北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (2): 362-365. doi: 10.19723/j.issn.1671-167X.2023.02.024
全膝关节置换术后假体周围痛风发作误诊1例
- 北京大学第一医院骨科, 北京 100034
Periprosthetic gout flare after total knee arthroplasty: A misdiagnostic case report
Yi-lin YE,Heng LIU,Li-ping PAN*( ),Wei-bing CHAI
),Wei-bing CHAI
- Department of Orthopedics, Peking University First Hospital, Beijing 100034, China
摘要:
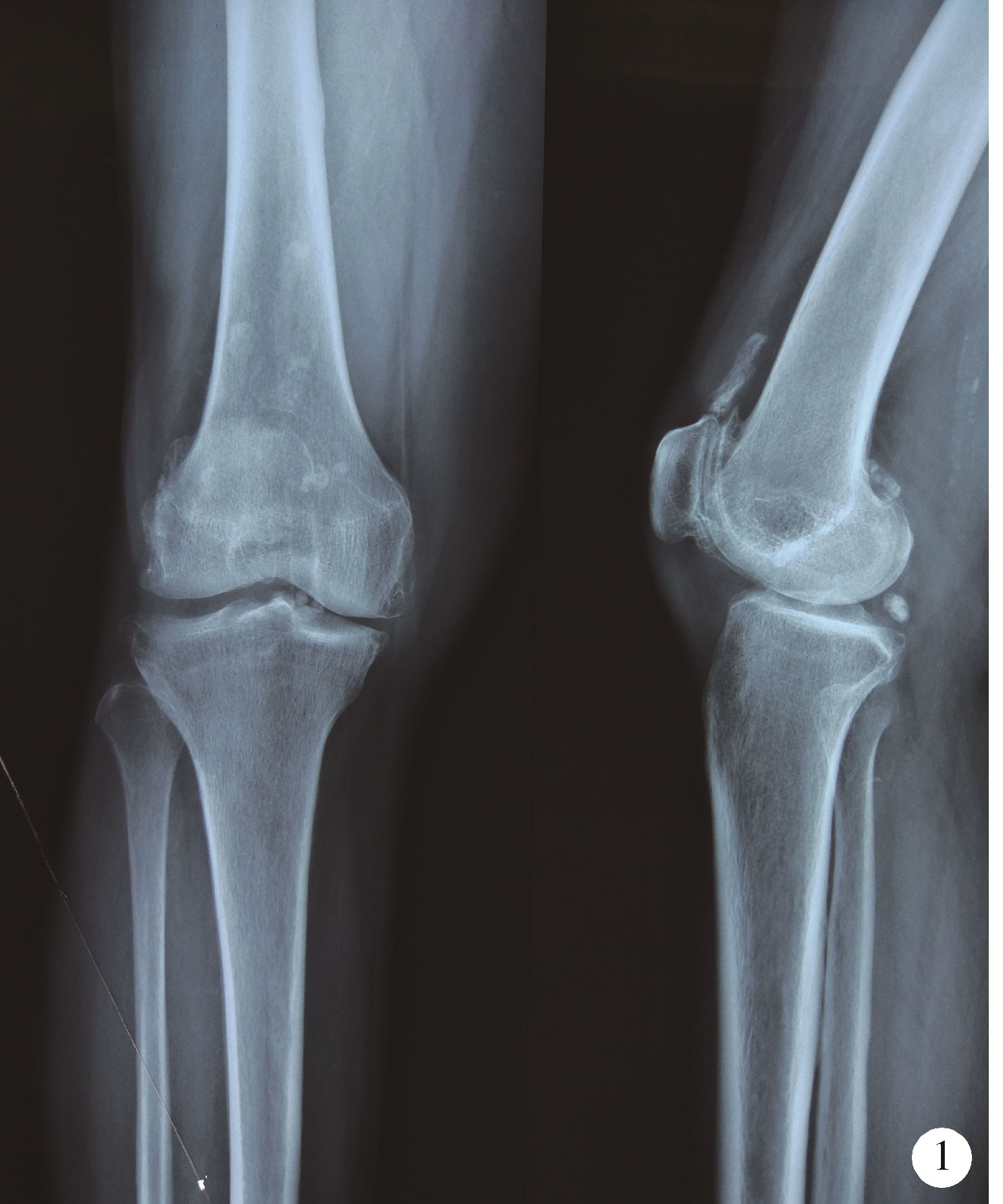
全膝关节置换术后假体周围痛风发作临床上极为少见。由于痛风发作时的临床表现及实验室检查与假体周围急性感染极为相似, 故容易导致误诊。对于假体周围急性感染的患者, 为了及时控制感染并同时保留假体, 常常需要尽早进行关节清创灌洗术并长时间使用抗生素, 而术后关节制动也会导致膝关节功能受限。因此, 术前除外假体周围痛风发作等无菌性关节炎极为重要。本文报道1例长期患有糖尿病及口服激素所致全身免疫缺陷的患者因右膝骨性关节炎进行膝关节置换术, 术后8周时突发发热、关节肿痛及关节功能受限, 同时血白细胞、红细胞沉降率、C反应蛋白显著升高。根据现有的肌肉骨骼感染协会假体周围感染的诊断标准该患者误诊为假体周围急性感染, 并进行了保留假体的关节清理灌洗术。术后患者症状及实验室炎性指标仅有短期好转, 同时病原学结果显示为阴性。当关节清理术后11 d患者全身和局部症状再次出现时, 对该患者进行关节穿刺, 偏光显微镜下关节液晶体检测证实为急性痛风发作。使用抗痛风药物治疗后症状消失, 炎症指标恢复正常, 2年随访无复发。尽管假体周围通风发作十分罕见, 但其仍应作为全膝关节置换术后关节肿痛的一个鉴别诊断, 目前现有的假体周围感染的诊断标准中没有设立除外诊断标准, 提示晶体性关节炎的可能性未在全膝关节置换术后关节肿痛发生时获得重视, 极易带来误诊。因此, 术前常规进行关节液晶体检测非常必要。
中图分类号:
- R697.4
| 1 |
Holt G , Vass C , Kumar CS . Acute crystal arthritis mimicking infection after total knee arthroplasty[J]. BMJ, 2005, 331 (7528): 1322- 1323.
doi: 10.1136/bmj.331.7528.1322 |
| 2 | Salin JW , Lombardi AV Jr , Berend KR , et al. Acute gouty arthropathy after total knee arthroplasty[J]. Am J Orthop, 2008, 37 (8): 420- 422. |
| 3 |
Zadaka A , Gioe T , Gertner E . Acute crystal-induced arthritis following arthroplasty[J]. J Knee Surg, 2010, 23 (1): 17- 20.
doi: 10.1055/s-0030-1262903 |
| 4 | Archibeck MJ , Rosenberg AG , Sheinkop MB , et al. Gout-induced arthropathy after total knee arthroplasty: A report of two cases[J]. Clin Orthop Relat Res, 2001, (392): 377- 382. |
| 5 |
Crawford L , Kumar A , Shepard GJ . Gouty synovitis after total knee arthroplasty: A case report[J]. J Orthop Surg (Hong Kong), 2007, 15 (3): 384- 385.
doi: 10.1177/230949900701500330 |
| 6 |
Parvizi J , Gehrke T . International Consensus Group on Periprosthetic Joint Infection. Definition of periprosthetic joint[J]. J Arthroplasty, 2014, 29 (7): 1331.
doi: 10.1016/j.arth.2014.03.009 |
| 7 | Fokter SK , Repse-Fokter A . Acute gouty arthritis in a patient after total knee arthroplasty[J]. Wien Klin Wochenschr, 2010, 122 (11/12): 366- 367. |
| 8 | Chen F , Glezos C , Blum Y , et al. Nonsurgical treatment of aseptic periprosthetic gout flare of the knee: A report of 2 cases[J]. JBJS Case Connect, 2016, 6 (4): 1- 5. |
| 9 |
Buck M , Delaney M . Diagnosis and management of gout in total knee arthroplasty[J]. Orthop Nurs, 2014, 33 (1): 37- 40.
doi: 10.1097/NOR.0000000000000021 |
| 10 |
Deirmengian C , Kardos K , Kilmartin P , et al. The alpha-defensin test for periprosthetic joint infection outperforms the leukocyte esterase test strip[J]. Clin Orthop Relat Res, 2015, 473 (1): 198- 203.
doi: 10.1007/s11999-014-3722-7 |
| 11 | Lenski M , Scherer MA . Analysis of synovial inflammatory markers to differ infectious from gouty arthritis[J]. Clin Biochem, 2014, 47 (1/2): 49- 55. |
| 12 |
Khalfaoui MY , Yassa R . Crystal arthropathy following knee arthroplasty: A review of the literature[J]. Int J Orthop, 2015, 2 (5): 411- 417.
doi: 10.17554/j.issn.2311-5106.2015.02.113 |
| [1] | 董泓,王丽敏,王志强,刘彦卿,张晓刚,张明明,刘娟,李振彬. 急性痛风发作的昼夜差异: 一项男性痛风患者的临床研究[J]. 北京大学学报(医学版), 2023, 55(5): 915-922. |
| [2] | 王昱,张慧敏,邓雪蓉,刘伟伟,陈璐,赵宁,张晓慧,宋志博,耿研,季兰岚,王玉,张卓莉. 尿枸橼酸定量检测在原发性痛风患者肾结石诊断中的应用价值[J]. 北京大学学报(医学版), 2022, 54(6): 1134-1140. |
| [3] | 谢晓炜,李芬,凌光辉,谢希,许素清,陈谊月. 痛风患者健康教育知识知晓度测量问卷的研制及临床应用[J]. 北京大学学报(医学版), 2022, 54(4): 699-704. |
| [4] | 彭喆,丁亚敏,裴林,姚海红,张学武,唐素玫. 痛风患者发生关节及肌腱内晶体沉积的临床特点[J]. 北京大学学报(医学版), 2021, 53(6): 1067-1071. |
| [5] | 张学武. 痛风关节炎治疗中几个备受关注的问题[J]. 北京大学学报(医学版), 2021, 53(6): 1017-1019. |
| [6] | 王贵红,左婷,李然,左正才. 瑞巴派特在大鼠痛风性关节炎急性发作中的作用[J]. 北京大学学报(医学版), 2021, 53(4): 716-720. |
| [7] | 谢一帆,王昱,邓雪蓉,耿研,季兰岚,张卓莉. 影响双能CT尿酸盐结晶检出率的因素[J]. 北京大学学报(医学版), 2021, 53(2): 261-265. |
| [8] | 王昱,邓雪蓉,季兰岚,张晓慧,耿研,张卓莉. 超声检测痛风患者肌腱受累的危险因素和诊断价值[J]. 北京大学学报(医学版), 2021, 53(1): 143-149. |
| [9] | 季兰岚,郝燕捷,张卓莉. 原发性骨髓纤维化引起的继发性痛风1例[J]. 北京大学学报(医学版), 2018, 50(6): 1117-1119. |
| [10] | 张倩茹,王昱,张卓莉. 2015 ACR/EULAR痛风分类标准与既往标准诊断价值的比较研究[J]. 北京大学学报(医学版), 2017, 49(6): 979-984. |
| [11] | 赵卫, 高辉, 朱佳鑫, 张学武, 栗占国. 血清Dickkopf-1与原发性痛风性关节炎骨破坏的相关性[J]. 北京大学学报(医学版), 2012, 44(2): 254-258. |
| [12] | 武丽君, 宋小芸, 库尔班江, 石亚妹, 黄慈波, 黄嘉, 刘爱华, 米克拉依, 滕玉芬, 古丽娜, 孟新艳, 单新洁, 木亚赛, 苑爱萍, 张莉. 新疆吐鲁番地区维吾尔族人群高尿酸血症和痛风的流行病学调查[J]. 北京大学学报(医学版), 2012, 44(2): 250-253. |
| [13] | 刘湘源, 郑晓娟. 尿酸持续达标是难治性痛风治疗的关键[J]. 北京大学学报(医学版), 2012, 44(2): 168-170. |
| [14] | 张学武. 痛风的规范化诊治迫在眉睫[J]. 北京大学学报(医学版), 2012, 44(2): 165-167. |
|
||