoS One, 2021, 16 (4): e0250617.
doi: 10.1371/journal.pone.0250617 |
| 18 | Altay M , Şahin T , Yildiz Z , et al. Changes in conjunctiva morphology using impression cytology in patients with Hashimoto's thyroiditis without thyroid-associated ophthalmopathy[J]. Turk Patoloji Derg, 2019, 35 (3): 213- 220. |
| 19 |
Wang Q , Shangguan J , Zhang Y , et al. The prevalence of thyroid autoantibodies in autoimmune connective tissue diseases: A systematic review and meta-analysis[J]. Expert Rev Clin Immunol, 2020, 16 (9): 923- 930.
doi: 10.1080/1744666X.2020.1811089 |
| 20 | 解如山. 桥本甲状腺炎患者发生干眼症的相关联性分析[J]. 现代医药卫生, 2015, 31 (22): 3436- 3438. |
| 21 | Altin Ekin M , Karadeniz Ugurlu S , Egrilmez ED , et al. Ocular surface changes in Hashimoto's thyroiditis without thyroid ophthalmopathy[J]. Eye Contact Lens, 2021, 47 (1): 32- 37. |
| 22 | Xu J, Chen P, Yu C, et al. In vivo confocal microscopic evaluation of corneal dendritic cell density and subbasal nerve parameters in dry eye patients: A systematic review and meta-analysis[J/OL]. Front Med, 2021, 8: 578233[2021-07-01]. https://www.frontiersin.org/articles/10.3389/fmed.2021.578233/full. |
| 23 | Li F, Zhang Q, Ying X, et al. Corneal nerve structure in patients with primary Sjögren's syndrome in China[J/OL]. BMC Ophthalmol, 2021, 21(1): 211[2021-07-01]. https://bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-021-01967-7. |
| 24 | Gabbriellini G , Baldini C , Varanini V , et al. In vivo confocal scanning laser microscopy in patients with primary Sjögren's syndrome: A monocentric experience[J]. Mod Rheumatol, 2015, 25 (4): 585- 589. |
| 25 | Levine H, Hwang J, Dermer H, et al. Relationships between activated dendritic cells and dry eye symptoms and signs[J/OL]. Ocul Surf, 2021, 21: 186-192[2021-07-01]. https://www.sciencedirect.com/science/article/pii/S1542012421000513?via%3Dihub. |
| 26 | Cardigos J , Barcelos F , Carvalho H , et al. Tear meniscus and corneal sub-basal nerve plexus assessment in primary Sjögren syndrome and sicca syndrome patients[J]. Cornea, 2019, 38 (2): 221- 228. |
| [1] | 孟彦宏,陈怡帆,周培茹. CENP-B抗体阳性的原发性干燥综合征患者的临床和免疫学特征[J]. 北京大学学报(医学版), 2023, 55(6): 1088-1096. |
| [2] | 韩艺钧,李常虹,陈秀英,赵金霞. 抗SSB抗体阳性和阴性的原发性干燥综合征患者临床及免疫学特征的比较[J]. 北京大学学报(医学版), 2023, 55(6): 1000-1006. |
| [3] | 王一帆,范稹,成姚斌,金月波,霍阳,何菁. 原发性干燥综合征患者睡眠障碍的相关影响因素[J]. 北京大学学报(医学版), 2020, 52(6): 1063-1068. |
| [4] | 蔡佳,张曼. 孕期不同甲状腺功能状态血清高密度脂蛋白胆固醇和载脂蛋白A-Ⅰ的变化趋势[J]. 北京大学学报(医学版), 2015, 47(6): 910-913. |
| [5] | 徐佳露, 杨茹莱, 毛华庆, 赵正言. 浙江省不同地域新生儿先天性甲状腺功能低下症筛查分析[J]. 北京大学学报(医学版), 2012, 44(5): 816-818. |
| [6] | 姚海红, 李玉慧, 张学武, 栗占国. 皮肌炎合并甲状腺功能异常的临床及免疫学特征分析[J]. 北京大学学报(医学版), 2011, 43(2): 209-212. |
| [7] | 伍细言, 王华, 黄定梅, 雷花香, 胡蓉, 马力, 邹珊静, 禹虹. 湖南省106 224例新生儿先天性甲状腺功能减低症筛查[J]. 北京大学学报(医学版), 2005, 37(1): 42-44. |
|
||