北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (2): 299-307. doi: 10.19723/j.issn.1671-167X.2023.02.014
411例早期胃癌及癌前病变内镜黏膜下剥离术标本的病理学评估
刘菊梅1,梁丽1,张继新1,戎龙2,张梓怡1,吴悠1,赵旭东2,李挺1,*( )
)
- 1. 北京大学第一医院病理科,北京 100034
2. 北京大学第一医院内镜中心,北京 100034
Pathological evaluation of endoscopic submucosal dissection for early gastric cancer and precancerous lesion in 411 cases
Ju-mei LIU1,Li LIANG1,Ji-xin ZHANG1,Long RONG2,Zi-yi ZHANG1,You WU1,Xu-dong ZHAO2,Ting LI1,*( )
)
- 1. Department of Pathology, Peking University First Hospital, Beijing 100034, China
2. Center of Endoscopy, Peking University First Hospital, Beijing 100034, China
摘要:
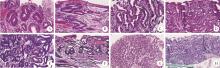
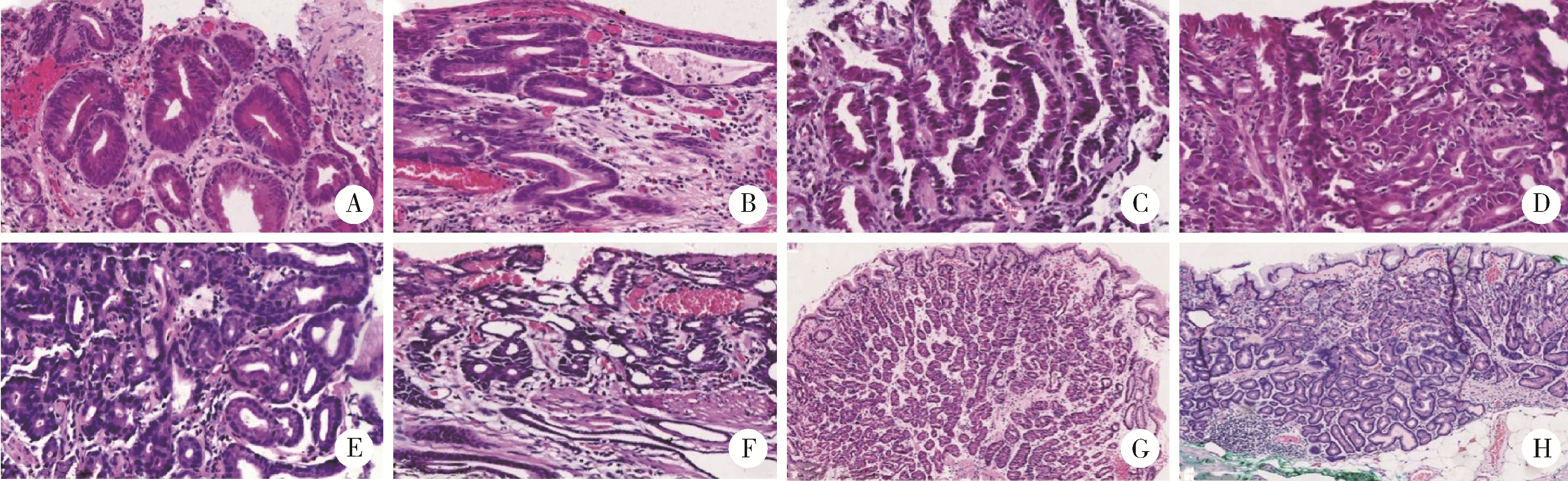
目的: 评估早期胃癌及癌前病变内镜黏膜下剥离术(endoscopic submucosal dissection,ESD)标本的病理学特征,为临床诊疗及病理学分析积累经验。方法: 按日本早期胃癌ESD治疗指南和日本胃癌分类和处理指南,回顾性分析2013年9月至2021年12月北京大学第一医院ESD治疗的411例早期胃癌或癌前病变临床病理资料、病理诊断评估、术前胃镜活检(400例)与ESD术后组织病理学诊断符合情况,以及非治愈切除危险因素等。结果: 411例中,96例(23.4%)为腺瘤(WHO低级别异型增生),315例(76.6%)为早期胃癌,后者包括115例(28.0%)非浸润性癌(WHO高级别异型增生)和200例(48.7%)浸润性癌。术前活检与术后组织病理学诊断符合率为66.0%(264/400)。ESD前后诊断符合率与组织学类型及病变部位相关(P < 0.01)。ESD术后组织病理学诊断升级119例(29.8%)、降级17例(4.2%)。315例早期胃癌中,组织学分类的分化型癌277例(87.9%),未分化型癌38例(12.1%);绝对适应证262例(83.2%),相对适应证53例(16.8%);整块切除率98.1%,治愈性切除率82.9%。非治愈性切除的独立危险因素包括病变最大径>20 mm(OR=3.631,95%CI: 1.170~11.270,P=0.026)、肿瘤浸润至黏膜下层(OR=69.761,95%CI: 21.033~231.376,P < 0.001),以及组织学分类为未分化型癌(OR=16.950,95%CI: 4.585~62.664,P < 0.001)。结论: 活检标本局限性、病变特点和分布、病理认识、内镜观察取材等主客观因素可导致术前活检与ESD术后组织病理学诊断存在差异,尤其术后升级诊断更显著,应引起内镜中心与病理科医生的重视。ESD手术早期胃癌治愈率高,非治愈性切除与病变最大径、肿瘤浸润深度及组织学类型相关。未分化型早期胃癌符合适应证标准也可实施ESD。ESD手术标本的全面及规范化病理学分析对ESD手术疗效及患者预后评估具有临床指导意义。
中图分类号:
- R735.2
| 1 |
Japanese Gastric Cancer Association . Japanese gastric cancer treatment guidelines 2018 (5th edition)[J]. Gastric Cancer, 2021, 24 (1): 1- 21.
doi: 10.1007/s10120-020-01042-y |
| 2 |
Banks M , Graham D , Jansen M , et al. British society of gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma[J]. Gut, 2019, 68 (9): 1545- 1575.
doi: 10.1136/gutjnl-2018-318126 |
| 3 |
北京市科委重大项目《早期胃癌治疗规范研究》专家组. 早期胃癌内镜下规范化切除的专家共识意见(2018, 北京)[J]. 中华消化内镜杂志, 2018, 36 (6): 381- 392.
doi: 10.3760/cma.j.issn.1007-5232.2018.06.001 |
| 4 |
赫捷, 陈万青, 李兆申, 等. 中国胃癌筛查与早诊早治指南制定专家组, 中国胃癌筛查与早诊早治指南制定工作组.中国胃癌筛查与早诊早治指南(2022, 北京)[J]. 中华消化外科杂志, 2022, 21 (7): 827- 851.
doi: 10.3760/cma.j.cn115610-20220624-00370 |
| 5 |
Lim H , Jung HY , Park YS , et al. Discrepancy between endos-copic forceps biopsy and endoscopic resection in gastric epithelial neoplasia[J]. Surg Endosc, 2014, 28 (4): 1256- 1262.
doi: 10.1007/s00464-013-3316-6 |
| 6 |
Lu C , Lv X , Lin Y , et al. Retrospective study: The diagnostic accuracy of conventional forceps biopsy of gastric epithelial compared to endoscopic submucosal dissection (STROBE compliant)[J]. Medicine, 2016, 95 (30): e4353.
doi: 10.1097/MD.0000000000004353 |
| 7 |
Wu S , Zhu X , Xiang L , et al. The Diagnostic accuracy of conventional forceps biopsy compared to ESD[J]. Open medicine (Warsaw, Poland), 2017, 12, 261- 265.
doi: 10.1515/med-2017-0039 |
| 8 |
Ono H , Yao K , Fujishiro M , et al. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer (second edition)[J]. Dig Endosc, 2021, 33 (1): 4- 20.
doi: 10.1111/den.13883 |
| 9 |
梁丽, 张继新, 戎龙, 等. 80例早期胃癌及癌前病变内镜黏膜下剥离术标本的处理及病理学评估[J]. 中华消化内镜杂志, 2016, 33 (9): 589- 597.
doi: 10.3760/cma.j.issn.1007-5232.2016.09.004 |
| 10 |
梁丽, 于妍斐, 张继新, 等. 113例早期结直肠癌及癌前病变内镜黏膜下剥离术标本处理及病理学评估[J]. 中华消化内镜杂志, 2018, 35 (7): 470- 476.
doi: 10.3760/cma.j.issn.1007-5232.2018.07.004 |
| 11 |
Nagtegaal ID , Odze RD , Klimstra D , et al. The 2019 WHO classification of tumours of the digestive system[J]. Histopathology, 2020, 76 (2): 182- 188.
doi: 10.1111/his.13975 |
| 12 |
Sano T , Aiko T . New Japanese classifications and treatment guidelines for gastric cancer: Revision concepts and major revised points[J]. Gastric Cancer, 2011, 14 (2): 97- 100.
doi: 10.1007/s10120-011-0040-6 |
| 13 |
Sung H , Ferlay J , Siegel RL , et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71 (3): 209- 249.
doi: 10.3322/caac.21660 |
| 14 |
Ito Y , Miyashiro I , Ishikawa T , et al. Determinant factors on differences in survival for gastric cancer between the United States and Japan using nationwide databases[J]. J Epidemiol, 2021, 31 (4): 241- 248.
doi: 10.2188/jea.JE20190351 |
| 15 |
Hong S , Won YJ , Lee JJ , et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2018[J]. Cancer Res Treat, 2021, 53 (2): 301- 315.
doi: 10.4143/crt.2021.291 |
| 16 | 曹晖, 张子臻, 赵恩昊, 等. 对早期胃癌内镜治疗的评价、思考及展望[J]. 中国实用外科杂志, 2022, 42 (10): 1097- 1103. |
| 17 |
Hasuike N , Ono H , Boku N , et al. A non-randomized confirmatory trial of an expanded indication for endoscopic submucosal dissection for intestinal-type gastric cancer (cT1a): The Japan clinical oncology group study (JCOG0607)[J]. Gastric Cancer, 2018, 21 (1): 114- 123.
doi: 10.1007/s10120-017-0704-y |
| 18 |
Lee CK , Chung IK , Lee SH , et al. Is endoscopic forceps biopsy enough for a definitive diagnosis of gastric epithelial neoplasia[J]. J Gastroenterol Hepatol, 2010, 25 (9): 1507- 1513.
doi: 10.1111/j.1440-1746.2010.006367.x |
| 19 |
Zhao G , Xue M , Hu Y , et al. How Commonly is the diagnosis of gastric low grade dysplasia upgraded following endoscopic resection? A meta-analysis[J]. PLoS One, 2015, 10 (7): e0132699.
doi: 10.1371/journal.pone.0132699 |
| 20 |
Jung SH , Chung WC , Lee KM , et al. Risk factors in malignant transformation of gastric epithelial neoplasia categorized by the revised Vienna classification: endoscopic, pathological, and immunophenotypic features[J]. Gastric Cancer, 2010, 13 (2): 123- 130.
doi: 10.1007/s10120-010-0550-7 |
| 21 |
Sung JK . Diagnosis and management of gastric dysplasia[J]. Korean J Intern Med, 2016, 31 (2): 201- 209.
doi: 10.3904/kjim.2016.021 |
| 22 |
国家消化系疾病临床医学研究中心(上海), 国家消化道早癌防治中心联盟, 中华医学会消化病学分会幽门螺杆菌学组, 等. 中国胃黏膜癌前状态和癌前病变的处理策略专家共识(2020年)[J]. 中华消化杂志, 2020, 40 (11): 731- 741.
doi: 10.3760/cma.j.cn311367-20200915-00554 |
| 23 | De Marco MO , Tustumi F , Brunaldi VO , et al. Prognostic factors for ESD of early gastric cancers: A systematic review and meta-analysis[J]. Endosc Int Open, 2020, 8 (9): e1144- e1155. |
| [1] | 熊焰,张波,聂立功,吴世凯,赵虎,李东,邸吉廷. 胸部SMARCA4缺失性未分化肿瘤的病理诊断与联合免疫检测点抑制剂治疗[J]. 北京大学学报(医学版), 2023, 55(2): 351-356. |
| [2] | 侯卫华,宋书杰,石中月,金木兰. 幽门螺杆菌阴性早期胃癌的临床病理特征[J]. 北京大学学报(医学版), 2023, 55(2): 292-298. |
| [3] | 武颖超,蔡云龙,戎龙,张继新,刘金,汪欣. 早期胃癌淋巴结转移规律及内镜黏膜下剥离术治疗早期胃癌的疗效评价[J]. 北京大学学报(医学版), 2020, 52(6): 1093-1097. |
| [4] | 刘鑫,张静,王晔,张贺军,丁士刚,周丽雅. 早期胃癌白光内镜下特征分析[J]. 北京大学学报(医学版), 2019, 51(2): 302-306. |
| [5] | 李士杰,王警,李子禹,步召德,苏向前,李忠武,吴齐. 内镜黏膜下剥离术在早期胃癌治疗中的应用[J]. 北京大学学报(医学版), 2015, 47(6): 945-951. |
|
||