北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (6): 1136-1144. doi: 10.19723/j.issn.1671-167X.2025.06.018
中国老年人社会经济地位与视力障碍的相关性
- 北京大学公共卫生学院卫生政策与管理学系, 北京 100191
Association between socioeconomic status and vision impairment among Chinese elderly
- Department of Health Policy and Management, Peking University School of Public Health, Beijing 100191, China
摘要:
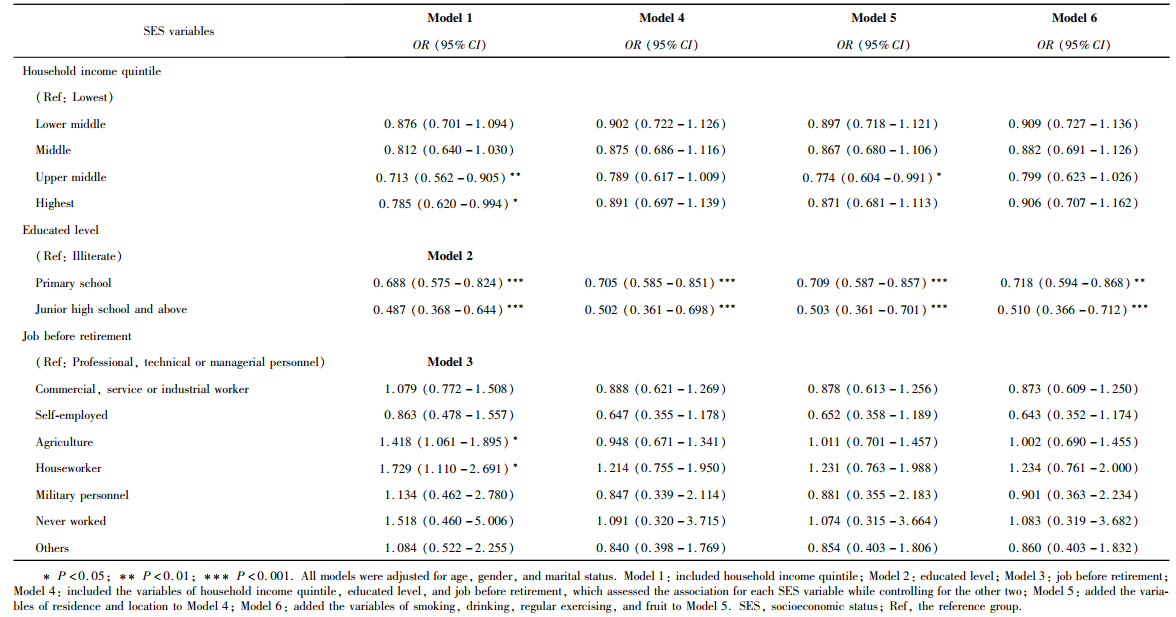
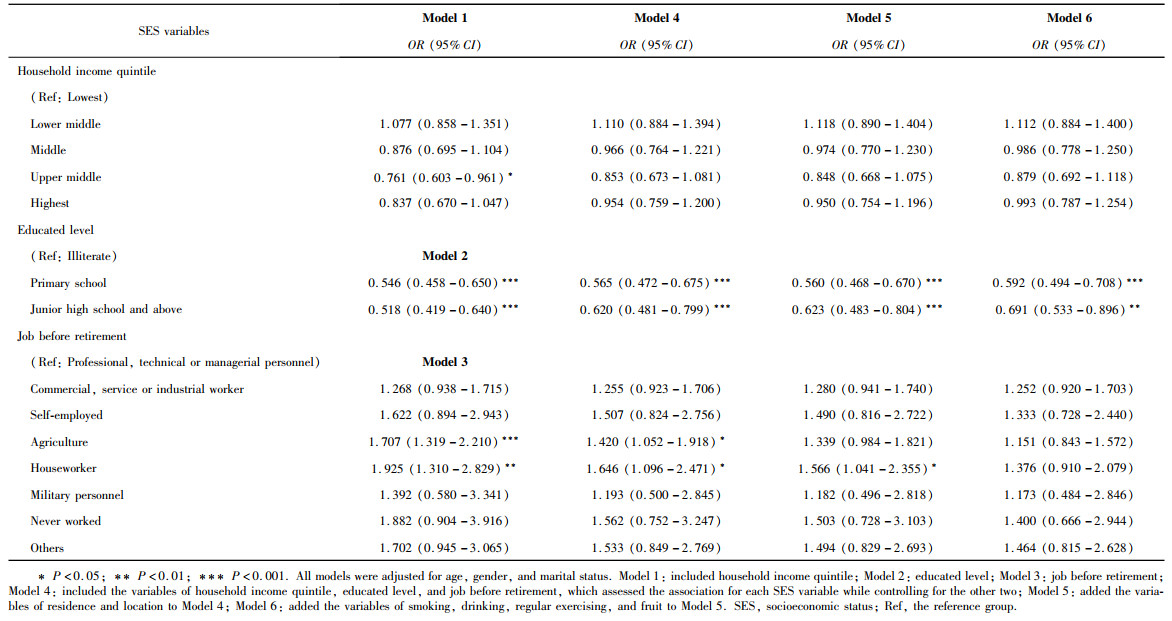
目的: 分析中国65岁及以上老年人的社会经济地位与视力障碍的相关性, 并比较2008-2018年的变化情况。方法: 使用2008年和2018年"中国老年人健康长寿影响因素调查"的横断面数据, 分别纳入12970名和9702名受访者。构建Logistic回归模型, 采用逐步进入法依次加入控制变量, 分析2008年和2018年中国老年人家庭收入、受教育程度、退休前职业与视力障碍之间的关联。结果: 2008年中国65岁及以上老年人视力障碍患病率为16.92%(95%CI: 15.91%~17.98%), 2018年该患病率上升至18.45%(95%CI: 17.41%~19.53%)。与低收入群体相比, 2008年高收入和中高收入群体患视力障碍的风险较低, 2018年仅中高收入群体患视力障碍的风险较低(OR=0.761, 95%CI: 0.603~0.961), 且差距缩小。与文盲相比, 2008年小学、初中及以上学历群体患视力障碍的风险较低, 2018年小学组与文盲组的差距增大, 初中及以上组与文盲组、小学组的差距缩小, 控制其他因素后, 初中及以上组的患病风险高于小学组(OR=0.691, 95%CI: 0.533~0.896;OR=0.592, 95%CI: 0.494~0.708)。与退休前从事专业技术或管理类职业群体相比, 2008年从事农业、家务劳动群体患视力障碍的风险较高, 2018年这一现象依旧存在(OR=1.707, 95%CI: 1.319~2.210;OR=1.925, 95%CI: 1.310~2.829), 且两个群体间的差距有所增大。结论: 中国老年人视力障碍的患病率在2008-2018年间有所上升, 家庭收入、受教育程度、退休前职业与视力障碍之间存在关联。2008-2018年, 不同家庭收入群体患视力障碍的风险差距缩小; 不同受教育程度群体的患病风险差距整体缩小, 但小学学历群体与文盲群体的差距增大; 退休前各职业类型群体的患病风险差距增大。
中图分类号:
- R197.1
| 1 |
doi: 10.1016/S2214-109X(21)00031-0 |
| 2 |
doi: 10.1080/13607863.2022.2077303 |
| 3 |
doi: 10.1016/S2214-109X(20)30549-0 |
| 4 |
doi: 10.1097/OPX.0000000000001773 |
| 5 |
doi: 10.1136/jech-2016-207331 |
| 6 |
World Health Organization. World report on vision. Geneva: World Health Organization [EB/OL]. (2019-12-08) [2025-01-26]. https://www.who.int/publications/i/item/9789241516570.
|
| 7 |
doi: 10.1016/S0140-6736(18)32335-3 |
| 8 |
doi: 10.1186/s12886-018-0710-9 |
| 9 |
国家卫生健康委. 国家卫生健康委关于印发"十四五"全国眼健康规划(2021—2025年)的通知[EB/OL]. (2022-01-04) [2025-01-26]. https://www.gov.cn/zhengce/zhengceku/2022-01/17/content_5668951.htm.
|
| 10 |
doi: 10.7189/jogh.12.11006 |
| 11 |
doi: 10.4103/0301-4738.100529 |
| 12 |
|
| 13 |
|
| 14 |
|
| 15 |
doi: 10.1016/j.ophtha.2015.03.022 |
| 16 |
doi: 10.1371/journal.pone.0215329 |
| 17 |
doi: 10.1016/S0140-6736(17)30548-2 |
| 18 |
北京大学健康老龄与发展研究中心. 中国老年健康影响因素跟踪调查(CLHLS)-追踪数据(1998-2018) [EB/OL]. (2020-04-03) [2025-02-06]. https://doi.org/10.18170/DVN/WBO7LK.
|
| 19 |
doi: 10.3917/popu.p2001.13n1.0116 |
| 20 |
doi: 10.1111/jgs.17311 |
| 21 |
doi: 10.1016/j.survophthal.2018.08.003 |
| 22 |
doi: 10.2105/AJPH.92.7.1151 |
| 23 |
doi: 10.14283/jpad.2024.127 |
| 24 |
doi: 10.1186/s12877-018-0785-4 |
| 25 |
doi: 10.1093/ageing/afx038 |
| 26 |
doi: 10.1016/S2468-2667(20)30254-1 |
| 27 |
|
| 28 |
doi: 10.1016/j.ophtha.2022.07.010 |
| 29 |
doi: 10.1136/bjophthalmol-2013-303249 |
| 30 |
doi: 10.1001/jamaophthalmol.2022.5237 |
| 31 |
赵月, 王爱平. 老年人视力障碍影响因素的研究进展[J]. 中国实用护理杂志, 2021, 37 (13): 1032- 1036.
|
| 32 |
熊晓菁. 重庆市农村地区土家族老年人群视力障碍患病率及原因分析[D]. 重庆: 重庆医科大学, 2018.
|
| 33 |
|
| 34 |
张文宏, 陈晓冰. 教育对个体健康水平的影响[J]. 山东社会科学, 2020 (7): 84- 93.
|
| 35 |
吴玮. 教育对健康的影响分析[D]. 杭州: 浙江大学, 2009.
|
| 36 |
资德平. 教育对健康的影响分析[D]. 长沙: 湖南大学, 2016.
|
| 37 |
成前, 王鸿儒, 倪志良. 教育水平、个体健康与公共财政支持[J]. 江西财经大学学报, 2016 (5): 24- 32.
|
| 38 |
靳永爱, 胡文波, 冯阳. 数字时代的互联网使用与中老年人生活——中国老年群体数字鸿沟与数字融入调查主要数据结果分析[J]. 人口研究, 2024, 48 (1): 40- 55.
|
| 39 |
中国互联网络信息中心. 第43次《中国互联网络发展状况统计报告》 [EB/OL]. (2019-02-28) [2025-02-06]. https://www.cnnic.cn/n4/2022/0401/c88-838.html.
|
| 40 |
中国乡村发展基金会. 光明工程白内障复明项目[EB/OL]. (2022) [2025-02-06]. https://www.cfpa.org.cn/project/GNProjectDetail.aspx?id=134.
|
| 41 |
马震, 严丽萍, 魏南方. 不同职业特征人群健康素养现状调查[J]. 中国预防医学杂志, 2012, 13 (5): 380- 383.
|
| [1] | 刘园梅, 傅义程, 郝靖欣, 张福春, 刘慧琳. 老年髋部骨折患者住院期间发生术后心力衰竭的列线图预测模型的构建及验证[J]. 北京大学学报(医学版), 2024, 56(5): 874-883. |
| [2] | 张浩宇,石逸雯,潘薇,刘爱萍,孙昕霙,李曼,张旭熙. 基于不同失能水平的老年人照料需求的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 431-440. |
| [3] | 靖婷,江华,李婷,申倩倩,叶兰,曾银丹,梁文欣,冯罡,司徒文佑,张玉梅. 中国西部5城市中老年人血清25羟基维生素D与握力的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 448-455. |
| [4] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [5] | 汤华萌,袁典琪,王明星,杨晗冰,郭超. 数字融入和健康生活方式对社会经济状况与老年人抑郁关系的序列中介作用[J]. 北京大学学报(医学版), 2024, 56(2): 230-238. |
| [6] | 刘慧丽,吕彦函,王晓晓,李民. 老年患者腹腔镜泌尿系肿瘤根治术后慢性疼痛的影响因素[J]. 北京大学学报(医学版), 2023, 55(5): 851-856. |
| [7] | 祝春素,连至炜,崔一民. 中国中老年人抑郁和慢性病的关联[J]. 北京大学学报(医学版), 2023, 55(4): 606-611. |
| [8] | 刘光奇,庞元捷,吴疆,吕敏,于孟轲,李雨橦,黄旸木. 2013—2019年流感季北京市住院老年人流感疫苗接种趋势分析[J]. 北京大学学报(医学版), 2022, 54(3): 505-510. |
| [9] | 刘杰,郭超. 正/负性情绪对中国老年人死亡风险影响的前瞻性队列研究[J]. 北京大学学报(医学版), 2022, 54(2): 255-260. |
| [10] | 李佳,徐钰,王优雅,高占成. 老年流感肺炎的临床特征及D-二聚体与疾病严重程度的相关性[J]. 北京大学学报(医学版), 2022, 54(1): 153-160. |
| [11] | 敖明昕,李学民,于媛媛,时会娟,黄红拾,敖英芳,王薇. 视觉重建对老年人行走动态足底压力的影响[J]. 北京大学学报(医学版), 2021, 53(5): 907-914. |
| [12] | 彭顺壮, 付茜茜, 冯星淋. 中国中老年居民教育程度与失能发生:社会参与的中介作用[J]. 北京大学学报(医学版), 2021, 53(3): 549-554. |
| [13] | 陈家丽,金月波,王一帆,张晓盈,李静,姚海红,何菁,李春. 老年发病类风湿关节炎的临床特征及其心血管疾病危险因素分析:一项大样本横断面临床研究[J]. 北京大学学报(医学版), 2020, 52(6): 1040-1047. |
| [14] | 陈健,左才红,张财义,杨明,张培训. 解剖型髓内钉和股骨近端防旋髓内钉治疗老年股骨转子间骨折的疗效比较[J]. 北京大学学报(医学版), 2019, 51(2): 283-287. |
| [15] | 徐小凤,陈茜,赵艺璞,胡秀英. 我国西部地区居家老年人生活自理能力调查分析[J]. 北京大学学报(医学版), 2018, 50(3): 457-462. |
|
||