Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (4): 661-666. doi: 10.19723/j.issn.1671-167X.2024.04.019
Previous Articles Next Articles
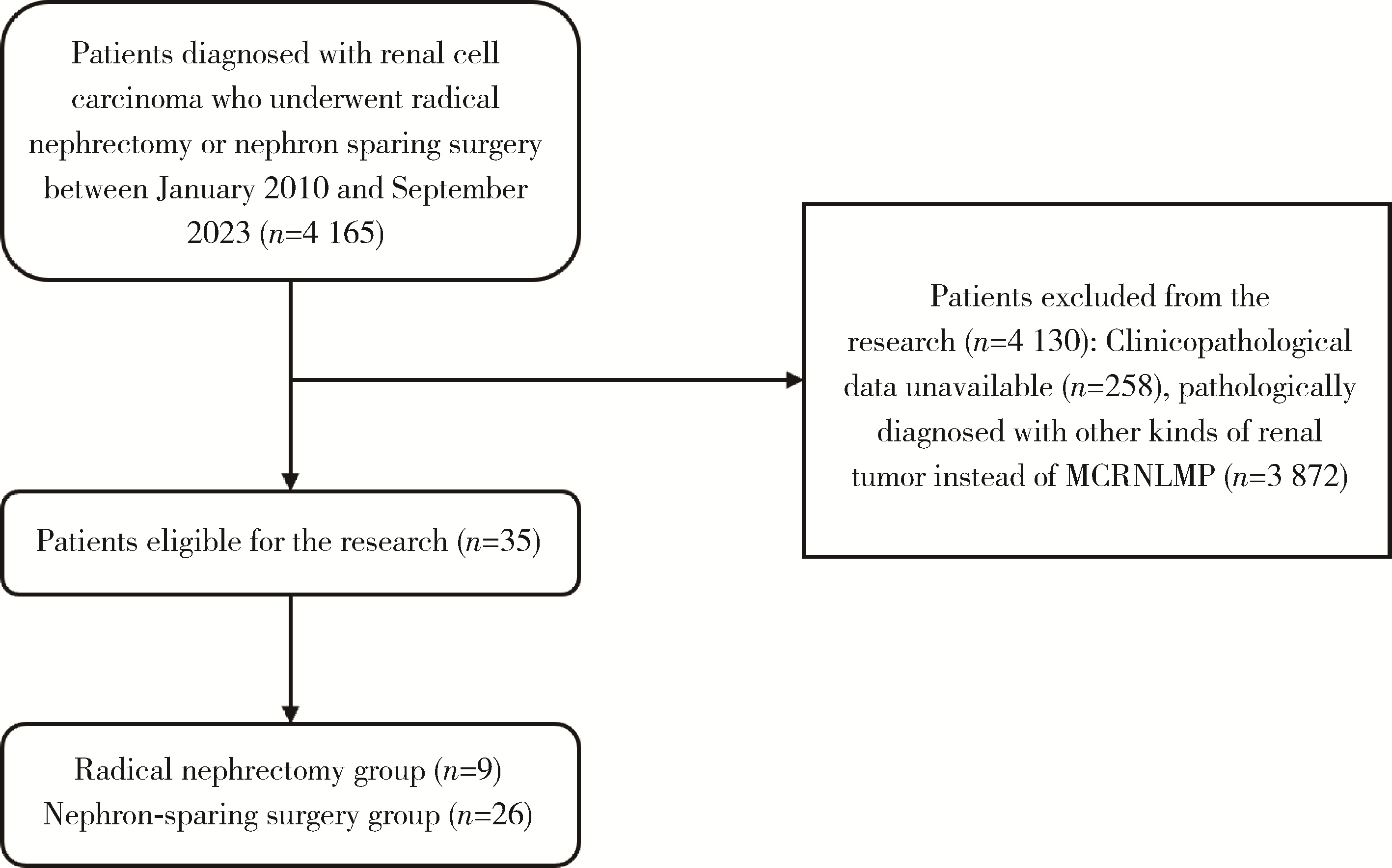
Clinicopathological characteristics and prognosis of multilocular cystic renal neoplasm of low malignant potential
Le YU,Shaohui DENG,Fan ZHANG,Ye YAN,Jianfei YE,Shudong ZHANG*( )
)
- Department of Urology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.1
| 1 |
Siegel RL , Miller KD , Fuchs HE , et al. Cancer statistics, 2022[J]. CA Cancer J Clin, 2022, 72 (1): 7- 33.
doi: 10.3322/caac.21708 |
| 2 |
Moch H , Cubilla AL , Humphrey PA , et al. The 2016 WHO classification of tumours of the urinary system and male genital organs. Part A: Renal, penile, and testicular tumours[J]. Eur Urol, 2016, 70 (1): 93- 105.
doi: 10.1016/j.eururo.2016.02.029 |
| 3 |
Li T , Chen J , Jiang Y , et al. Multilocular cystic renal cell neoplasm of low malignant potential: A series of 76 cases[J]. Clin Genitourin Cancer, 2016, 14 (6): e553- e557.
doi: 10.1016/j.clgc.2016.03.017 |
| 4 |
Westerman ME , Cheville JC , Lohse CM , et al. Long-term outcomes of patients with low grade cystic renal epithelial neoplasms[J]. Urology, 2019, 133, 145- 150.
doi: 10.1016/j.urology.2019.07.017 |
| 5 |
Suzigan S , López-Beltrán A , Montironi R , et al. Multilocular cystic renal cell carcinoma: A report of 45 cases of a kidney tumor of low malignant potential[J]. Am J Clin Pathol, 2006, 125 (2): 217- 222.
doi: 10.1309/AH6FC77PYR2V6YAY |
| 6 |
Kashan M , Ghanaat M , Hötker AM , et al. Cystic renal cell carcinoma: A report on outcomes of surgery and active surveillance in patients retrospectively identified on pretreatment imaging[J]. J Urol, 2018, 200 (2): 275- 282.
doi: 10.1016/j.juro.2018.02.3087 |
| 7 |
Silverman SG , Pedrosa I , Ellis JH , et al. Bosniak classification of cystic renal masses, version 2019: An update proposal and needs assessment[J]. Radiology, 2019, 292 (2): 475- 488.
doi: 10.1148/radiol.2019182646 |
| 8 |
Alrumayyan M , Raveendran L , Lawson KA , et al. Cystic renal masses: Old and new paradigms[J]. Urol Clin North Am, 2023, 50 (2): 227- 238.
doi: 10.1016/j.ucl.2023.01.003 |
| 9 |
Yang B , Sun L , Cao WF , et al. Clear cell renal cell carcinoma with cystic component similar to multilocular cystic renal neoplasm of low malignant potential: A rare pattern of cyst-dependent progression from multilocular cystic renal neoplasm of low malignant potential[J]. Diagn Pathol, 2023, 18 (1): 27.
doi: 10.1186/s13000-023-01315-x |
| 10 |
Pini GM , Lucianò R , Colecchia M . Cystic clear cell renal cell carcinoma: A morphological and molecular reappraisal[J]. Can-cers (Basel), 2023, 15 (13): 3352.
doi: 10.3390/cancers15133352 |
| 11 |
Kim SH , Park WS , Chung J . SETD2, GIGYF2, FGFR3, BCR, KMT2C, and TSC2 as candidate genes for differentiating multi-locular cystic renal neoplasm of low malignant potential from clear cell renal cell carcinoma with cystic change[J]. Investig Clin Urol, 2019, 60 (3): 148- 155.
doi: 10.4111/icu.2019.60.3.148 |
| 12 |
Raspollini MR , Castiglione F , Martignoni G , et al. Unlike in clear cell renal cell carcinoma, KRAS is not mutated in multilocular cystic clear cell renal cell neoplasm of low potential[J]. Virchows Arch, 2015, 467 (6): 687- 693.
doi: 10.1007/s00428-015-1859-8 |
| 13 |
Shan K , Fu A , Liu N , et al. Contrast-enhanced ultrasound (CEUS) vs contrast-enhanced computed tomography for multilocular cystic renal neoplasm of low malignant potential: A retrospective analysis for diagnostic performance study[J]. Medicine (Baltimore), 2020, 99 (46): e23110.
doi: 10.1097/MD.0000000000023110 |
| 14 |
Bhatt JR , Jewett MA , Richard PO , et al. Multilocular cystic renal cell carcinoma: Pathological T staging makes no difference to favorable outcomes and should be reclassified[J]. J Urol, 2016, 196 (5): 1350- 1355.
doi: 10.1016/j.juro.2016.05.118 |
| 15 |
Nassir A , Jollimore J , Gupta R , et al. Multilocular cystic renal cell carcinoma: A series of 12 cases and review of the literature[J]. Urology, 2002, 60 (3): 421- 427.
doi: 10.1016/S0090-4295(02)01742-9 |
| 16 |
Gong K , Zhang N , He Z , et al. Multilocular cystic renal cell carcinoma: An experience of clinical management for 31 cases[J]. J Cancer Res Clin Oncol, 2008, 134 (4): 433- 437.
doi: 10.1007/s00432-007-0302-1 |
| 17 |
Pitra T , Pivovarcikova K , Alaghehbandan R , et al. A comprehensive commentary on the multilocular cystic renal neoplasm of low malignant potential: A urologist' s perspective[J]. Cancers (Basel), 2022, 14 (3): 831.
doi: 10.3390/cancers14030831 |
| 18 |
Cao C , Deng S , Wang B , et al. Intraoperative near-infrared Ⅱ window fluorescence imaging-assisted nephron-sparing surgery for complete resection of cystic renal masses[J]. Clin Transl Med, 2021, 11 (10): e604.
doi: 10.1002/ctm2.604 |
| [1] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [2] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [3] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [4] | Yangyi FANG,Qiang LI,Zhigao HUANG,Min LU,Kai HONG,Shudong ZHANG. Well-differentiated papillary mesothelial tumour of the tunica vaginalis: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 741-744. |
| [5] | Yuanyuan ZENG,Yun XIE,Daonan CHEN,Ruilan WANG. Related factors of euthyroid sick syndrome in patients with sepsis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 526-532. |
| [6] | Kewei CHEN,Shaohui DENG,Zhuo LIU,Hongxian ZHANG,Lulin MA,Shudong ZHANG. Discussion on the surgical timing of rupture and hemorrhage of renal angiomyolipoma [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 326-331. |
| [7] | Jian-bin LI,Meng-na LYU,Qiang CHI,Yi-lin PENG,Peng-cheng LIU,Rui WU. Early prediction of severe COVID-19 in patients with Sjögren’s syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1007-1012. |
| [8] | Huan-rui LIU,Xiang PENG,Sen-lin LI,Xin GOU. Risk modeling based on HER-2 related genes for bladder cancer survival prognosis assessment [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 793-801. |
| [9] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [10] | Han LU,Jian-yun ZHANG,Rong YANG,Le XU,Qing-xiang LI,Yu-xing GUO,Chuan-bin GUO. Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 702-707. |
| [11] | Yun-fei SHI,Hao-jie WANG,Wei-ping LIU,Lan MI,Meng-ping LONG,Yan-fei LIU,Yu-mei LAI,Li-xin ZHOU,Xin-ting DIAO,Xiang-hong LI. Analysis of clinicopathological and molecular abnormalities of angioimmunoblastic T-cell lymphoma [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 521-529. |
| [12] | Xiao-juan ZHU,Hong ZHANG,Shuang ZHANG,Dong LI,Xin LI,Ling XU,Ting LI. Clinicopathological features and prognosis of breast cancer with human epidermal growth factor receptor 2 low expression [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 243-253. |
| [13] | Yu-mei LAI,Zhong-wu LI,Huan LI,Yan WU,Yun-fei SHI,Li-xin ZHOU,Yu-tong LOU,Chuan-liang CUI. Clinicopathological features and prognosis of anorectal melanoma: A report of 68 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 262-269. |
| [14] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
| [15] | Qian SU,Xin PENG,Chuan-xiang ZHOU,Guang-yan YU. Clinicopathological characteristics and prognosis of non-Hodgkin lymphoma in oral and maxillofacial regions: An analysis of 369 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 13-21. |
|
||