北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 871-876. doi: 10.19723/j.issn.1671-167X.2021.05.010
膝关节前交叉韧带断裂后单腿位置觉测试时脑电功率谱的变化特征
- 北京大学第三医院运动医学科,北京大学运动医学研究所,运动医学关节伤病北京市重点实验室,北京 100191
Changes of electroencephalography power spectrum during joint position perception test after anterior cruciate ligament rupture
MIAO Xin,HUANG Hong-shi,HU Xiao-qing,SHI Hui-juan,REN Shuang,AO Ying-fang( )
)
- Department of Sports Medicine, Peking University Third Hospital, Institute of Sports Medicine of Peking University,Beijing Key Laboratory of Sports Injuries, Beijing 100191, China
摘要:
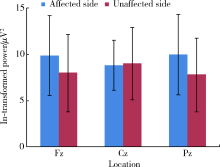
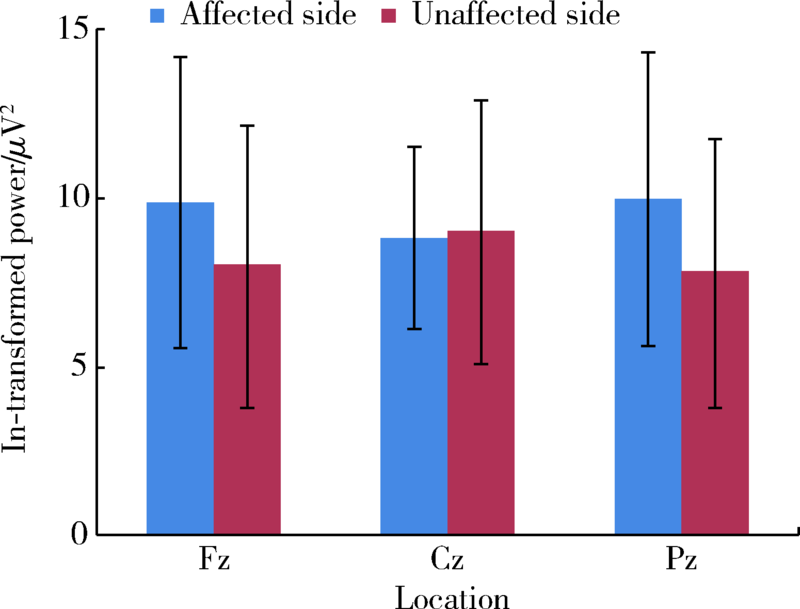
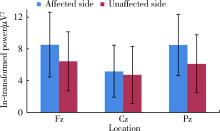
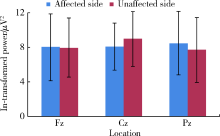
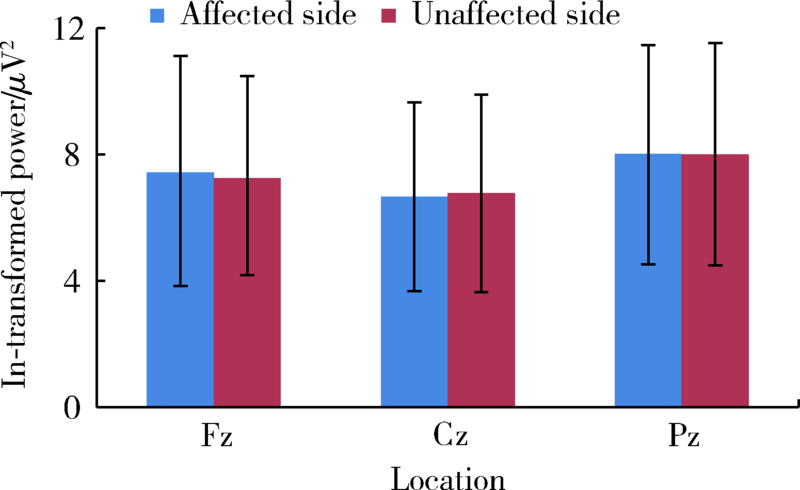
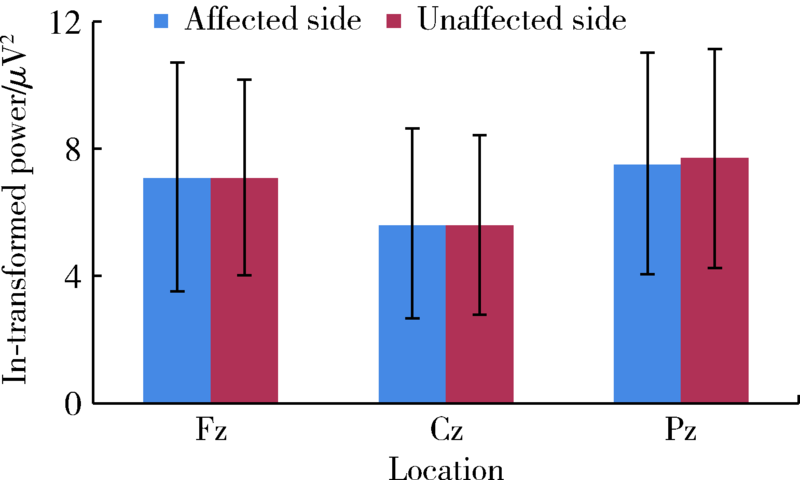
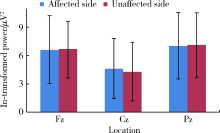
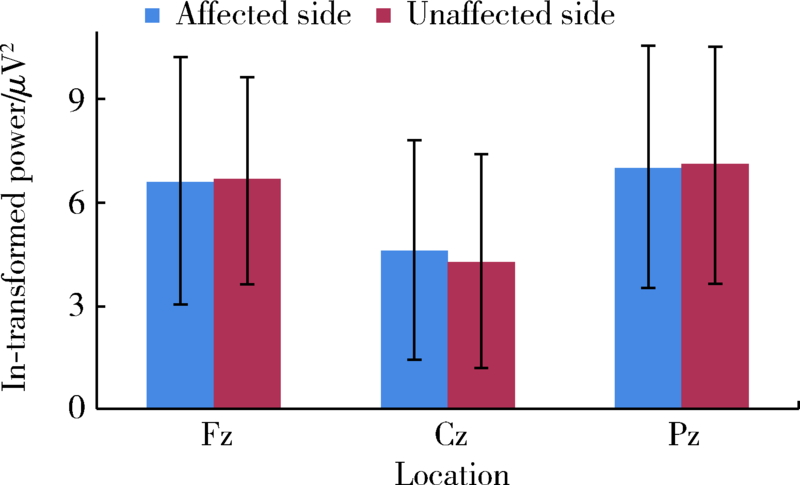
目的: 同步记录膝关节前交叉韧带(anterior cruciate ligament,ACL)断裂患者进行单腿位置觉测试时的脑电信号,分析ACL断裂人群未伤侧、患侧分别运动时的脑电差异,明确ACL断裂造成的脑电功率谱变化特征,探究前交叉韧带断裂、膝关节失稳的中枢神经机制,为治疗及康复提供理论依据。方法: 选择北京大学第三医院运动医学科2014年11月—2015年4月收治的一侧单纯ACL断裂男性患者16例参与研究,使用等速肌力测试设备进行单侧主动膝关节位置觉运动和被动膝关节位置觉运动。同步记录ACL断裂人群未伤侧和患侧被动膝关节位置觉测试、主动膝关节位置觉测试的脑电功率谱(electroencephalography,EEG), 分析ACL断裂侧和非损伤侧单独运动时患者不同频段的脑电功率差异。主动膝关节位置觉任务和被动膝关节位置觉任务的目标位置为屈膝30°位。结果: ACL断裂人群未伤侧运动和患侧单独进行主动、被动膝关节位置觉测试发现,被动关节位置觉运动时,患侧较未伤侧脑电功率谱的Delta[ F (1, 15)=0.003, P=0.957,
中图分类号:
- R686
| [1] | 钱菁华. 功能性踝关节不稳的神经肌肉控制机制及PNF干预效果研究 [D]. 北京:北京体育大学, 2016. |
| [2] |
Schultz RA, Miller DC, Kerr C, et al. Mechanoreceptors in human cruciate ligaments. A histological study [J]. J Bone Joint Surg Am, 1984, 66(7):1072-1076.
pmid: 6207177 |
| [3] |
Zimny ML, Schutte M, Dabezies E. Mechanoreceptors in the human anterior cruciate ligament [J]. Anat Rec, 1986, 214(2):204-209.
pmid: 3954077 |
| [4] |
Johansson H, Sjölander P, Sojka P. Receptors in the knee joint ligaments and their role in the biomechanics of the joint [J]. Crit Rev Biomed Eng, 1991, 18(5):341-368.
pmid: 2036801 |
| [5] |
Friden T, Roberts D, Ageberg E, et al. Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture [J]. J Orthop Sport Phys Ther, 2001, 31(10):567-576.
doi: 10.2519/jospt.2001.31.10.567 |
| [6] |
Valeriani M, Restuccia D, Di Lazzaro V, et al. Clinical and neurophysiological abnormalities before and after reconstruction of the anterior cruciate ligament of the knee [J]. Acta Neurol Scand, 1999, 99(5):303-307.
pmid: 10348160 |
| [7] |
Borsa PA, Lephart SM, Irrgang JJ, et al. The effects of joint position and direction of joint motion on proprioceptive sensibility in anterior cruciate ligament-deficient athletes [J]. Am J Sports Med, 1997, 25(3):336-340.
doi: 10.1177/036354659702500311 |
| [8] |
Fremerey RW, Lobenhoffer P, Zeichen J, et al. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study [J]. J Bone Joint Surg Br, 2000, 82(6):801-806.
pmid: 10990300 |
| [9] |
Miao X, Huang H, Hu X, et al. The characteristics of EEG power spectra changes after ACL rupture [J]. PLoS One, 2017, 12(2):e0170455.
doi: 10.1371/journal.pone.0170455 |
| [10] |
Baumeister J, Reinecke K, Weiss M. Changed cortical activity after anterior cruciate ligament reconstruction in a joint position paradigm: an EEG study [J]. Scand J Med Sci Sports, 2008, 18(4):473-484.
doi: 10.1111/j.1600-0838.2007.00702.x |
| [11] | Hewett T, Paterno M, Noyes F. Differences in single leg balance on an unstable platform between female and male normal, ACL-deficient and ACL-reconstructed knees. Proprioception and neuromuscular control in joint stability [M]. Champaign, Illinois: Human Kinetics, 1999: 77-88. |
| [12] |
Corrigan JP, Cashman WF, Brady MP. Proprioception in the cruciate deficient knee [J]. J Bone Joint Surg Br, 1992, 74(2):247-250.
pmid: 1544962 |
| [13] |
Fridén T, Zätterström R, Lindstrand A, et al. A stabilometric technique for evaluation of lower limb instabilities [J]. Am J Sports Med, 1989, 17(1):118-122.
doi: 10.1177/036354658901700120 |
| [14] |
Wojtys EM, Huston LJ. Neuromuscular performance in normal and anterior cruciate ligament-deficient lower extremities [J]. Am J Sports Med, 1994, 22(1):89-104.
doi: 10.1177/036354659402200116 |
| [1] | 孟广艳,张筠肖,张渝昕,刘燕鹰. IgG4相关性疾病中枢神经系统受累的临床特点分析[J]. 北京大学学报(医学版), 2021, 53(6): 1043-1048. |
| [2] | 许力,胡明洁,李玉玉,屈洪党,钱伟东,刘晓林. 圆锥马尾部黏液乳头型室管膜瘤继发中枢神经系统表面铁沉积症1例报道及文献复习[J]. 北京大学学报(医学版), 2019, 51(4): 769-774. |
| [3] | 杨丹,乔琳,赵丽丹. 原发干燥综合征伴发脑梗塞1例报告附文献复习[J]. 北京大学学报(医学版), 2016, 48(6): 1077-1080. |
| [4] | 漆学良, 陈静, 郑日亮, 李颖, 黄一宁, 袁云. 可缓解和复发的瘤样炎性脱髓鞘病1例[J]. 北京大学学报(医学版), 2009, 41(5): 588-589. |
| [5] | 王洪涛, 周站云, 王凤荣, 豆波建, 王孝伟, 刘俊义. 中枢神经保护剂--四环素类化合物C2位衍生物的设计与合成[J]. 北京大学学报(医学版), 2004, 36(5): 550-551. |
| [6] | 谢英, 叶丽亚, 张小滨, 侯新朴, 娄晋宁. 血脑屏障体外实验模型的建立[J]. 北京大学学报(医学版), 2004, 36(4): 435-438. |
|
||