北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (5): 788-793. doi: 10.19723/j.issn.1671-167X.2024.05.006
尿促黄体生成素在女童中枢性性早熟预测中的应用
- 北京大学第三医院儿科, 北京 100191
Application of urinary luteinizing hormone in the prediction of central precocious puberty in girls
Jinfang YUAN, Xinli WANG*( ), Yunpu CUI, Xuemei WANG
), Yunpu CUI, Xuemei WANG
- Department of Pediatrics, Peking University Third Hospital, Beijing 100191, China
摘要:
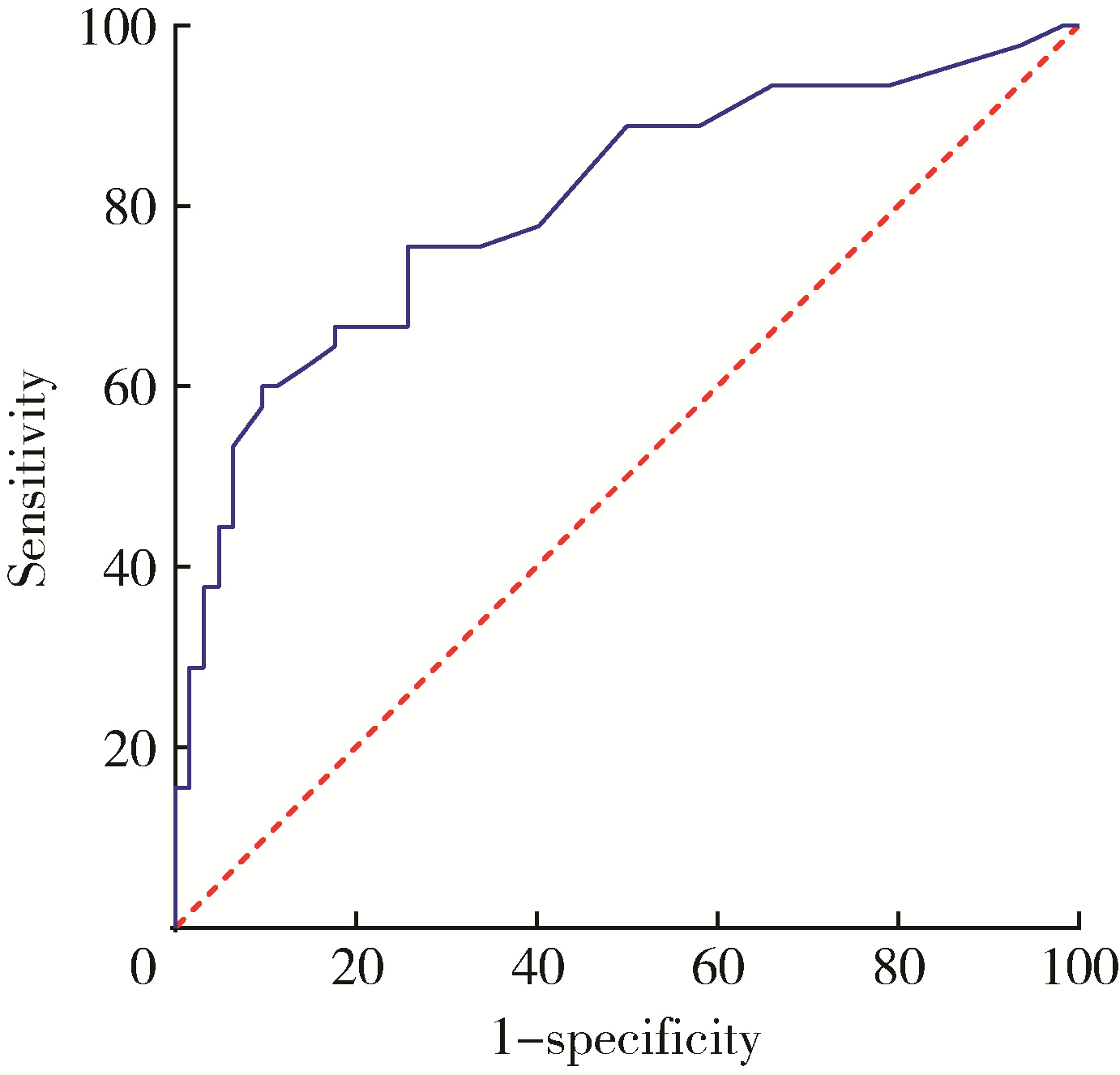
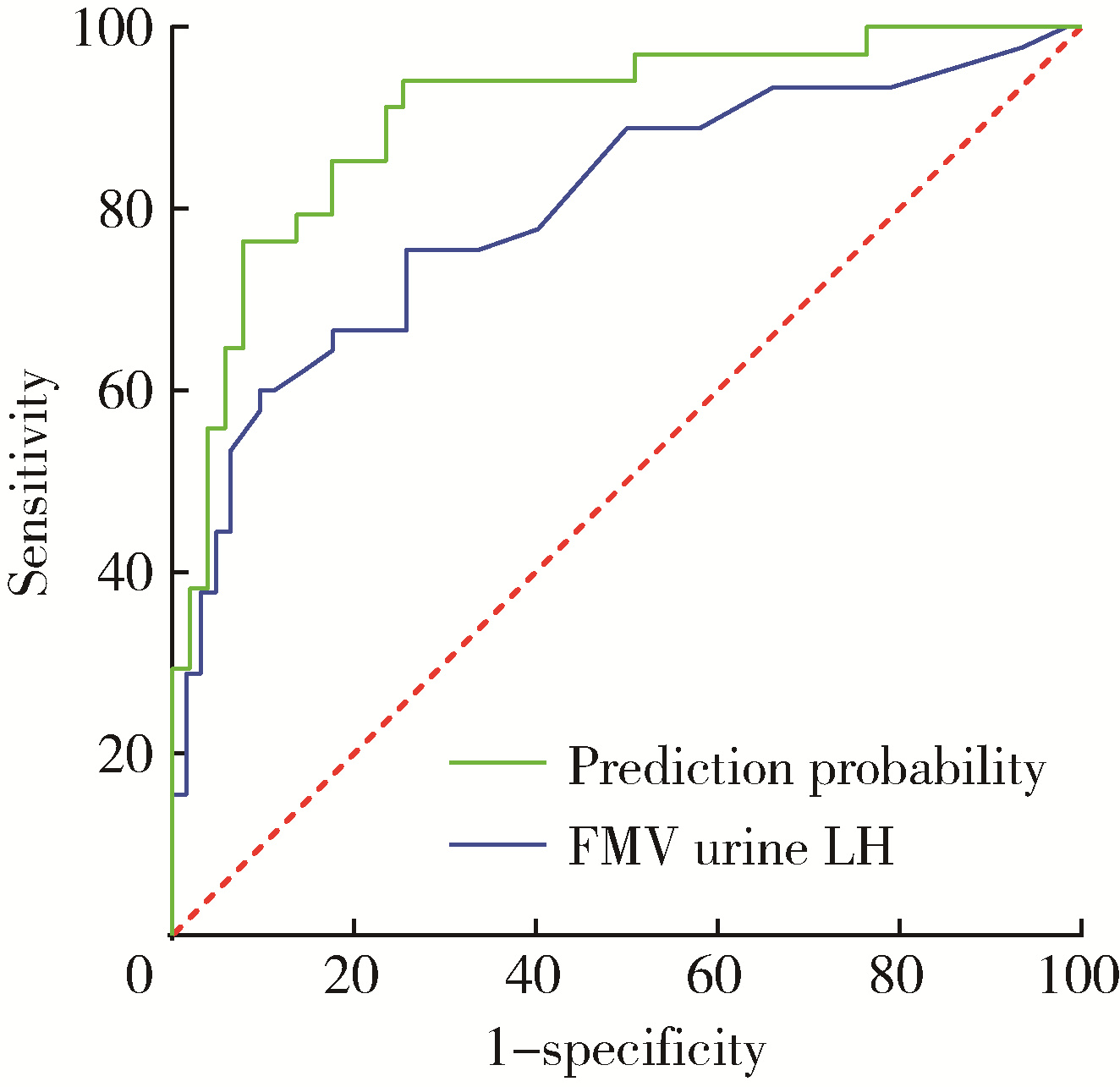
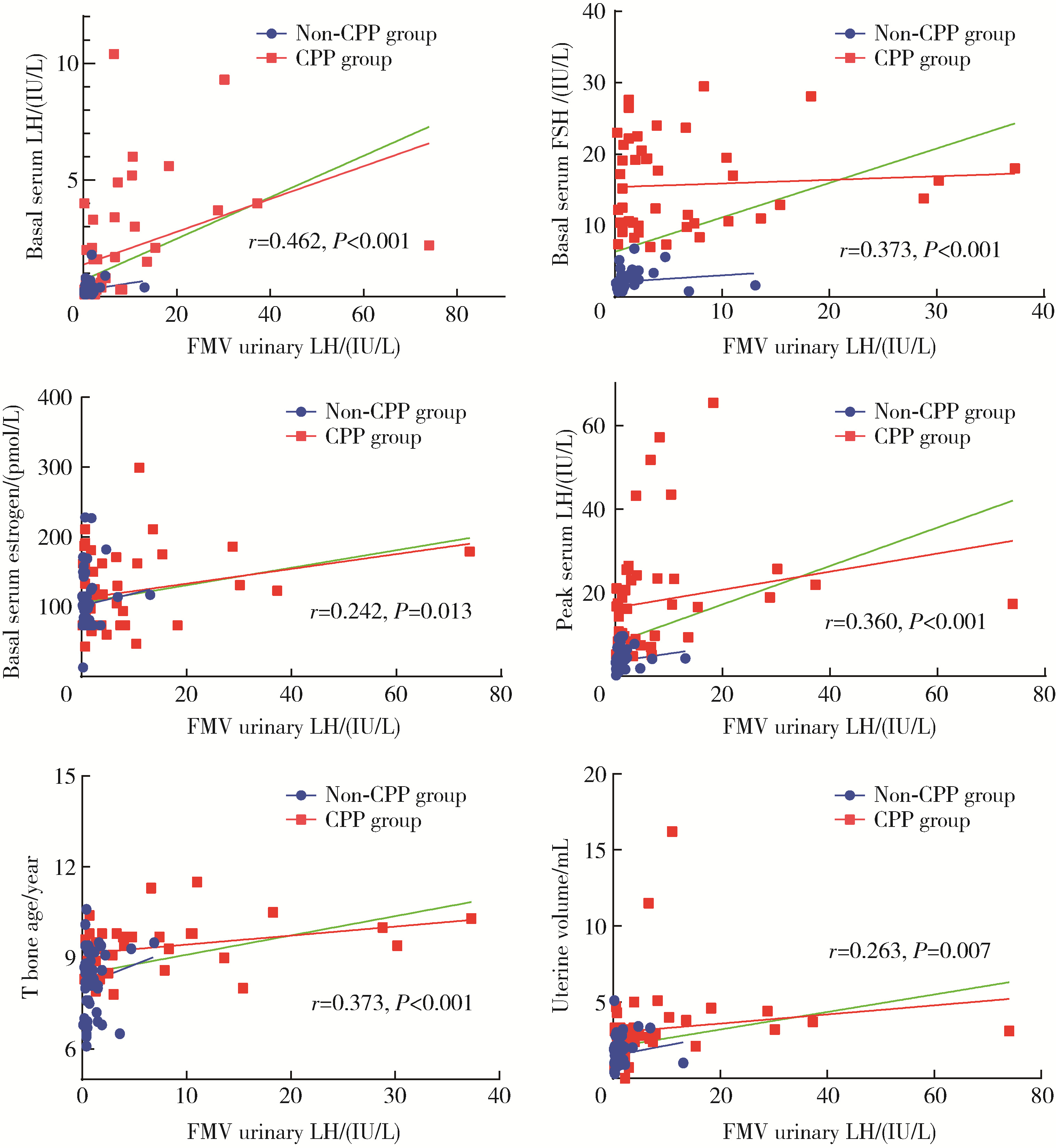
目的: 评估乳房发育女童晨尿促黄体生成素(luteinizing hormone,LH)水平,以确定晨尿LH对于评价中枢性性早熟(central precocious puberty,CPP)的价值。方法: 收集2018年9月至2021年4月期间因性早熟就诊于北京大学第三医院儿科门诊并住院行促性腺激素释放激素(gonadotropin-releasing hormone,GnRH)激发试验的女童共108例,根据CPP诊断标准分为CPP组(n=45)和非CPP组(n=63),比较两组的临床特征及激素水平,采用受试者工作特征(receiver operating characteristic,ROC)曲线分析得出尿LH的临床参考切割值。对尿LH水平与临床常用指标进行相关性分析,进一步评估尿LH在CPP诊断中的价值。结果: ROC曲线分析显示,晨尿LH水平对CPP诊断有意义,切割值为0.69 IU/L时,其敏感度为85%,特异度56.9%,曲线下面积为0.804(P < 0.001)。对GnRH激发试验前的基本临床特征进行二元Logistic回归分析,提示晨尿LH水平、子宫体积、卵巢体积、T骨龄提前程度对于诊断女童CPP均有预测意义(OR值分别为2.125、1.961、1.564、2.672),建立预测模型,ROC曲线下面积为0.904(P<0.001)。进一步行相关性分析,晨尿LH水平与GnRH激发试验前血激素水平(LH、FSH、雌激素)、GnRH激发试验后血LH峰值、T骨龄、子宫体积均呈正相关,r值分别为0.462、0.373、0.242、0.360、0.373和0.263,P值分别为 < 0.001、 < 0.001、0.013、 < 0.001、 < 0.001和0.007。结论: 晨尿LH水平对CPP的诊断有较好的提示意义,同时结合T骨龄提前程度及盆腔超声测量可进一步提高其对女童CPP诊断的预测价值。
中图分类号:
- R725.85
| 1 | 中华医学会儿科学分会内分泌遗传代谢学组, 中华儿科杂志编辑委员会. 中枢性性早熟诊断与治疗专家共识(2022)[J]. 中华儿科杂志, 2023, 61 (1): 16- 22. |
| 2 | Bradley SH , Lawrence N , Steele C , et al. Precocious puberty[J]. BMJ, 2020, 368, l6597. |
| 3 |
Latronico AC , Brito VN , Carel JC . Causes, diagnosis, and treatment of central precocious puberty[J]. Lancet Diabetes Endocrinol, 2016, 4 (3): 265- 274.
doi: 10.1016/S2213-8587(15)00380-0 |
| 4 |
Teilmann G , Pedersen CB , Jensen TK , et al. Prevalence and incidence of precocious pubertal development in Denmark: An epidemiologic study based on national registries[J]. Pediatrics, 2005, 116 (6): 1323- 1328.
doi: 10.1542/peds.2005-0012 |
| 5 | Demir A , Voutilainen R , Juul A , et al. Increase in first morning voided urinary luteinizing hormone levels precedes the physical onset of puberty[J]. J Clin Endocrinol Metab, 1996, 81 (8): 2963- 2967. |
| 6 |
中华医学会儿科学分会内分泌遗传代谢学组, 《中华儿科杂志》编辑委员会. 中枢性性早熟诊断与治疗共识(2015)[J]. 中华儿科杂志, 2015, 53 (6): 412- 418.
doi: 10.3760/cma.j.issn.0578-1310.2015.06.004 |
| 7 | Girard J , Hadziselimovic F . Relevance of urinary gonadotrophins[J]. Eur J Pediatr, 1987, 146 (Suppl 2)): S18- S20. |
| 8 |
Kulin HE , Santner SJ . Timed urinary gonadotropin measurements in normal infants, children, and adults, and in patients with disorders of sexual maturation[J]. J Pediatr, 1977, 90 (5): 760- 765.
doi: 10.1016/S0022-3476(77)81243-2 |
| 9 |
Wood CL , Lane LC , Cheetham T . Puberty: Normal physiology (brief overview)[J]. Best Pract Res Clin Endocrinol Metab, 2019, 33 (3): 101265.
doi: 10.1016/j.beem.2019.03.001 |
| 10 |
Abreu AP , Kaiser UB . Pubertal development and regulation[J]. Lancet Diabetes Endocrinol, 2016, 4 (3): 254- 264.
doi: 10.1016/S2213-8587(15)00418-0 |
| 11 |
Cantas-Orsdemir S , Eugster EA . Update on central precocious puberty: From etiologies to outcomes[J]. Expert Rev Endocrinol Metab, 2019, 14 (2): 123- 130.
doi: 10.1080/17446651.2019.1575726 |
| 12 |
Swerdloff RS , Odell WD . Hormonal mechanisms in the onset of puberty[J]. Postgrad Med J, 1975, 51 (594): 200- 208.
doi: 10.1136/pgmj.51.594.200 |
| 13 |
Apter D , Cacciatore B , Alfthan H , et al. Serum luteinizing hormone concentrations increase 100-fold in females from 7 years to adulthood, as measured by time-resolved immunofluorometric assay[J]. J Clin Endocrinol Metab, 1989, 68 (1): 53- 57.
doi: 10.1210/jcem-68-1-53 |
| 14 |
Rosenfield RL , Bordini B , Yu C . Comparison of detection of normal puberty in girls by a hormonal sleep test and a gonadotropin-releasing hormone agonist test[J]. J Clin Endocrinol Metab, 2013, 98 (4): 1591- 1601.
doi: 10.1210/jc.2012-4136 |
| 15 |
McNeilly JD , Mason A , Khanna S , et al. Urinary gonadotrophins: A useful non-invasive marker of activation of the hypothalamic pituitary-gonadal axis[J]. Int J Pediatr Endocrinol, 2012, 2012 (1): 10.
doi: 10.1186/1687-9856-2012-10 |
| 16 |
Kolby N , Busch AS , Aksglaede L , et al. Nocturnal urinary excretion of FSH and LH in children and adolescents with normal and early puberty[J]. J Clin Endocrinol Metab, 2017, 102 (10): 3830- 3838.
doi: 10.1210/jc.2017-01192 |
| 17 |
Demir A , Voutilainen R , Stenman UH , et al. First morning voided urinary gonadotropin measurements as an alternative to the GnRH test[J]. Horm Res Paediatr, 2016, 85 (5): 301- 308.
doi: 10.1159/000440955 |
| 18 |
Shim YS , An SH , Lee HJ , et al. Random urinary gonadotropins as a useful initial test for girls with central precocious puberty[J]. Endocr J, 2019, 66 (10): 891- 903.
doi: 10.1507/endocrj.EJ19-0071 |
| 19 |
Lee SY , Kim JM , Kim YM , et al. Single random measurement of urinary gonadotropin concentration for screening and monitoring of girls with central precocious puberty[J]. Ann Pediatr Endocrinol Metab, 2021, 26 (3): 178- 184.
doi: 10.6065/apem.2040208.104 |
| 20 |
Zung A , Burundukov E , Ulman M , et al. The diagnostic value of first-voided urinary LH compared with GnRH-stimulated gonadotropins in differentiating slowly progressive from rapidly progressive precocious puberty in girls[J]. Eur J Endocrinol, 2014, 170 (5): 749- 758.
doi: 10.1530/EJE-14-0010 |
| 21 |
Soriano-Guillen L , Argente J . Central precocious puberty, functional and tumor-related[J]. Best Pract Res Clin Endocrinol Metab, 2019, 33 (3): 101262.
doi: 10.1016/j.beem.2019.01.003 |
| 22 |
Xu YQ , Li GM , Li Y . Advanced bone age as an indicator facilitates the diagnosis of precocious puberty[J]. J Pediatr (Rio J), 2018, 94 (1): 69- 75.
doi: 10.1016/j.jped.2017.03.010 |
| 23 |
de Vries L , Horev G , Schwartz M , et al. Ultrasonographic and clinical parameters for early differentiation between precocious puberty and premature thelarche[J]. Eur J Endocrinol, 2006, 154 (6): 891- 898.
doi: 10.1530/eje.1.02151 |
| 24 |
Eksioglu AS , Yilmaz S , Cetinkaya S , et al. Value of pelvic sono-graphy in the diagnosis of various forms of precocious puberty in girls[J]. J Clin Ultrasound, 2013, 41 (2): 84- 93.
doi: 10.1002/jcu.22004 |
| 25 |
Lee SH , Joo EY , Lee JE , et al. The diagnostic value of pelvic ultrasound in girls with central precocious puberty[J]. Chonnam Med J, 2016, 52 (1): 70- 74.
doi: 10.4068/cmj.2016.52.1.70 |
| 26 |
Yuan B , Pi YL , Zhang YN , et al. A diagnostic model of idiopa-thic central precocious puberty based on transrectal pelvic ultrasound and basal gonadotropin levels[J]. J Int Med Res, 2020, 48 (8): 300060520935278.
doi: 10.1177/0300060520935278 |
| 27 |
Yu HK , Liu X , Chen JK , et al. Pelvic ultrasound in diagnosing and evaluating the efficacy of gonadotropin-releasing hormone agonist therapy in girls with idiopathic central precocious puberty[J]. Front Pharmacol, 2019, 10, 104.
doi: 10.3389/fphar.2019.00104 |
| [1] | 王杰, 王建伟, 夏海缀, 徐啸, 翟建坡, 何峰, 黄广林, 李贵忠. 阴茎远端尿道狭窄疾病的手术治疗方式[J]. 北京大学学报(医学版), 2024, 56(6): 1075-1082. |
| [2] | 毛雅晴, 陈震, 于尧, 章文博, 刘洋, 彭歆. 2型糖尿病对口腔鳞状细胞癌患者预后的影响[J]. 北京大学学报(医学版), 2024, 56(6): 1089-1096. |
| [3] | 柯涵炜, 王起, 许克新. 优化环磷酰胺剂量在间质性膀胱炎/膀胱疼痛综合征啮齿动物模型中的应用[J]. 北京大学学报(医学版), 2024, 56(5): 908-912. |
| [4] | 陈思鹭, 王海菊, 吴宇财, 李志华, 黄燕波, 何宇辉, 许洋洋, 李学松, 贯华. 成人肾积水病因分析:一项单中心横断面研究[J]. 北京大学学报(医学版), 2024, 56(5): 913-918. |
| [5] | 王明瑞, 王起, 胡浩, 赖金惠, 唐鑫伟, 万春艳, 许克新, 徐涛. 覆膜金属输尿管支架治疗盆腔脂肪增多症所致肾积水的疗效[J]. 北京大学学报(医学版), 2024, 56(5): 919-922. |
| [6] | 张培恒, 高莹, 吴红花, 张健, 张俊清. 暴发性1型糖尿病合并急性胰腺炎1例及文献回顾[J]. 北京大学学报(医学版), 2024, 56(5): 923-927. |
| [7] | 于书慧,韩佳凝,钟丽君,陈聪语,肖云翔,黄燕波,杨洋,车新艳. 术前盆底肌电生理参数对前列腺癌根治性切除术后早期尿失禁的预测价值[J]. 北京大学学报(医学版), 2024, 56(4): 594-599. |
| [8] | 李雨清,王飚,乔鹏,王玮,关星. 经耻骨后尿道中段悬吊带术治疗女性复发性压力性尿失禁的中长期疗效[J]. 北京大学学报(医学版), 2024, 56(4): 600-604. |
| [9] | 王明瑞,刘军,熊六林,于路平,胡浩,许克新,徐涛. 经皮微通道-微电子肾镜-微超声探针碎石术治疗1.5~2.5 cm肾结石的疗效和安全性[J]. 北京大学学报(医学版), 2024, 56(4): 605-609. |
| [10] | 应沂岑,杜毅聪,李志华,张一鸣,李新飞,王冰,张鹏,朱宏建,周利群,杨昆霖,李学松. 机器人辅助腹腔镜下颊黏膜补片输尿管成形术治疗复杂输尿管狭窄[J]. 北京大学学报(医学版), 2024, 56(4): 640-645. |
| [11] | 杨文博,余磊,张维宇,徐涛,王强. 带线输尿管支架自排技术在肾移植受者中的效果及安全性[J]. 北京大学学报(医学版), 2024, 56(4): 656-660. |
| [12] | 周庆欣,杨晴晴,石舒原,李沛,孙凤. 健康体检人群血尿酸与气流阻塞的相关性[J]. 北京大学学报(医学版), 2024, 56(4): 693-699. |
| [13] | 马雨佳,卢燃藜,周泽宸,李晓怡,闫泽玉,武轶群,陈大方. 基于两样本孟德尔随机化的失眠与2型糖尿病关联研究[J]. 北京大学学报(医学版), 2024, 56(1): 174-178. |
| [14] | 许克新,丁泽华. 人工智能在功能泌尿外科的应用[J]. 北京大学学报(医学版), 2023, 55(5): 771-774. |
| [15] | 毛海,张帆,张展奕,颜野,郝一昌,黄毅,马潞林,褚红玲,张树栋. 基于MRI前列腺腺体相关参数构建腹腔镜前列腺癌术后尿失禁的预测模型[J]. 北京大学学报(医学版), 2023, 55(5): 818-824. |
|
||