北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (3): 573-579. doi: 10.19723/j.issn.1671-167X.2021.03.022
原发性甲状旁腺功能亢进症术后甲状旁腺激素升高9例并文献复习
- 中日友好医院内分泌科,北京 100029
Normocalcemic with elevated post-operative parathormone in primary hyperpara-thyroidism: 9 case reports and literature review
XIE Ling-ding,WANG Na,ZHANG Jin-ping,WANG Xin,CHEN Xiao-ping,ZHANG Bo,BU ShiΔ( )
)
- Department of Endocrinology, China-Japanese Friendship Hospital, Beijing 100029, China
摘要:
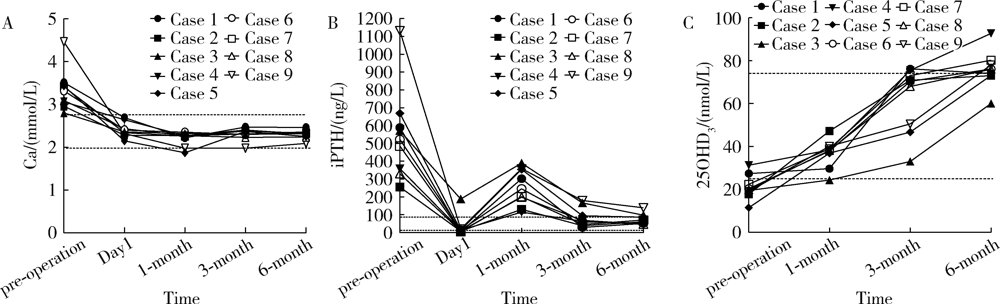
目的: 对经外科治疗后出现甲状旁腺激素(parathyroid hormone, PTH)升高伴正常血钙(normocalcemic parathormone elevation,NPE) 的原发性甲状旁腺功能亢进症(primary hyperparathyroidism,PHPT)患者的临床特征进行分析,提高该病的诊治能力,完善PHPT患者的术后管理。方法: 选取2017年8月至2019年11月中日友好医院内分泌科诊断为PHPT且术后6个月内出现NPE的9例患者作为研究对象,回顾性分析其临床资料和转归,并进行相关文献总结。结果: 临床特点:9例患者中6例为中老年女性,3例为男性。除1例为无症状性PHPT,其余8例主要临床表现为骨痛、肾结石及恶心、乏力。实验室检查:就诊时均血钙升高[(3.33±0.48) mmol/L],血磷降低[0.76 (0.74,0.78) mmol/L],24 h尿钙升高[8.1 (7.8,12.0) mmol/24 h],全片段甲状旁腺激素(intact parathyroid hormone, iPTH)明显升高[(546.1±257.7) ng/L],维生素D缺乏[25羟维生素D3水平(21.0±5.7) nmol/L],骨源性碱性磷酸酶[7例41.3 (38.6,68.4) μg/L,2例>90 μg/L]及N端中段骨钙素(>71.4 μg/L)明显升高,2例患者存在肾功能异常。影像学检查:7例骨质疏松,3例患者肾脏超声见肾结石。所有患者甲状旁腺影像学检查均发现明确病灶, 其中2例为多发病灶,7例为单发病灶。治疗及转归:2例患者行甲状旁腺切除术治疗,其余患者予甲状旁腺微波热消融治疗;术后1个月患者均出现PTH升高[(255.0±101.4) ng/L],血钙正常,甲状旁腺超声未发现复发病灶。给予钙剂及维生素D联合治疗至术后6个月,PTH均显著下降,术后血钙水平始终正常。结论: PHPT术后发生NPE与术前PTH高水平、维生素D缺乏及肾功能受损可能相关,但并不意味着PHPT的复发或者存在残余病灶;术后充足的钙剂及维生素D的补充可能使患者获益;应规范对PHPT患者的术后随访,以预防和治疗术后NPE。
中图分类号:
- R582.1
| [1] |
Silverberg SJ, Clarke BL, Peacock M, et al. Current issues in the presentation of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop[J]. J Clin Endocrinol Metab, 2014,99(10):3580-3594.
doi: 10.1210/jc.2014-1415 |
| [2] |
Sun B, Guo B, Wu B, et al. Characteristics, management, and outcome of primary hyperparathyroidism at a single clinical center from 2005 to 2016[J]. Osteoporos Int, 2018,29(3):635-642.
doi: 10.1007/s00198-017-4322-7 pmid: 29198075 |
| [3] |
Yao XA, Wei BJ, Jiang T, et al. The characteristics of clinical changes in primary hyperparathyroidism in Chinese patients[J]. J Bone Miner Metab, 2019,37(2):336-341.
doi: 10.1007/s00774-018-0922-3 |
| [4] | 中华医学会骨质疏松和骨矿盐疾病分会, 中华医学会内分泌分会代谢性骨病学组. 原发性甲状旁腺功能亢进症诊疗指南[J]. 中华骨质疏松和骨矿盐疾病杂志, 2014,7(3):187-198. |
| [5] |
Wei Y, Peng L, Li Y, et al. Clinical study on safety and efficacy of microwave ablation for primary hyperparathyroidism[J]. Korean J Radiol, 2020,21(5):572-581.
doi: 10.3348/kjr.2019.0593 |
| [6] |
Fan BQ, He XW, Chen HH, et al. US-guided microwave ablation for primary hyperparathyroidism: a safety and efficacy study[J]. Eur Radiol, 2019,29(10):5607-5616.
doi: 10.1007/s00330-019-06078-y |
| [7] |
Biskobing DM. Significance of elevated parathyroid hormone after parathyroidectomy[J]. Endocr Pract, 2010,16(1):112-117.
doi: 10.4158/EP09122.RA pmid: 19789155 |
| [8] |
Goldfarb M, Gondek S, Irvin GL, 3rd, et al. Normocalcemic parathormone elevation after successful parathyroidectomy: long-term analysis of parathormone variations over 10 years[J]. Surgery, 2011,150(6):1076-1084.
doi: 10.1016/j.surg.2011.09.017 pmid: 22136824 |
| [9] |
Carsello CB, Yen TW, Wang TS. Persistent elevation in serum parathyroid hormone levels in normocalcemic patients after parathyroidectomy: does it matter?[J]. Surgery, 2012,152(4):575-581.
doi: 10.1016/j.surg.2012.07.005 pmid: 23021134 |
| [10] |
Beyer TD, Solorzano CC, Prinz RA, et al. Oral vitamin D supplementation reduces the incidence of eucalcemic PTH elevation after surgery for primary hyperparathyroidism[J]. Surgery, 2007,141(6):777-783.
pmid: 17560254 |
| [11] |
Lang BH, Wong IY, Wong KP, et al. Eucalcemic parathyroid hormone elevation after parathyroidectomy for primary sporadic hyperparathyroidism: risk factors, trend, and outcome[J]. Ann Surg Oncol, 2012,19(2):584-590.
doi: 10.1245/s10434-011-1846-5 |
| [12] |
Duke WS, Kim AS, Waller JL, et al. Persistently elevated parathyroid hormone after successful parathyroid surgery[J]. Laryngoscope, 2017,127(7):1720-1723.
doi: 10.1002/lary.v127.7 |
| [13] |
Caldwell M, Laux J, Clark M, et al. Persistently elevated PTH after parathyroidectomy at one year: experience in a tertiary referral center[J]. J Clin Endocrinol Metab, 2019,104(10):4473-4480.
doi: 10.1210/jc.2019-00705 |
| [14] |
Westerdahl J, Valdemarsson S, Lindblom P, et al. Postoperative elevated serum levels of intact parathyroid hormone after surgery for parathyroid adenoma: sign of bone remineralization and decreased calcium absorption[J]. World J Surg, 2000,24(11):1323-1329.
pmid: 11038201 |
| [15] |
Cao S, Hu Y, Zhao Y, et al. A retrospective study of elevated post-operative parathormone in primary hyperparathyroid patients[J]. Oncotarget, 2017,8(60):101158-101164.
doi: 10.18632/oncotarget.v8i60 |
| [16] |
Nordenstrom E, Westerdahl J, Isaksson A, et al. Patients with elevated serum parathyroid hormone levels after parathyroidectomy: showing signs of decreased peripheral parathyroid hormone sensiti-vity[J]. World J Surg, 2003,27(2):212-215.
doi: 10.1007/s00268-002-6600-5 |
| [17] |
Mittendorf EA, McHenry CR. Persistent parathyroid hormone elevation following curative parathyroidectomy for primary hyperparathyroidism[J]. Arch Otolaryngol Head Neck Surg, 2002,128(3):275-279.
doi: 10.1001/archotol.128.3.275 |
| [18] |
Rianon N, Alex G, Callender G, et al. Preoperative serum osteocalcin may predict postoperative elevated parathyroid hormone in patients with primary hyperparathyroidism[J]. World J Surg, 2012,36(6):1320-1326.
doi: 10.1007/s00268-012-1432-4 pmid: 22278606 |
| [19] | Silverberg SJ, Gartenberg F, Jacobs TP, et al. Increased bone mineral density after parathyroidectomy in primary hyperparathyroidism[J]. J Clin Endocrinol Metab, 1995,80(3):729-734. |
| [20] |
Ning L, Sippel R, Schaefer S, et al. What is the clinical significance of an elevated parathyroid hormone level after curative surgery for primary hyperparathyroidism?[J]. Ann Surg, 2009,249(3):469-472.
doi: 10.1097/SLA.0b013e31819a6ded |
| [21] |
Wang TS, Ostrower ST, Heller KS. Persistently elevated parathyroid hormone levels after parathyroid surgery[J]. Surgery, 2005,138(6):1130-1135.
doi: 10.1016/j.surg.2005.08.026 |
| [22] |
Carty SE, Roberts MM, Virji MA, et al. Elevated serum parathormone level after “concise parathyroidectomy” for primary sporadic hyperparathyroidism[J]. Surgery, 2002,132(6):1086-1092.
doi: 10.1067/msy.2002.128479 |
| [23] |
Press D, Politz D, Lopez J, et al. The effect of vitamin D levels on postoperative calcium requirements, symptomatic hypocalcemia, and parathormone levels following parathyroidectomy for primary hyperparathyroidism[J]. Surgery, 2011,150(6):1061-1068.
doi: 10.1016/j.surg.2011.09.018 |
| [24] |
Aberg V, Norenstedt S, Zedenius J, et al. Health-related quality of life after successful surgery for primary hyperparathyroidism: no additive effect from vitamin D supplementation: results of a double-blind randomized study[J]. Eur J Endocrinol, 2015,172(2):181-187.
doi: 10.1530/EJE-14-0757 |
| [25] |
Norenstedt S, Pernow Y, Zedenius J, et al. Vitamin D supplementation after parathyroidectomy: effect on bone mineral density: a randomized double-blind study[J]. J Bone Miner Res, 2014,29(4):960-967.
doi: 10.1002/jbmr.v29.4 |
| [26] |
Rolighed L, Rejnmark L, Sikjaer T, et al. Vitamin D treatment in primary hyperparathyroidism: a randomized placebo controlled trial[J]. J Clin Endocrinol Metab, 2014,99(3):1072-1080.
doi: 10.1210/jc.2013-3978 |
| [27] |
Grubbs EG, Rafeeq S, Jimenez C, et al. Preoperative vitamin D replacement therapy in primary hyperparathyroidism: safe and beneficial?[J]. Surgery, 2008,144(6):852-858.
doi: 10.1016/j.surg.2008.06.032 |
| [28] |
de la Plaza Llamas R, Ramia Angel JM, Arteaga Peralta V, et al. Elevated parathyroid hormone levels after successful parathyroidectomy for primary hyperparathyroidism: a clinical review[J]. Eur Arch Otorhinolaryngol, 2018,275(3):659-669.
doi: 10.1007/s00405-017-4836-9 |
| [1] | 靖婷,江华,李婷,申倩倩,叶兰,曾银丹,梁文欣,冯罡,司徒文佑,张玉梅. 中国西部5城市中老年人血清25羟基维生素D与握力的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 448-455. |
| [2] | 鲍雷,蔡夏夏,张明远,任磊磊. 维生素D3对2型糖尿病小鼠轻度认知障碍的改善作用及机制研究[J]. 北京大学学报(医学版), 2023, 55(4): 587-592. |
| [3] | 孙希雅,陈艺璐,曾琳,闫丽盈,乔杰,李蓉,智旭. 不孕女性维生素D水平与抗苗勒氏管激素的相关性及对妊娠结局的预测[J]. 北京大学学报(医学版), 2023, 55(1): 167-173. |
| [4] | 何伟,杨思雯,陈娟,朱晓俊,陈志忠,马文军. 275 nm和310 nm紫外线对去卵巢骨质疏松大鼠骨代谢的影响[J]. 北京大学学报(医学版), 2022, 54(2): 236-243. |
| [5] | 邹健梅,武丽君,罗采南,石亚妹,吴雪. 血清25-羟维生素D与系统性红斑狼疮活动的关系[J]. 北京大学学报(医学版), 2021, 53(5): 938-941. |
| [6] | 刘凯宁,孟焕新,侯建霞. 维生素D受体FokⅠ多态性对牙周组织细胞CYP24A1表达的影响[J]. 北京大学学报(医学版), 2018, 50(1): 13-19. |
| [7] | 曹晓静, 和璐, 孟焕新, 李蓬, 陈智滨. 维生素D受体基因多态性与慢性牙周炎的相关性[J]. 北京大学学报(医学版), 2015, 47(4): 697-702. |
| [8] | 卓滋泽, 刘玲, 马文军, 赵茜, 赵欣, 王永志, 张国义. 长波紫外线和中波紫外线对去卵巢骨质疏松大鼠1,25-二羟基维生素D3和骨代谢影响的比较[J]. 北京大学学报(医学版), 2013, 45(03): 392-397. |
|
||