Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (2): 249-254. doi: 10.19723/j.issn.1671-167X.2022.02.008
Previous Articles Next Articles
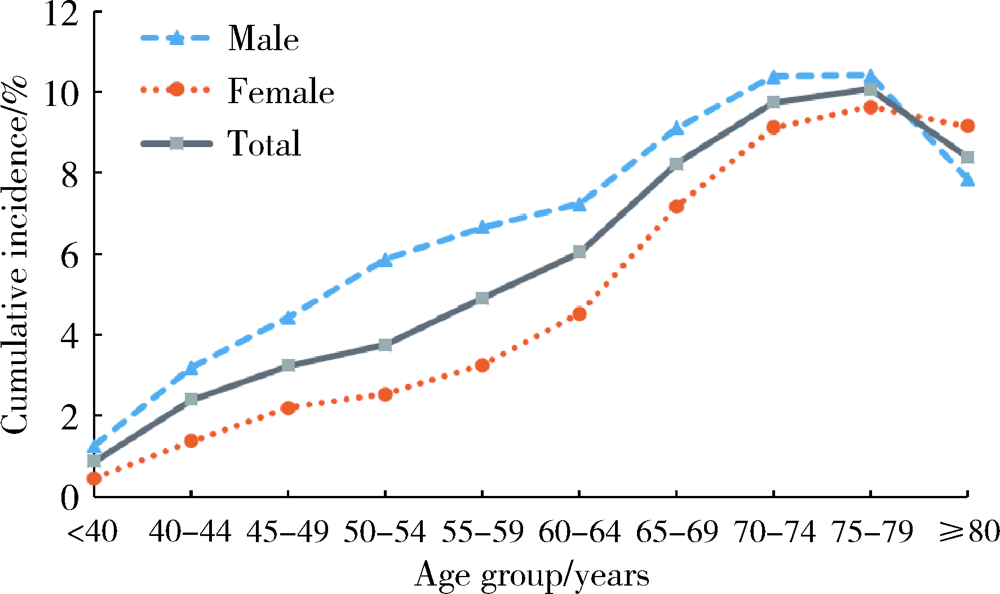
Incidence and risk factors of ischemic stroke in patients with type 2 diabetes among urban workers in Beijing, China
WU Jun-hui,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,QIN Xue-ying,WANG Meng-ying,WANG Xiao-wen,WANG Jia-ting,HU Yong-hua( )
)
- Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
CLC Number:
- R181.32
| [1] |
Cho NH, Shaw JE, Karuranga S, et al. IDF diabetes atlas: Glo-bal estimates of diabetes prevalence for 2017 and projections for 2045[J]. Diabetes Res Clin Pract, 2018, 138:271-281.
doi: 10.1016/j.diabres.2018.02.023 |
| [2] |
Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: A systema-tic analysis for the global burden of disease study 2013[J]. Lancet Neurol, 2016, 15(9):913-924.
doi: 10.1016/S1474-4422(16)30073-4 |
| [3] |
Yang R, Pedersen NL, Bao C, et al. Type 2 diabetes in midlife and risk of cerebrovascular disease in late life: A prospective nested case-control study in a nationwide Swedish twin cohort[J]. Diabetologia, 2019, 62(8):1403-1411.
doi: 10.1007/s00125-019-4892-3 |
| [4] |
Kissela BM, Khoury J, Kleindorfer D, et al. Epidemiology of ischemic stroke in patients with diabetes: The greater Cincinnati/Northern Kentucky stroke study[J]. Diabetes Care, 2005, 28(2):355-359.
doi: 10.2337/diacare.28.2.355 pmid: 15677792 |
| [5] |
Huang ES, Laiteerapong N, Liu JY, et al. Rates of complications and mortality in older patients with diabetes mellitus: The diabetes and aging study[J]. JAMA Intern Med, 2014, 174(2):251-258.
doi: 10.1001/jamainternmed.2013.12956 |
| [6] |
Staszewsky L, Cortesi L, Baviera M, et al. Diabetes mellitus as risk factor for atrial fibrillation hospitalization: Incidence and outcomes over nine years in a region of Northern Italy[J]. Diabetes Res Clin Pract, 2015, 109(3):476-484.
doi: 10.1016/j.diabres.2015.06.006 |
| [7] |
Li J, Dong Y, Wu T, et al. Differences between Western and Asian type 2 diabetes patients in the incidence of vascular complications and mortality: A systematic review of randomized controlled trials on lowering blood glucose[J]. J Diabetes, 2016, 8(6):824-833.
doi: 10.1111/1753-0407.12361 |
| [8] |
Mulnier HE, Seaman HE, Raleigh VS, et al. Risk of stroke in people with type 2 diabetes in the UK: A study using the general practice research database[J]. Diabetologia, 2006, 49(12):2859-2865.
pmid: 17072582 |
| [9] |
Giorda CB, Avogaro A, Maggini M, et al. Incidence and risk factors for stroke in type 2 diabetic patients: The DAI study[J]. Stroke, 2007, 38(4):1154-1160.
pmid: 17332448 |
| [10] |
Gong Q, Zhang P, Wang J, et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing diabetes prevention outcome study[J]. Lancet Diabetes Endocrinol, 2019, 7(6):452-461.
doi: 10.1016/S2213-8587(19)30093-2 |
| [11] |
Banerjee C, Moon YP, Paik MC, et al. Duration of diabetes and risk of ischemic stroke: The Northern Manhattan study[J]. Stroke, 2012, 43(5):1212-1217.
doi: 10.1161/STROKEAHA.111.641381 |
| [12] | 任晓宇, 史典, 张德生, 等. 金昌队列人群代谢性疾病与脑卒中发病关系前瞻性研究[J]. 中华流行病学杂志, 2019, 40(5):521-525. |
| [13] | 沈卓之, 丁贤彬, 毛德强, 等. 2015年重庆市常住人口脑卒中发病与死亡情况[J]. 公共卫生与预防医学, 2016, 27(5):48-51. |
| [14] | 韩荣荣, 唐爱奇, 方杭燕, 等. 2型糖尿病患者并发脑卒中的前瞻性研究[J]. 预防医学, 2017, 29(2):139-141. |
| [15] |
Luk AOY, Hui EMT, Sin MC, et al. Declining trends of cardiovascular-renal complications and mortality in type 2 diabetes: The Hong Kong diabetes database[J]. Diabetes Care, 2017, 40(7):928-935.
doi: 10.2337/dc16-2354 |
| [16] |
Shen Y, Shi L, Nauman E, et al. Race and sex differences in rates of diabetic complications[J]. J Diabetes, 2019, 11(6):449-456.
doi: 10.1111/1753-0407.12869 pmid: 30315628 |
| [17] |
Wang Y, Dai Y, Zheng J, et al. Sex difference in the incidence of stroke and its corresponding influence factors: Results from a follow-up 8.4 years of rural China hypertensive prospective cohort study[J]. Lipids Health Dis, 2019, 18(1):72.
doi: 10.1186/s12944-019-1010-y |
| [18] |
Barker-Collo S, Bennett DA, Krishnamurthi RV, et al. Sex diffe-rences in stroke incidence, prevalence, mortality and disability-adjusted life years: Results from the global burden of disease study 2013[J]. Neuroepidemiology, 2015, 45(3):203-214.
doi: 10.1159/000441103 pmid: 26505984 |
| [19] |
Madsen TE, Khoury JC, Alwell KA, et al. Sex differences in cardiovascular risk profiles of ischemic stroke patients with diabetes in the Greater Cincinnati/Northern Kentucky stroke study[J]. J Diabetes, 2018, 10(6):496-501.
doi: 10.1111/1753-0407.12567 pmid: 28523847 |
| [20] |
Petrea RE, Beiser AS, Seshadri S, et al. Gender differences in stroke incidence and poststroke disability in the Framingham heart study[J]. Stroke, 2009, 40(4):1032-1037.
doi: 10.1161/STROKEAHA.108.542894 |
| [21] | 申宏, 方旭东. 重庆市巴南区居民2012—2015年脑卒中发病情况分析[J]. 检验医学与临床, 2016, 13(23):3398-3399. |
| [22] | 叶虹. 2型糖尿病合并缺血性脑血管病的相关危险因素研究[D]. 广州: 南方医科大学, 2011. |
| [23] |
GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: A systematic analysis for the glo-bal burden of disease study 2016[J]. Lancet Neurol, 2019, 18(5):439-458.
doi: 10.1016/S1474-4422(19)30034-1 |
| [24] | Madan S. Changes in diabetes-related complications in the United States[J]. N Engl J Med, 2014, 371(3):285-286. |
| [25] |
Bui HDT, Jing X, Lu R, et al. Prevalence of and factors related to microvascular complications in patients with type 2 diabetes mellitus in Tianjin, China: A cross-sectional study[J]. Ann Transl Med, 2019, 7(14):325.
doi: 10.21037/atm |
| [1] | Peiheng ZHANG, Ying GAO, Honghua WU, Jian ZHANG, Junqing ZHANG. Fulminant type 1 diabetes mellitus with acute pancreatitis: A case report and literature review [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 923-927. |
| [2] | Yujia MA,Ranli LU,Zechen ZHOU,Xiaoyi LI,Zeyu YAN,Yiqun WU,Dafang CHEN. Association between insomnia and type 2 diabetes: A two-sample Mendelian rando-mization study [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 174-178. |
| [3] | Lei BAO,Xia-xia CAI,Ming-yuan ZHANG,Lei-lei REN. Effect of vitamin D3 on mild cognitive impairment in type 2 diabetic mice and its possible mechanism [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 587-592. |
| [4] | Xiao-yue ZHANG,Yu-xin LIN,Ying JIANG,Lan-chao ZHANG,Mang-yan DONG,Hai-yi CHI,Hao-yu DONG,Li-jun MA,Zhi-jing LI,Chun CHANG. Mediating effect of self-efficacy on self-management ability and self-management behavior in patients with type 2 diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 450-455. |
| [5] | Huan YU,Ruo-tong YANG,Si-yue WANG,Jun-hui WU,Meng-ying WANG,Xue-ying QIN,Tao WU,Da-fang CHEN,Yi-qun WU,Yong-hua HU. Metformin use and risk of ischemic stroke in patients with type 2 diabetes: A cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 456-464. |
| [6] | Ruo-tong YANG,Meng-ying WANG,Chun-nan LI,Huan YU,Xiao-wen WANG,Jun-hui WU,Si-yue WANG,Jia-ting WANG,Da-fang CHEN,Tao WU,Yong-hua HU. Interaction between ischemic stroke risk loci identified by genome-wide association studies and sleep habits [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 412-420. |
| [7] | Yu-han DENG,Yong JIANG,Zi-yao WANG,Shuang LIU,Yu-xin WANG,Bao-hua LIU. Long short-term memory and Logistic regression for mortality risk prediction of intensive care unit patients with stroke [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 458-467. |
| [8] | Bing-jie HE,Zhi-ke LIU,Peng SHEN,Ye-xiang SUN,Bin CHEN,Si-yan ZHAN,Hong-bo LIN. Epidemiological study on the incidence of inflammatory bowel disease in Yinzhou District, Ningbo City from 2011 to 2020 [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 511-519. |
| [9] | XU Xin-ran,HUO Peng-cheng,HE Lu,MENG Huan-xin,ZHU Yun-xuan,JIN Dong-si-qi. Comparison of initial periodontal therapy and its correlation with white blood cell level in periodontitis patients with or without diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 48-53. |
| [10] | REN Guo-yong,WU Xue-mei, ,LI Jie-yu,SUN Wei-ping,HUANG Yi-ning. Susceptibility vessel sign in subacute stroke patients with large vessel occlusion [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1133-1138. |
| [11] | Ya-fei LIU,Lin-lin SONG,Mao-wei XING,Li-xin CAI,Dong-xin WANG. Comparison of pulse pressure variation, stroke volume variation, and plethysmographic variability index in pediatric patients undergoing craniotomy [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 946-951. |
| [12] | GUO Hong-ping,ZHAO Ai,XUE Yong,MA Liang-kun,ZHANG Yu-mei,WANG Pei-yu. Relationship between nutrients intake during pregnancy and the glycemic control effect in pregnant women with gestational diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 467-472. |
| [13] | YAO Xiao-ying,LIU Zhi-ke,LI Ning,MA Rui,ZHAO Xue-fei,ZHANG Liang,XU Guo-zhang,ZHAN Si-yan,FANG Ting. Epidemiological study of infantile epilepsy incidence density among infants under 36 months of age in Ningbo City from 2015 to 2019 [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 485-490. |
| [14] | WU Jun-hui,CHEN Hong-bo,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,WANG Meng-ying,WANG Si-yue,WANG Xiao-wen,WANG Jia-ting,YU Huan,HU Yong-hua. Prevalence and risk factors of osteoarthritis in patients with type 2 diabetes in Beijing, China from 2015 to 2017 [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 518-522. |
| [15] | FAN Li-shi,GAO Min,Edwin B. FISHER,SUN Xin-ying. Factors associated with quality of life in 747 patients with type 2 diabetes in Tongzhou District and Shunyi District of Beijing [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 523-529. |
|
||