北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (3): 430-435. doi: 10.19723/j.issn.1671-167X.2025.03.004
基于社区人群队列的甘油三酯-葡萄糖指数与心血管病发病和死亡的关联
陆梦溪1, 刘秋萍1, 周恬静1, 刘晓非1, 孙烨祥2, 沈鹏2, 林鸿波2, 唐迅1,3,*( ), 高培1,3,4,*(
), 高培1,3,4,*( )
)
- 1. 北京大学公共卫生学院流行病与卫生统计学系, 北京 100191
2. 宁波市鄞州区疾病预防控制中心, 浙江宁波 315101
3. 重大疾病流行病学教育部重点实验室(北京大学), 北京 100191
4. 北京大学临床研究所真实世界证据评价中心, 北京 100191
Association of triglyceride-glucose index and cardiovascular disease in a community-based Chinese cohort
Mengxi LU1, Qiuping LIU1, Tianjing ZHOU1, Xiaofei LIU1, Yexiang SUN2, Peng SHEN2, Hongbo LIN2, Xun TANG1,3,*( ), Pei GAO1,3,4,*(
), Pei GAO1,3,4,*( )
)
- 1. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
2. Yinzhou District Center for Disease Control and Prevention, Ningbo 315101, Zhejiang, China
3. Key Laboratory of Epidemiology of Major Disease (Peking University), Ministry of Education, Beijing 100191, China
4. Center for Real-World Evidence Evaluation, Peking University Clinical Research Institute, Beijing 100191, China
摘要:
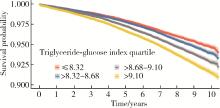
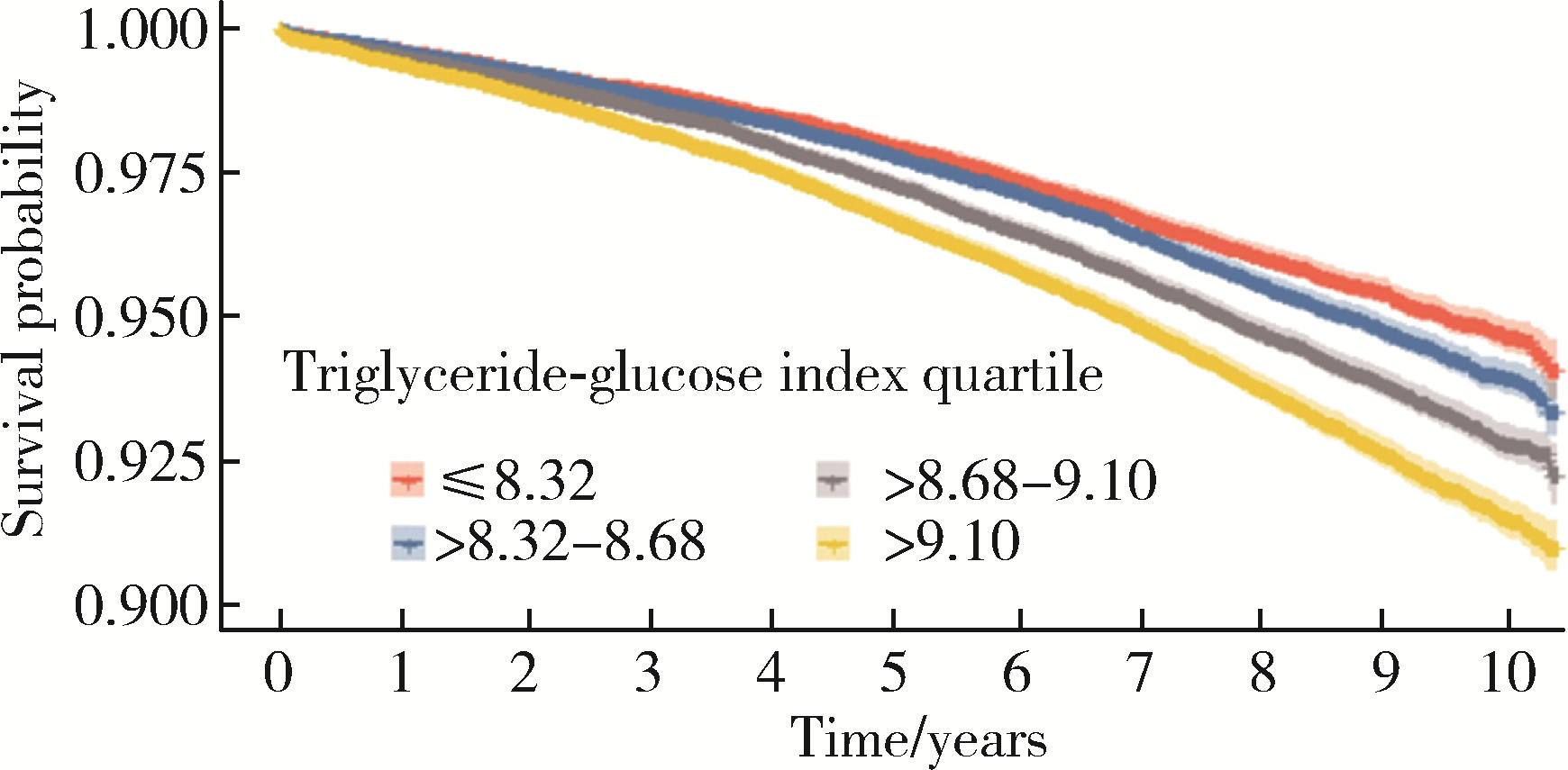
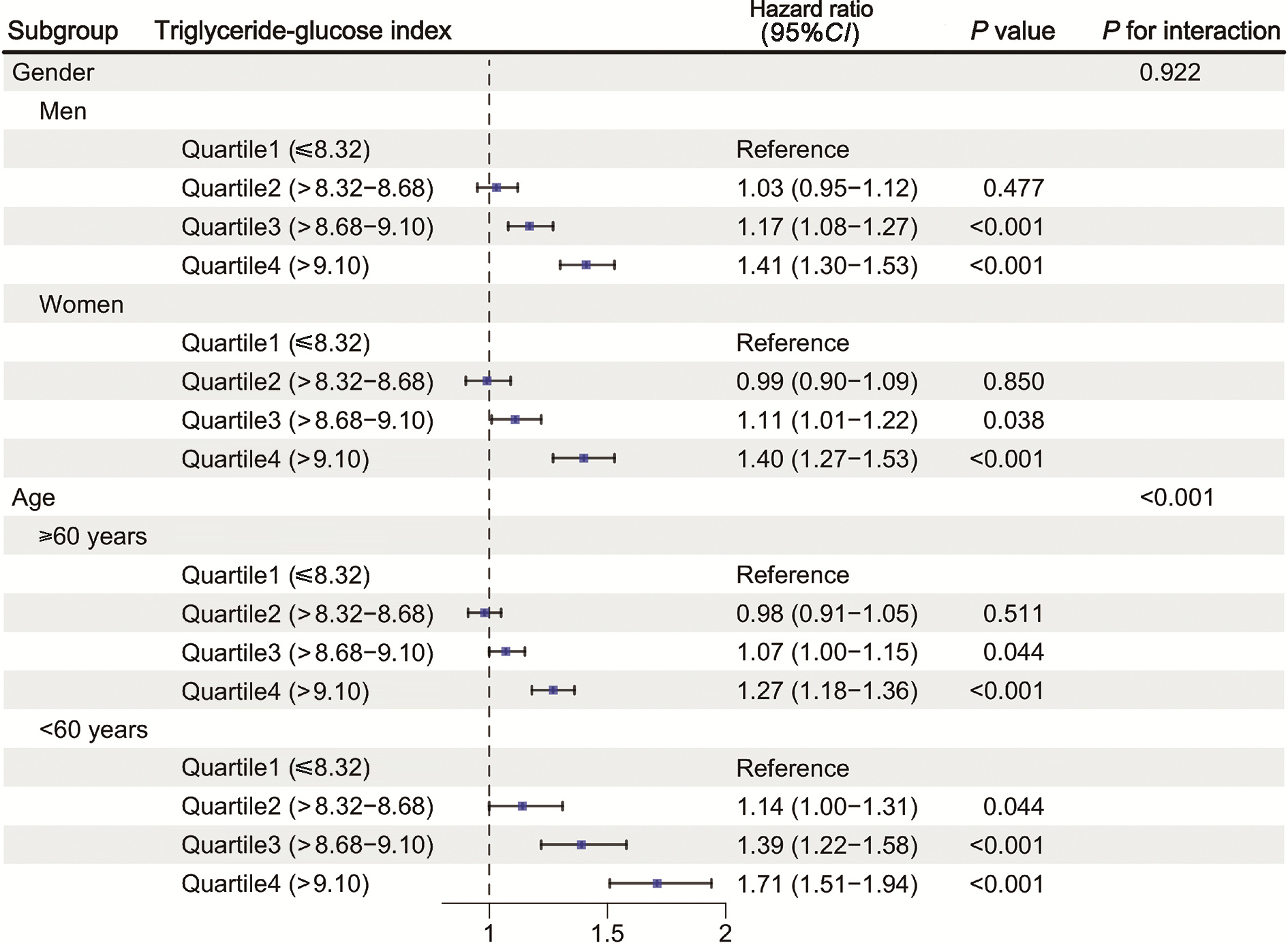
目的: 在大样本社区人群队列中探索甘油三酯-葡萄糖(triglyceride-glucose, TyG)指数与心血管病发病和死亡的关联。方法: 研究对象为2010年1月1日至2020年5月31日纳入中国鄞州电子健康档案研究(CHinese Electronic health Records Research in Yinzhou, CHERRY)队列中40~79岁基线无心血管病史的人群。根据个体的基线甘油三酯和血糖水平计算TyG指数,采用Cox比例风险模型分析TyG指数与心血管病发病和死亡的关联,调整年龄、性别、教育水平、居住地、吸烟状态、体重指数、收缩压及总胆固醇等影响因素后计算风险比(hazard ratio, HR)及其95%置信区间(confidence interval, CI)。采用限制性立方样条回归方法进一步分析TyG指数与心血管病发病和死亡的非线性关联,并按性别、年龄分层探索其关联在不同亚组的差异。结果: 共纳入226 406名研究对象,人群的基线平均年龄为(55.0±9.7)岁,46.8%为男性,TyG指数的中位数为8.68。在中位随访7.99年期间,9 815人(4.34%)出现心血管病发病和死亡。调整年龄、性别、教育水平、居住地、吸烟状态、体重指数、收缩压及总胆固醇等影响因素后,心血管病发病和死亡的风险呈现随TyG指数增加而增大的趋势(P < 0.001),TyG指数处于上四分位数(TyG>9.10)组与下四分位数组(TyG≤8.32)相比,心血管病发病和死亡的风险增加42%(HR=1.42,95%CI:1.34~1.51)。TyG指数对于60岁以下低年龄组人群的心血管病发病和死亡风险增加的效应值相比60岁及以上人群更明显(HR:1.71 vs. 1.27,P < 0.05)。限制性立方样条回归的结果进一步显示,在总人群中TyG指数与心血管病发病和死亡的关联呈现“反L型”关系(非线性趋势P < 0.001),TyG指数超过8.67阈值时心血管病发病和死亡的风险随该指数的增加而升高;但这种非线性关联的风险阈值存在性别差异,女性(8.51)低于男性(8.67)。结论: TyG指数与心血管病发病和死亡存在明显阈值效应的非线性关系,当TyG指数超过一定阈值时,心血管病发病和死亡发生的风险增加,且女性的阈值低于男性,提示后续利用TyG指数开展综合风险预测与危险因素干预时,需要按性别分层管理,特别是在60岁以下人群中开展早期干预具有重要的公共卫生学意义。
中图分类号:
- R54
| 1 |
doi: 10.1161/CIR.0000000000001191 |
| 2 |
doi: 10.1016/j.jacc.2019.03.009 |
| 3 |
doi: 10.1002/dmrr.3502 |
| 4 |
doi: 10.1186/s12933-021-01268-9 |
| 5 |
doi: 10.1186/s12933-024-02571-x |
| 6 |
doi: 10.1186/s12933-022-01511-x |
| 7 |
doi: 10.1186/s12933-024-02244-9 |
| 8 |
doi: 10.1136/bmjopen-2017-019698 |
| 9 |
doi: 10.1186/s12916-020-01824-2 |
| 10 |
doi: 10.1016/S2214-109X(19)30318-3 |
| 11 |
|
| 12 |
doi: 10.1186/s12933-022-01546-0 |
| 13 |
doi: 10.1093/eurjpc/zwae025 |
| 14 |
doi: 10.1038/s41598-019-43776-5 |
| 15 |
doi: 10.1186/s12933-023-02115-9 |
| 16 |
doi: 10.1093/eurheartj/ehab484 |
| 17 |
|
| 18 |
doi: 10.1016/S2214-109X(24)00210-9 |
| 19 |
doi: 10.1186/s12933-024-02334-8 |
| 20 |
doi: 10.1186/s12933-022-01456-1 |
| [1] | 刘伟, 郭稳, 过哲, 李春艳, 李云龙, 刘思奇, 张亮, 宋慧. 痛风患者放射学阴性骨侵蚀的相关危险因素[J]. 北京大学学报(医学版), 2025, 57(4): 735-739. |
| [2] | 杨龙傲, 金旭, 黄文初, 何丽华, 陈娟. 视屏作业人员视疲劳及干眼的流行病学调查[J]. 北京大学学报(医学版), 2025, 57(3): 554-561. |
| [3] | 郭华秋, 王哲, 杨雪, 白洁. 口腔急诊出血患者的临床特征与危险因素[J]. 北京大学学报(医学版), 2025, 57(1): 142-147. |
| [4] | 邓敏婷, 王楠, 夏斌, 赵玉鸣, 朱俊霞. 儿童及青少年挫入恒前牙自行再萌出的相关影响因素[J]. 北京大学学报(医学版), 2025, 57(1): 148-153. |
| [5] | 李钰锴, 王红彦, 罗靓, 李云, 李春. 抗磷脂抗体在白塞病合并血栓中的临床意义[J]. 北京大学学报(医学版), 2024, 56(6): 1036-1040. |
| [6] | 田杨, 韩永正, 李娇, 王明亚, 曲音音, 房景超, 金辉, 李民, 王军, 徐懋, 王圣林, 郭向阳. 颈椎前路手术后硬膜外血肿的发生率和危险因素[J]. 北京大学学报(医学版), 2024, 56(6): 1058-1064. |
| [7] | 王明瑞, 赖金惠, 姬家祥, 唐鑫伟, 胡浩浦, 王起, 许克新, 徐涛, 胡浩. 使用中文版威斯康星结石生活质量问卷预测肾结石患者生活质量降低的危险因素[J]. 北京大学学报(医学版), 2024, 56(6): 1069-1074. |
| [8] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [9] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [10] | 陈延,李况蒙,洪锴,张树栋,程建星,郑仲杰,唐文豪,赵连明,张海涛,姜辉,林浩成. 阴茎海绵体注射试验对阴茎血管功能影响的回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 680-686. |
| [11] | 庞博,郭桐君,陈曦,郭华棋,石嘉章,陈娟,王欣梅,李耀妍,单安琪,余恒意,黄婧,汤乃军,王艳,郭新彪,李国星,吴少伟. 天津与上海35岁以上人群氮氧化物个体暴露水平及其影响因素[J]. 北京大学学报(医学版), 2024, 56(4): 700-707. |
| [12] | 和静,房中则,杨颖,刘静,马文瑶,霍勇,高炜,武阳丰,谢高强. 血浆中脂质代谢分子与颈动脉粥样硬化斑块、传统心血管危险因素及膳食因素的关系[J]. 北京大学学报(医学版), 2024, 56(4): 722-728. |
| [13] | 郭煌达,彭和香,王斯悦,侯天姣,李奕昕,章涵宇,王梦莹,武轶群,秦雪英,唐迅,李劲,陈大方,胡永华,吴涛. 短期大气颗粒物暴露和MTNR1B基因多态性对甘油三酯-葡萄糖指数影响的家系研究[J]. 北京大学学报(医学版), 2024, 56(3): 375-383. |
| [14] | 蔡珊,张依航,陈子玥,刘云飞,党佳佳,师嫡,李佳欣,黄天彧,马军,宋逸. 北京市中小学生身体活动时间现状及影响因素的路径[J]. 北京大学学报(医学版), 2024, 56(3): 403-410. |
| [15] | 张祖洪,陈天娇,马军. 中小学生青春发动时相与心血管代谢危险因素的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 418-423. |
|
||