北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (1): 153-160. doi: 10.19723/j.issn.1671-167X.2022.01.024
老年流感肺炎的临床特征及D-二聚体与疾病严重程度的相关性
- 1.北京大学人民医院急诊科,北京 100044
2.北京积水潭医院呼吸与危重症医学科,北京 100035
3.北京大学人民医院呼吸与危重症医学科,北京 100044
Clinical characteristics of influenza pneumonia in the elderly and relationship between D-dimer and disease severity
LI Jia1,XU Yu2,WANG You-ya3,GAO Zhan-cheng3,△( )
)
- 1. Department of Emergency, Peking University People’s Hospital, Beijing 100044, China
2. Department of Pulmonary and Critical Care Medicine, Beijing Jishuitan Hospital, Beijing 100035, China
3. Department of Pulmonary and Critical Care Medicine, Peking University People’s Hospital, Beijing 100044, China
摘要:
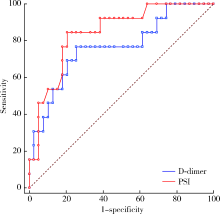
目的: 研究老年流感肺炎的临床特征以及D-二聚体与流感肺炎严重程度的相关性,以期提高临床医生对此类肺炎的甄别和管理。方法: 回顾性收集2014年起连续5个流感季(当年10月1日至次年3月31日)于北京大学人民医院诊断为流感肺炎的住院患者,年龄>65岁,收集患者的一般资料、临床症状、实验室检查、治疗方式及预后,比较重症和非重症肺炎的临床特点,分析D-二聚体与肺炎严重程度的关系,并应用受试者工作特征(receiver operating characteristic, ROC)曲线评估其预测流感肺炎死亡的效能。结果: 共纳入实验室确诊的老年流感肺炎住院患者52例,男性31例(59.6%),平均年龄(77.1±7.4)岁,符合重症肺炎诊断标准者19例(36.5%),约70%病例出现不同程度发热,重症肺炎组与非重症肺炎组相比,呼吸困难的发生率差异有统计学意义(14/19例,73.7% vs. 10/33例,30.3%,P=0.004),重症肺炎组的CURB-65(confusion, urea, respiratory rate, blood pressure, and age>65)评分、肺炎严重度指数(pneumonia severity index, PSI)评分、C反应蛋白、乳酸脱氢酶、尿素氮、空腹血糖、D-二聚体均高于非重症肺炎组,两组间差异有统计学意义(P值分别为0.004、<0.001、<0.001、0.003、0.038、0.018、<0.001),重症肺炎组的白蛋白则低于非重症肺炎组[(35.8±5.6) g/L vs. (38.9±3.5) g/L, t=-2.348,P=0.018]。入院首次检测的D-二聚体与PSI评分呈显著正相关(r=0.540, 95%CI:0.302~0.714,P<0.001),与氧合指数呈显著负相关(r=-0.559, 95%CI:-0.726-~0.330,P<0.001)。以患者是否住院期间死亡绘制ROC曲线,D-二聚体曲线下面积为0.765(95%CI:0.627~0.872),PSI曲线下面积为0.843(95%CI:0.716~0.929),二者相比,检验效能差异无统计学意义(Z=2.360,P=0.174)。D-二聚体>1 225 μg/L预测流感肺炎住院期间死亡的敏感性为76.92%,特异性为74.36%。结论: 高龄老年流感肺炎患者的发热症状不典型,呼吸困难是重症肺炎的突出表现,D-二聚体升高与老年流感肺炎严重程度相关,D-二聚体>1 200 μg/L对于老年重症流感肺炎住院期间死亡具有较好的预测价值。
中图分类号:
- R563.1
| [1] |
Luliano AD, Roguski KM, Chang HH, et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study[J]. Lancet, 2018, 391(10127):1285-1300.
doi: 10.1016/S0140-6736(17)33293-2 |
| [2] |
Gefenaite G, Pistol A, Popescu R, et al. Estimating burden of influenza-associated influenza-like illness and severe acute respiratory infection at public healthcare facilities in Romania during the 2011/12-2015/16 influenza seasons[J]. Influenza Other Respir Viruses, 2018, 12(1):183-192.
doi: 10.1111/irv.2018.12.issue-1 |
| [3] |
Loubet P, Samihlenzi N, Galtier F, et al. Factors associated with poor outcomes among adults hospitalized for influenza in France: A three-year prospective multicenter study[J]. J Clin Virol, 2016, 79:68-73.
doi: S1386-6532(16)30069-5 pmid: 27105315 |
| [4] | 中华人民共和国国家健康委员会. 流行性感冒诊疗方案(2018年版修订版)[J]. 中华临床感染病杂志, 2019, 12(1):1-5. |
| [5] | 中华医学会呼吸病学分会. 中国成人社区获得性肺炎诊断和治疗指南(2016年版)[J]. 中华结核和呼吸杂志, 2016, 39(4):253-279. |
| [6] | 中华医学会血液学分会血栓与止血学组. 弥散性血管内凝血诊断中国专家共识(2017年版)[J]. 中华血液学杂志, 2017, 38(5):361-363. |
| [7] | Palevsky PM, Liu KD, Brophy PD, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury[J]. Am J Kindney Dis, 2013, 61(5):649-672. |
| [8] |
Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008[J]. Crit Care Med, 2008, 36(1):296-327.
pmid: 18158437 |
| [9] |
Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: Advances in diagnosis and treatment[J]. JAMA, 2018, 319(7):698-710.
doi: 10.1001/jama.2017.21907 |
| [10] |
Childs A, Zullo AR, Joyce NR, et al. The burden of respiratory infections among older adults in long-term care: A systematic review[J]. BMC Geriatr, 2019, 19(1):210.
doi: 10.1186/s12877-019-1236-6 |
| [11] |
Chow EJ, Doyle JD, Uyeki TM. Influenza virus-related critical illness: prevention, diagnosis, treatment[J]. Crit Care, 2019, 23(1):214.
doi: 10.1186/s13054-019-2491-9 |
| [12] | Czaja CA, Miller L, Alden N, et al. Age-related differences in hospitalization rates, clinical presentation, outcomes among older adults hospitalized with influenza: U.S. Influenza Hospitalization Surveillance Network(FluSurv-NET)[J]. Open Forum Infect Dis, 2019, 6(7): ofz225. |
| [13] |
Matsuno O, Kataoka H, Takenaka R, et al. Influence of age on symptoms and laboratory findings at presentation in patients with influenza-associated pneumonia[J]. Arch Gerontol Geriatr, 2009, 49(2):322-325.
doi: 10.1016/j.archger.2008.11.015 |
| [14] |
Talbot HK. Influenza in older adults[J]. Infect Dis Clin North Am, 2017, 31(4):757-766.
doi: 10.1016/j.idc.2017.07.005 |
| [15] |
Aronen M, Viikari L, Kohonen I, et al. Respiratory tract virus infections in the elderly with pneumonia[J]. BMC Geriatrics, 2019, 19(1):111.
doi: 10.1186/s12877-019-1125-z pmid: 30991957 |
| [16] |
Chung JY, Hsu CC, Chen JH, et al. Shock index predicted mortality in geriatric patients with influenza in the emergency department[J]. Am J Emerg Med, 2019, 37(3):391-394.
doi: 10.1016/j.ajem.2018.05.059 |
| [17] |
van Asten L, Luna Pinzon A, de Lange DW, et al. Estimating severity of influenza epidemics from severe acute respiratory infections (SARI) in intensive care units[J]. Crit Care, 2018, 22(1):351.
doi: 10.1186/s13054-018-2274-8 |
| [18] |
Zhou F, Li H, Gu L, et al. Risk factors for nosocomial infection among hospitalised severe influenza A(H1N1)pdm09 patients[J]. Resp Med, 2018, 134:86-91.
doi: 10.1016/j.rmed.2017.11.017 |
| [19] |
Sahuquillo JM, Menéndez R, Méndez R, et al. Age-related risk factors for bacterial aetiology in community-acquired pneumonia[J]. Respirology, 2016, 21(8):1472-1479.
doi: 10.1111/resp.12851 pmid: 27417291 |
| [20] |
Daoud A, Laktineh A, Macrander C, et al. Pulmonary complications of influenza infection: A targeted narrative review[J]. Postgrad Med, 2019, 131(5):299-308.
doi: 10.1080/00325481.2019.1592400 pmid: 30845866 |
| [21] |
Nguyen JL, Yang W, Ito K, et al. Seasonal influenza infections and cardiovascular disease mortality[J]. JAMA Cardiol, 2016, 1(3):274-281.
doi: 10.1001/jamacardio.2016.0433 |
| [22] |
Kilic H, Kanbay A, Karalezli A, et al. Clinical characteristics of 75 pandemic H1N1 influenza patients from Turkey; risk factors for fatality[J]. Turk J Med Sci, 2015, 45(3):562-567.
doi: 10.3906/sag-1401-111 |
| [23] |
Ma S, Lai X, Chen Z, et al. Clinical characteristics of critically ill patients co-infected with SARS-CoV-2 and the influenza virus in Wuhan, China[J]. Int J Infect Dis, 2020, 96(1):683-687.
doi: 10.1016/j.ijid.2020.05.068 |
| [24] |
Zhang L, Yan X, Fan Q, et al. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19[J]. J Thromb Haemost, 2020, 18(6):1324-1329.
doi: 10.1111/jth.v18.6 |
| [25] |
Wang ZF, Su F, Lin XJ, et al. Serum D-dimer changes and prognostic implication in 2009 novel influenza A(H1N1)[J]. Thromb Res, 2011, 127(3):198-201.
doi: 10.1016/j.thromres.2010.11.032 pmid: 21216444 |
| [26] |
Kim MA, Park JS, Lee CW, et al. Pneumonia severity index in viral community acquired pneumonia in adults[J]. PLoS One, 2019, 14(3):e0210102.
doi: 10.1371/journal.pone.0210102 |
| [27] |
Dominguez-Cherit G, De la Torre A, Rishu A, et al. Influenza A(H1N1pdm09)-related critical illness and mortality in Mexico and Canada, 2014[J]. Crit Care Med, 2016, 44(10):1861-1870.
doi: 10.1097/CCM.0000000000001830 pmid: 27359085 |
| [1] | 李志昌,侯云飞,周之伟,姜龙,张舒,林剑浩. 影响全膝关节置换术患者术前预期的患者因素[J]. 北京大学学报(医学版), 2022, 54(1): 170-176. |
| [2] | 周传香,周正,张晔,刘晓筱,高岩. 28例口腔基底样鳞状细胞癌的临床病理分析[J]. 北京大学学报(医学版), 2022, 54(1): 62-67. |
| [3] | 孙玉春,郭雨晴,陈虎,邓珂慧,李伟伟. 口腔精准仿生修复技术的自主创新研发与转化[J]. 北京大学学报(医学版), 2022, 54(1): 7-12. |
| [4] | 王飞,朱翔,贺蓓,朱红,沈宁. 自发缓解的滤泡性细支气管炎伴非特异性间质性肺炎1例报道并文献复习[J]. 北京大学学报(医学版), 2021, 53(6): 1196-1200. |
| [5] | 孟洪,季丽娜,黄静,晁爽,周佳雯,李学军,尹小梅,樊丽容. COVID-19疫情前后北京市某综合医院儿科门诊患儿就诊量变化分析[J]. 北京大学学报(医学版), 2021, 53(5): 952-956. |
| [6] | 敖明昕,李学民,于媛媛,时会娟,黄红拾,敖英芳,王薇. 视觉重建对老年人行走动态足底压力的影响[J]. 北京大学学报(医学版), 2021, 53(5): 907-914. |
| [7] | 郭应禄. 夯实人才培养,实现我国泌尿外科奋斗目标[J]. 北京大学学报(医学版), 2021, 53(4): 633-634. |
| [8] | 尤鹏越,刘玉华,王新知,王思雯,唐琳. 脱细胞猪心包膜生物相容性及成骨性能的体内外评价[J]. 北京大学学报(医学版), 2021, 53(4): 776-784. |
| [9] | 刘承,马潞林. 前入路机器人辅助前列腺根治性切除术中改善排尿控制的经验[J]. 北京大学学报(医学版), 2021, 53(4): 635-639. |
| [10] | 郝瀚,刘越,陈宇珂,司龙妹,张萌,范宇,张中元,唐琦,张雷,吴士良,宋毅,林健,赵峥,谌诚,虞巍,韩文科. 机器人辅助前列腺癌根治术后患者的控尿恢复时间[J]. 北京大学学报(医学版), 2021, 53(4): 697-703. |
| [11] | 彭顺壮, 付茜茜, 冯星淋. 中国中老年居民教育程度与失能发生:社会参与的中介作用[J]. 北京大学学报(医学版), 2021, 53(3): 549-554. |
| [12] | 林瑜,吴静依,蔺轲,胡永华,孔桂兰. 基于集成学习模型预测重症患者再入重症监护病房的风险[J]. 北京大学学报(医学版), 2021, 53(3): 566-572. |
| [13] | 李远骋, 崔闻心, 郭雪儿, 朱璠, 刘思辰, 贾碧波, 汪培, 马迎华. 青年学生男男性行为人群中人类免疫缺陷病毒阳性与阴性者获得性免疫缺陷综合征(艾滋病)相关知识与行为比较[J]. 北京大学学报(医学版), 2021, 53(3): 511-517. |
| [14] | 刘晓强,杨洋,周建锋,刘明月,谭建国. 成年人后牙失去邻牙合接触后的三维位置变化[J]. 北京大学学报(医学版), 2021, 53(3): 594-597. |
| [15] | 陈平,黎泽明,郭怡,孙昕霙,Edwin B.FISHER. 基于大五人格理论应用潜在剖面分析探究2型糖尿病患者的用药依从性[J]. 北京大学学报(医学版), 2021, 53(3): 530-535. |
|