北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (6): 1056-1061. doi: 10.19723/j.issn.1671-167X.2019.06.014
术前贫血对上尿路尿路上皮癌预后的影响: 单中心686例患者回顾性研究
关豹1,翁迈2,凡航2,彭鼎1,方冬1,熊耕砚1,李学松1,△( ),周利群1
),周利群1
- 1. 北京大学第一医院泌尿外科,北京 100034
2. 武警北京总队医院泌尿外科,北京 100039
Evaluating the impact of preoperative anemia on the prognosis of upper tract urothelial carcinoma following radical nephroureterectomy: A single-center retrospective study of 686 patients
Bao GUAN1,Mai WENG2,Hang FAN2,Ding PENG1,Dong FANG1,Geng-yan XIONG1,Xue-song LI1,△( ),Li-qun ZHOU1
),Li-qun ZHOU1
- 1. Department of Urology, Peking University First Hospital, Beijing 100034, China
2. Department of Urology, Beijing Armed Police Corps Hospital, Beijing 100039, China
摘要:
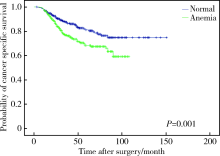
目的 评估术前血红蛋白水平与上尿路尿路上皮癌(upper tract urothelial carcinoma, UTUC)患者临床病理特征的关系及其对预后的预测价值。方法 回顾性收集北京大学第一医院泌尿外科2000年1月至2013年12月686例手术治疗的UTUC患者的临床病理资料及临床随访数据,患者血红蛋白水平测定均在入院第1天,并按照世界卫生组织国际贫血分类标准(男性血红蛋白<130 g/L,女性血红蛋白<120 g/L), 将患者分为贫血和正常血红蛋白水平两组,并使用SPSS 20.0进行统计学分析。结果 686例患者中,女性383(55.8%, 383/686)例,男性303(44.2%,303/686)例,中位年龄为68岁(四分位距:60~74岁), 术前贫血患者320例(46.6%,320/686)。术前贫血和患者性别(P = 0.002)、年龄(P < 0.001)、淋巴结转移(P = 0.026)、肿瘤分级(P = 0.018)、伴随原位癌(P = 0.038)、肿瘤组织坏死(P = 0.007)和肾功能状态(P < 0.001)显著相关。患者中位随访时间47个月(四分位距:31~75个月), 随访期间共有160例(23.3%,160/686)患者死亡,其中141例(20.6%,141/686)死于肿瘤,19(2.7%,19/686)例死于其他疾病或意外。单因素和多因素回归分析发现术前贫血是患者总生存(P<0.001,HR = 1.861)和肿瘤特异性生存(P = 0.003,HR = 1.688)的独立危险因素。结论 术前贫血是UTUC患者总生存和肿瘤特异性生存的独立预后因素。
中图分类号:
- R730.261
| [1] | Feng C, Wang L, Ding G , et al. Predictive value of clinicopathological markers for the metachronous bladder cancer and prognosis of upper tract urothelial carcinoma[J]. Sci Rep, 2014,4(6):4015. |
| [2] | Mehta R, Gillan AS, Ming ZY , et al. Socio-economic deprivation and outcomes following radical nephroureterectomy for clinically localized upper tract transitional cell carcinoma[J]. World J Urol, 2015,33(1):41-49. |
| [3] | Ishioka J, Saito K, Kijima T , et al. Risk stratification for bladder recurrence of upper urinary tract urothelial carcinoma after radical nephroureterectomy[J]. BJU Int, 2015,115(5):705-712. |
| [4] | Hamada S, Horiguchi A, Asano T , et al. Prognostic impact of fatty acid synthase expression in upper urinary tract urothelial carcinoma[J]. Jpn J Clin Oncol, 2014,44(5):486-492. |
| [5] | Rink M, Sharifi N, Fritsche HM , et al. Impact of preoperative anemia on oncologic outcomes of upper tract urothelial carcinoma treated with radical nephroureterectomy[J]. J Urol, 2014,191(2):316-322. |
| [6] | Krabbe LM, Westerman ME, Bagrodia A , et al. Surgical management of the distal ureter during radical nephroureterectomy is an independent predictor of oncological outcomes: results of a current series and a review of the literature[J]. Urol Oncol, 2014,32(1):54e19-54e26. |
| [7] | Chromecki TF, Cha EK, Fajkovic H , et al. The impact of tumor multifocality on outcomes in patients treated with radical nephroureterectomy[J]. Eur Urol, 2012,61(2):245-253. |
| [8] | Nutritional anaemias . Report of a WHO scientific group[J]. World Health Organ Tech Rep Ser, 1968,405:5-37. |
| [9] | Epstein JI, Amin MB, Reuter VR , et al. The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee[J]. Am J Surg Pathol, 1998,22(12):1435-1448. |
| [10] | Greene FL, Sobin LH . A worldwide approach to the TNM staging system: collaborative efforts of the AJCC and UICC[J]. J Surg Oncol, 2009,99(5):269-272. |
| [11] | Yeh HC, Chien TM, Wu WJ , et al. Is preoperative anemia a risk factor for upper tract urothelial carcinoma following radical nephroureterectomy?[J]. Urol oncol, 2016,34(8):337e331-337e339. |
| [12] | Lu YM, Li CC, Wu WJ , et al. Patients’ renal function is important when evaluating preoperative anemia in upper tract urothelial carcinoma[J]. Clin Genitourin Cancer, 2016,14(2):e241-e243. |
| [13] | Gilreath JA, Stenehjem DD, Rodgers GM . Diagnosis and treatment of cancer-related anemia[J]. Am J Hematol, 2014,89(2):203-212. |
| [14] | Gaspar BL, Sharma P, Das R . Anemia in malignancies: pathogenetic and diagnostic considerations[J]. Hematology, 2015,20(1):18-25. |
| [1] | 殳畅,韩烨,孙雨哲,杨再目,侯建霞. Ⅲ期牙周炎患者牙周基础治疗前后炎症性贫血相关指标的变化[J]. 北京大学学报(医学版), 2024, 56(1): 45-50. |
| [2] | 王薇,王佳宁,虞巍,朱赛楠,高莹,张俊清. 肾上腺性库欣综合征与无功能腺瘤患者的凝血功能比较及其影响因素[J]. 北京大学学报(医学版), 2023, 55(6): 1062-1067. |
| [3] | 林咏惟,周雅琳,赵润茏,许雅君,刘燕萍. 孕早期女性铁营养状况及其影响因素分析[J]. 北京大学学报(医学版), 2023, 55(4): 600-605. |
| [4] | 张崔建,何志嵩,周利群. 上尿路尿路上皮癌的淋巴清扫[J]. 北京大学学报(医学版), 2022, 54(4): 592-594. |
| [5] | 戴翔,王飞,杜依青,宋宇轩,徐涛. 上尿路尿路上皮癌组织中脂肪因子表达与临床病理特征及预后的相关性[J]. 北京大学学报(医学版), 2022, 54(4): 605-614. |
| [6] | 李志华,徐纯如,刘颖,贯华,张萌,车新艳,唐琦,黄燕波,李学松,周利群. 饮水习惯与上尿路尿路上皮癌病理特征的相关性分析[J]. 北京大学学报(医学版), 2022, 54(4): 621-627. |
| [7] | 樊理诗,高敏,Edwin B.FISHER,孙昕霙. 北京市通州区和顺义区747例2型糖尿病患者生存质量影响因素[J]. 北京大学学报(医学版), 2021, 53(3): 523-529. |
| [8] | 王兆年,高文静,王碧琦,曹卫华,吕筠,余灿清,逄增昌,丛黎明,汪华,吴先萍,刘彧,李立明. 成年双生子空腹血糖、糖化血红蛋白与全基因组DNA甲基化的相关性研究[J]. 北京大学学报(医学版), 2020, 52(3): 425-431. |
| [9] | 马闰卓,夏海缀,陆敏,张智荧,张启鸣,卢剑,王国良,马潞林. 输尿管镜活体组织检查对上尿路尿路上皮癌根治性手术的影响[J]. 北京大学学报(医学版), 2019, 51(4): 665-672. |
| [10] | 吴进锋,林榕城,林友成,蔡旺海,朱庆国,方冬,熊耕砚,张雷,周利群,叶烈夫,李学松. 肾输尿管全长切除术两种不同术式的双中心疗效对比[J]. 北京大学学报(医学版), 2019, 51(4): 646-652. |
| [11] | 杨超,王晋伟,杨尧政,白坤昊,高碧霞,赵明辉,张路霞,吴寿岭,王芳. 贫血及慢性肾脏病对糖尿病人群心脑血管事件发生与死亡的影响[J]. 北京大学学报(医学版), 2018, 50(3): 495-500. |
| [12] | 刘晓宇, 杨晓庆, 肖慧捷, 丁洁. 外周血无创总血红蛋白测定与静脉血血红蛋白检测在肾病患儿中的对比[J]. 北京大学学报(医学版), 2017, 49(5): 778-782. |
| [13] | 关豹,曹振朋,彭鼎,李一帆,詹永豪,刘漓波,何世明,熊耕砚,李学松,周利群. T2N0M0期上尿路尿路上皮癌患者预后相关因素分析:单中心235例患者回顾性研究[J]. 北京大学学报(医学版), 2017, 49(4): 603-607. |
| [14] | 曹亚英,唐迅,孙可欣,刘志科,项骁,隽娟,宋菁,殷琼洲,扎西德吉,胡亚楠,. 2型糖尿病患者血糖控制与内脏脂肪指数的关系[J]. 北京大学学报(医学版), 2017, 49(3): 446-450. |
| [15] | 宋逸,张冰,胡佩瑾,马军. 中国少数民族学生贫血现况及其与营养状况的关联研究[J]. 北京大学学报(医学版), 2016, 48(3): 429-435. |
|
||