北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (6): 1145-1152. doi: 10.19723/j.issn.1671-167X.2025.06.019
基于健康行动过程取向模型分析2型糖尿病患者膳食模式及血糖控制的影响因素
闵鹤葳1, 吴一波1, 史宇晖1, 李明子2, 孙昕霙1,*( )
)
- 1. 北京大学公共卫生学院社会医学与健康教育学系, 北京 100191
2. 北京大学护理学院, 北京 100191
Analyzing the influential factors of dietary patterns and blood glucose control in type 2 diabetes patients based on the model of health action process approach model
Hewei MIN1, Yibo WU1, Yuhui SHI1, Mingzi LI2, Xinying SUN1,*( )
)
- 1. Department of Social Medicine and Health Education, Peking University School of Public Health, Beijing 100191, China
2. Peking University School of Nursing, Beijing 100191, China
摘要:
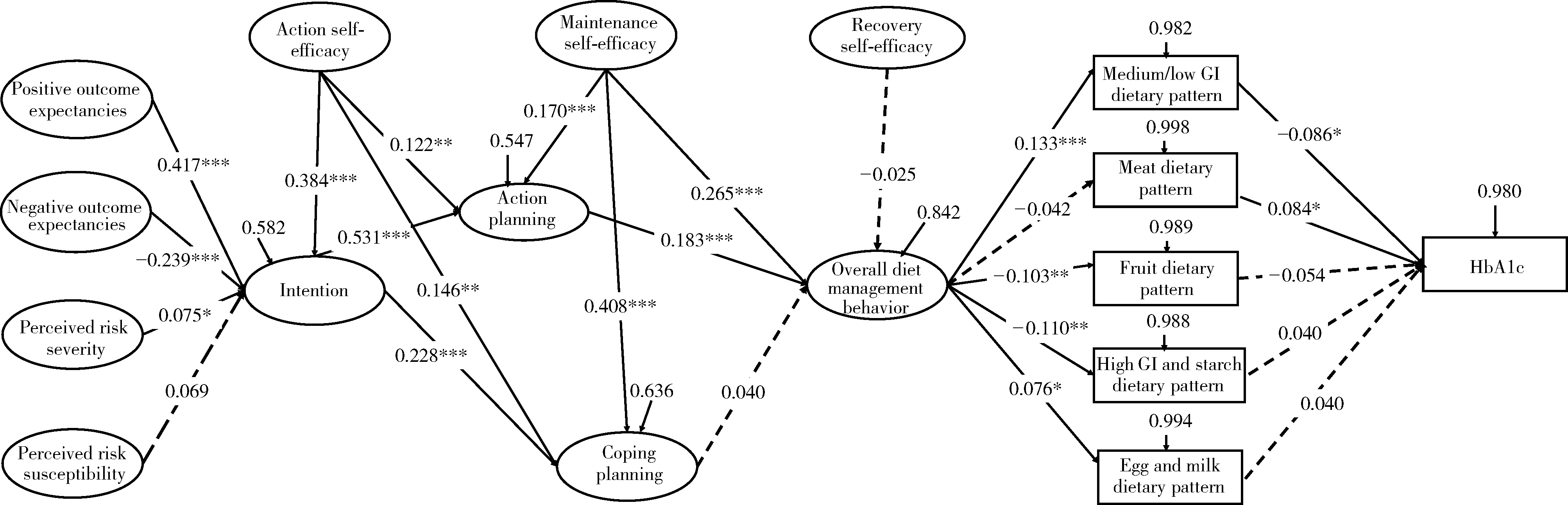
目的: 基于健康行动过程取向(health action process approach, HAPA)模型探究2型糖尿病患者膳食模式和血糖控制的影响因素。方法: 选取山东省东营市东城医院下属的11个社区卫生中心内的2型糖尿病患者作为研究对象,通过静脉抽血检测患者的糖化血红蛋白(glycosylated hemoglobin, HbA1c)水平,采用一般资料调查表、膳食频率调查问卷、2型糖尿病自我管理量表、HAPA量表收集信息。通过因子分析将患者的膳食模式划分为不同类型,通过结构方程模型分析HAPA模型各维度对于患者膳食模式和血糖控制的影响。结果: 共纳入819例2型糖尿病患者,总体HbA1c水平为7.1%±1.1%。研究对象的总体饮食管理得分为5.0 (1.0, 7.0),具体日常饮食被划分为中低血糖生成指数(glycemic index,GI)膳食模式、肉类膳食模式、水果膳食模式、高GI/淀粉类膳食模式、蛋奶类膳食模式。结构方程模型结果显示,积极结果预期(β=0.417,P<0.001)、消极结果预期(β=-0.239,P<0.001)和感知风险严重性(β=0.075,P=0.036)影响饮食管理行为意向;饮食管理行为意向影响行动计划(β=0.531,P<0.001)和应对计划(β=0.228,P<0.001);行动计划影响总体饮食管理行为(β=0.183,P<0.001);总体饮食管理行为影响中低GI膳食模式(β=0.133,P<0.001)、水果膳食模式(β=-0.103,P=0.003)、高GI/淀粉类膳食模式(β=-0.110,P=0.002)和蛋奶类膳食模式(β=0.076,P=0.031);中低GI膳食模式(β=-0.086,P=0.013)、肉类膳食模式(β=0.084,P=0.015)影响HbA1c水平。此外,行动自我效能可以影响行为意向(β=0.384,P<0.001)、行动计划(β=0.122,P=0.006)和应对计划(β=0.146,P=0.001)。维持自我效能可以影响行动计划(β=0.170,P<0.001)、应对计划(β=0.408,P<0.001)和总体饮食管理行为(β=0.265,P<0.001)。结论: 纳入的2型糖尿病患者的膳食模式存在差异,且每周饮食管理的水平欠佳,〖JP+2〗HAPA模型对于2型糖尿病患者的膳食模式和血糖控制水平具有较好的解释作用,因此,今后可基于HAPA模型制定针对性的饮食干预,提高患者的总体饮食管理水平,促进患者养成低GI的健康膳食模式,从而改善血糖水平,提高生活质量。
中图分类号:
- R193.3
| 1 |
|
| 2 |
doi: 10.1016/j.ajcnut.2023.08.022 |
| 3 |
Schwarzer R, Sniehotta FF, Lippke S, et al. On the assessment and analysis of variables in the health action process approach conducting an investigation[EB/OL]. (2013-11-01)[2024-05-20]. https://citeseerx.ist.psu.edu/viewdoc/download;jsessionid=3FFB18BA8EEC17A6CFA2C9065A98F60Fdoi=10.1.1.388.1394&rep=rep1&type=pdf.
|
| 4 |
doi: 10.1093/heapro/daad095 |
| 5 |
|
| 6 |
doi: 10.1080/08870446.2018.1458983 |
| 7 |
doi: 10.2196/13363 |
| 8 |
doi: 10.1111/aphw.12190 |
| 9 |
doi: 10.1016/j.pcd.2019.08.009 |
| 10 |
陈雪莹. 社区2型糖尿病患者饮食教具干预的效果评价研究[D]. 北京: 北京大学, 2021.
|
| 11 |
doi: 10.2337/diacare.23.7.943 |
| 12 |
doi: 10.1016/0749-5978(91)90020-T |
| 13 |
doi: 10.1037/0278-6133.19.5.487 |
| 14 |
温鑫. 基于HAPA理论慢性肾病健康饮食认知信念问卷的编制及应用研究[D]. 长春: 吉林大学, 2020.
|
| 15 |
doi: 10.2196/40420 |
| 16 |
doi: 10.1038/ejcn.2017.41 |
| 17 |
王雨, 李桂丽, 李颖. 糖尿病患者的膳食模式与伴发心脑血管疾病的关系研究[J]. 营养学报, 2021, 43 (2): 144- 149.
|
| 18 |
doi: 10.1016/j.jacc.2016.06.011 |
| 19 |
doi: 10.3390/nu13010116 |
| 20 |
doi: 10.1186/s12937-017-0303-0 |
| 21 |
doi: 10.1017/S1368980020004930 |
| 22 |
doi: 10.1007/s10654-017-0246-y |
| 23 |
doi: 10.3390/nu14030706 |
| 24 |
|
| 25 |
doi: 10.1016/S0140-6736(14)60613-9 |
| 26 |
doi: 10.1093/ajcn/nqz035 |
| 27 |
doi: 10.1111/obr.12172 |
| 28 |
doi: 10.1093/eurheartj/ehad336 |
| 29 |
doi: 10.1037/a0030182 |
| 30 |
doi: 10.19082/6647 |
| 31 |
doi: 10.1016/j.appet.2013.06.097 |
| 32 |
doi: 10.1111/aphw.12050 |
| 33 |
doi: 10.1111/bjhp.12144 |
| 34 |
曹佃省, 谢光荣. 从行为意向到健康行为: 健康行为程式模型(HAPA)概述[J]. 中国临床心理学杂志, 2010, 18 (6): 809- 812.
|
| 35 |
张持晨, 郑晓, 赵慧宁, 等. 基于健康行为过程取向的大学生膳食行为干预[J]. 卫生研究, 2017, 46 (5): 755- 760.
|
| 36 |
张向京, 岳建华, 林锐. 健康行为HAPA模型为指导提高老年高血压患者自我效能、心理健康和服药依从性的影响[J]. 中国健康心理学杂志, 2021, 29 (8): 1199- 1204.
|
| 37 |
doi: 10.1186/s13098-021-00773-x |
| 38 |
|
| 39 |
赵静, 赵秋利, 王丽敏, 等. 2型糖尿病患者饮食行为改变特征的研究[J]. 中华护理杂志, 2018, 53 (2): 139- 143.
|
| 40 |
郭怡, 孙信, 黎泽明, 等. 基于健康行动过程取向理论模型分析2型糖尿病患者锻炼行为现状[J]. 中华疾病控制杂志, 2022, 26 (1): 56-60, 98.
|
| 41 |
朱金凤, 蔡卫新, 陶子荣, 等. 中青年出血性脑卒中患者康复运动依从性现状及其影响因素分析[J]. 中华护理杂志, 2023, 58 (5): 580- 586.
|
| 42 |
doi: 10.4103/jehp.jehp_175_20 |
| [1] | 鲍雷,蔡夏夏,张明远,任磊磊. 维生素D3对2型糖尿病小鼠轻度认知障碍的改善作用及机制研究[J]. 北京大学学报(医学版), 2023, 55(4): 587-592. |
| [2] | 于欢,杨若彤,王斯悦,吴俊慧,王梦莹,秦雪英,吴涛,陈大方,武轶群,胡永华. 2型糖尿病患者使用二甲双胍与缺血性脑卒中发病风险的队列研究[J]. 北京大学学报(医学版), 2023, 55(3): 456-464. |
| [3] | 张晓悦,林雨欣,蒋莹,张蓝超,董芒艳,池海谊,董浩宇,马利军,李智婧,常春. 自我效能在2型糖尿病患者自我管理能力和自我管理行为间的中介效应[J]. 北京大学学报(医学版), 2023, 55(3): 450-455. |
| [4] | 陈平,黎泽明,郭怡,孙昕霙,Edwin B.FISHER. 基于大五人格理论应用潜在剖面分析探究2型糖尿病患者的用药依从性[J]. 北京大学学报(医学版), 2021, 53(3): 530-535. |
| [5] | 黎泽明,高敏,陈雪莹,孙昕霙. 2型糖尿病患者大五人格特征与自我管理态度的相关性[J]. 北京大学学报(医学版), 2020, 52(3): 506-513. |
| [6] | 谢江,李菲. 睡眠重叠综合征与糖尿病发病率的横断面调查研究[J]. 北京大学学报(医学版), 2019, 51(2): 252-255. |
|
||