北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (4): 660-664. doi: 10.19723/j.issn.1671-167X.2019.04.011
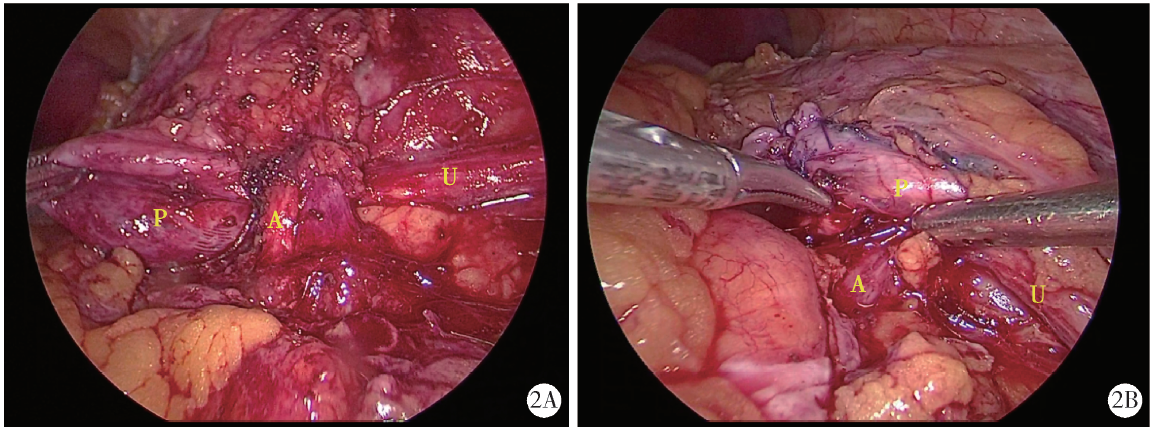
腹腔镜肾盂成型术中异位血管的处理方法
- 北京大学人民医院泌尿与碎石中心,北京 100034
Treatment of crossing vessels in laparoscopic pyeloplasty
Hai-yue ZHAO,Xiong-jun YE( ),Wei-nan CHEN,Li-zhe AN,Jun LIU,Liu-lin XIONG,Xiao-bo HUANG
),Wei-nan CHEN,Li-zhe AN,Jun LIU,Liu-lin XIONG,Xiao-bo HUANG
- Department of Urology and Lithotripsy Center, Peking University People’s Hospital, Beijing 100034, China
摘要:
目的:探讨腹腔镜肾盂成型术中对异位压迫血管的处理方法。方法:2016年1月至2018年6月共21例合并异位血管压迫的肾盂输尿管连接部狭窄(ureteropelvic junction obstruction, UPJO)患者在北京大学人民医院行腹腔镜肾盂成型术,其中男性15例、女性6例,平均年龄(33.9±15.0)岁,左侧13例、右侧8例。患者术前轻度肾积水4例、中度12例、重度5例。所有患者均行腹腔镜肾盂离断成型术(Anderson-Hynes术式),术中对于异位血管的处理采用Hem-o-lok悬吊(悬吊组14例)或将异位血管转位(转位组7例)两种方法,术后8周拔除双J管。收集患者临床资料(包括手术时间、异位血管处理时间、术中出血量、术后拔除引流管时间以及平均住院天数),术后对患者定期随访并进行手术效果评价。结果:所有患者的异位血管都得到成功保留,无一例在术中离断异位血管。本组平均手术时间(202.2±57.0) min,术中处理异位血管的平均时间(10.5±3.2) min,其中悬吊组为(6.1±2.0) min,转位组为(13.7±5.2) min。术中出血量(47.8±25.6) mL,术后拔除引流管时间(4.8±2.6) d,平均住院天数(11.5±3.3) d。术后发生轻微尿漏1例,所有患者术前患侧肾盂扩张(3.4±1.7) cm,术后3个月患侧肾盂扩张(1.9±1.3) cm,差异有统计学意义(P<0.05)。术后随访至2018年12月,所有患者肾脏大小无明显变化,肾积水均较术前有所缓解。结论:对于合并异位血管压迫的UPJO患者,在行肾盂成型术的同时,可以根据异位血管的位置采取Hem-o-lok悬吊或血管转位的方法来解除异位血管压迫,提高手术成功率。
中图分类号:
- R699.2
| [1] | Ellerkamp V, Kurth RR, Schmid E , et al. Differences between intrinsic and extrinsic ureteropelvic junction obstruction related to crossing vessels: histology and functional analyses[J]. World J Urol, 2016,34(4):577-583. |
| [2] | Zhang X, Li HZ, Wang SG , et al. Retroperitoneal laparoscopic dismembered pyeloplasty: experience with 50 eases[J]. Urology, 2005,66(3):514-517. |
| [3] | 张旭, 许凯, 张军 , 等. 后腹腔镜下Hellström术治疗异位血管导致的肾盂输尿管连接处狭窄[J]. 中华泌尿外科杂志, 2007,28(7):450-452. |
| [4] | 郭刚, 洪宝发, 符伟军 , 等. 肾迷走血管致肾盂输尿管连接部梗阻20例报告[J]. 临床泌尿外科杂志, 2003,18(12):721-723. |
| [5] | 王杭, 王国民 . CT尿路成像和IVU检查诊断泌尿系统疾病的比较研究[J]. 中华泌尿外科杂志, 2010,31(6):402-404. |
| [6] | Hellström J, Giertz G, Lindblom K . Pathogenesis and treatment of hydronephrosis[J]. J Belge Drol, 1951,20(1):1-6. |
| [7] | 中华医学会小儿外科学分会内镜外科学组. 腹腔镜肾盂输尿管连接部梗阻手术操作指南(2017版)[J]. 微创泌尿外科杂志, 2017,6(3):129-135. |
| [8] | 邱敏, 吴红章, 马潞林 , 等. 肾异位血管压迫引起肾盂输尿管连接部梗阻的临床诊治分析[J]. 中华外科杂志, 2014,52(9):702-705. |
| [9] | 宋宏程, 白继武, 黄澄如 , 等. 迷走血管压迫致梗阻性肾积水34例临床分析[J]. 临床小儿外科杂志, 2009,8(6):3-5. |
| [10] | Boylu U, Oommen M, Lee BR , et al. Ureteropelvic junction obstruction secondary to crossing vessels-to transpose or not? The robotic experience[J]. J Urol, 2009,181(4):1751-1755. |
| [1] | 邱敏,宗有龙,王滨帅,杨斌,徐楚潇,孙争辉,陆敏,赵磊,卢剑,刘承,田晓军,马潞林. 腹腔镜肾部分切除术治疗中高复杂程度肾肿瘤的效果[J]. 北京大学学报(医学版), 2023, 55(5): 833-837. |
| [2] | 刘慧丽,吕彦函,王晓晓,李民. 老年患者腹腔镜泌尿系肿瘤根治术后慢性疼痛的影响因素[J]. 北京大学学报(医学版), 2023, 55(5): 851-856. |
| [3] | 张铃福,侯纯升,徐智,王立新,凌晓锋,王港,崔龙,修典荣. 腹腔镜下经胆囊管胆管引流联合胆总管探查取石术治疗复杂胆管结石的临床效果[J]. 北京大学学报(医学版), 2022, 54(6): 1185-1189. |
| [4] | 安立哲,熊六林,陈亮,王焕瑞,陈伟男,黄晓波. 腹腔镜肾盂成形术联合肾盂镜超声碎石取石术治疗肾盂输尿管连接部梗阻合并肾结石[J]. 北京大学学报(医学版), 2022, 54(4): 746-750. |
| [5] | 张帆,陈曲,郝一昌,颜野,刘承,黄毅,马潞林. 术前及术后膜性尿道长度与腹腔镜根治性前列腺切除术后控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2022, 54(2): 299-303. |
| [6] | 张帆,黄晓娟,杨斌,颜野,刘承,张树栋,黄毅,马潞林. 前列腺尖部深度与腹腔镜前列腺癌根治术后早期控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2021, 53(4): 692-696. |
| [7] | 黄海文,闫兵,尚美霞,刘漓波,郝瀚,席志军. 女性膀胱癌患者腹腔镜膀胱全切术与开放膀胱全切术的倾向性评分匹配比较[J]. 北京大学学报(医学版), 2019, 51(4): 698-705. |
| [8] | 张铃福,侯纯升,黄永辉,徐智,王立新,凌晓锋,王港,崔龙,修典荣. 胃空肠吻合术后胆总管结石腹腔镜手术取石和内镜取石的比较[J]. 北京大学学报(医学版), 2019, 51(2): 345-348. |
| [9] | 徐奔,张喆楠,罗程,宋海峰,张骞. 后腹腔镜下肿瘤吸除术与肾部分切除术治疗肾血管平滑肌脂肪瘤的安全性与有效性对比[J]. 北京大学学报(医学版), 2018, 50(4): 700-704. |
| [10] | 王国良,叶剑飞,马潞林,黄毅,侯小飞,肖春雷,卢剑,洪锴,张树栋,赵磊,田晓军,. 腹腔镜前列腺癌根治术:无结技术与单结技术的回顾性对比研究[J]. 北京大学学报(医学版), 2017, 49(2): 361-364. |
| [11] | 叶雄俊,钟文龙,熊六林,马凯,徐涛,黄晓波,王晓峰. 后腹腔镜肾脂肪囊外肾蒂淋巴管结扎术治疗乳糜尿的疗效分析[J]. 北京大学学报(医学版), 2016, 48(4): 618-621. |
| [12] | 张洪宪,赵磊,马潞林,侯小飞,刘磊,邓绍辉. 后腹腔镜供肾切取自体肾移植术治疗复杂医源性输尿管损伤[J]. 北京大学学报(医学版), 2016, 48(4): 622-626. |
| [13] | 杨昆霖, 李学松, 周利群. 经腹腹腔镜输尿管体外裁剪、乳头再植术治疗成人梗阻性巨输尿管症的方法[J]. 北京大学学报(医学版), 2014, 46(4): 511-514. |
| [14] | 李清, 肖博, 刘士军, 徐涛, 王晓峰. 前列腺穿刺活检术后间隔时间对腹腔镜前列腺癌根治术的影响(附专家点评)[J]. 北京大学学报(医学版), 2014, 46(4): 532-536. |
| [15] | 张雷, 姚林, 李学松, 王天昱, 方冬, 张崔建, 蔡林, 谌诚, 周利群. 经腹腹腔镜肾切除手术的肾蒂处理技术:单一术者191例经验总结[J]. 北京大学学报(医学版), 2014, 46(4): 537-540. |
|
||