Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (4): 624-630. doi: 10.19723/j.issn.1671-167X.2024.04.013
Previous Articles Next Articles
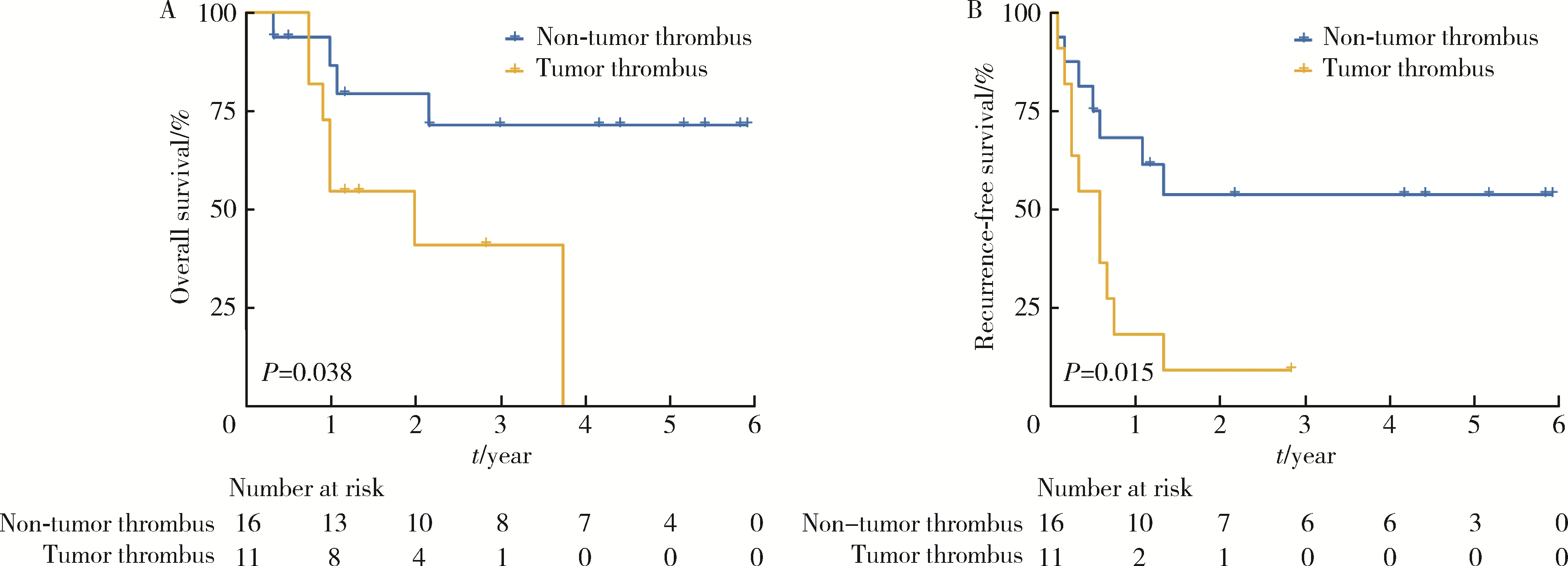
Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus
Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG*( )
)
- Department of Urology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R699.3
| 1 |
Calissendorff J , Calissendorff F , Falhammar H . Adrenocortical cancer: Mortality, hormone secretion, proliferation and urine ste-roids: Experience from a single centre spanning three decades[J]. BMC Endocr Disord, 2016, 16, 15.
doi: 10.1186/s12902-016-0095-9 |
| 2 |
De Filpo G , Mannelli M , Canu L . Adrenocortical carcinoma: Current treatment options[J]. Curr Opin Oncol, 2021, 33 (1): 16- 22.
doi: 10.1097/CCO.0000000000000695 |
| 3 |
Brönimann S , Garstka N , Remzi M . Treatment of adrenocortical carcinoma: Oncological and endocrine outcomes[J]. Curr Opin Urol, 2023, 33 (1): 50- 58.
doi: 10.1097/MOU.0000000000001045 |
| 4 |
Xu WH , Wu J , Wang J , et al. Screening and identification of potential prognostic biomarkers in adrenocortical carcinoma[J]. Front Genet, 2019, 10, 821.
doi: 10.3389/fgene.2019.00821 |
| 5 | 邓建华, 李汉忠, 纪志刚, 等. 肾上腺皮质癌的综合治疗[J]. 北京大学学报(医学版), 2019, 51 (2): 298- 301. |
| 6 |
Quinones-Baldrich W , Alktaifi A , Eilber F , et al. Inferior vena cava resection and reconstruction for retroperitoneal tumor excision[J]. J Vasc Surg, 2012, 55 (5): 1386- 1393.
doi: 10.1016/j.jvs.2011.11.054 |
| 7 |
Schwarzbach MH , Hormann Y , Hinz U , et al. Clinical results of surgery for retroperitoneal sarcoma with major blood vessel involvement[J]. J Vasc Surg, 2006, 44 (1): 46- 55.
doi: 10.1016/j.jvs.2006.03.001 |
| 8 |
Nooromid MJ , Ju MH , Havelka GE , et al. Fifteen-year expe-rience with renal cell carcinoma with associated venous tumor thrombus[J]. Surgery, 2016, 160 (4): 915- 923.
doi: 10.1016/j.surg.2016.06.029 |
| 9 |
Shao P , Li J , Qin C , et al. Laparoscopic radical nephrectomy and inferior vena cava thrombectomy in the treatment of renal cell carcinoma[J]. Eur Urol, 2015, 68 (1): 115- 122.
doi: 10.1016/j.eururo.2014.12.011 |
| 10 |
Agochukwu N , Shuch B . Clinical management of renal cell carcinoma with venous tumor thrombus[J]. World J Urol, 2014, 32 (3): 581- 589.
doi: 10.1007/s00345-014-1276-7 |
| 11 |
Fairweather M , Raut CP . Nephrectomy for retroperitoneal sarcoma: Stay calm and (cautiously) carry on[J]. Ann Surg Oncol, 2021, 28 (3): 1275- 1277.
doi: 10.1245/s10434-020-09293-w |
| 12 |
Liu Z , Ge L , Liu L , et al. Clinical experience and management strategy of retroperitoneal tumor with venous tumor thrombus involvement[J]. Front Oncol, 2022, 12, 873729.
doi: 10.3389/fonc.2022.873729 |
| 13 | Jannello LMI, Incesu RB, Morra S, et al. The European Network for the Study of Adrenal Tumors staging system (2015): A United States validation[J/OL]. J Clin Endocrinol Metab, 2024: dgae047[2024-02-18]. doi: 10.1210/clinem/dgae047. |
| 14 |
Liu Z , Zhao X , Ge L , et al. Completely laparoscopic versus open radical nephrectomy and infrahepatic tumor thrombectomy: Comparison of surgical complexity and prognosis[J]. Asian J Surg, 2021, 44 (4): 641- 648.
doi: 10.1016/j.asjsur.2020.12.003 |
| 15 |
Zhang G , Li X , Sun G , et al. Clinical analysis of Kimura's di-sease in 24 cases from China[J]. BMC Surg, 2020, 20 (1): 1.
doi: 10.1186/s12893-019-0673-7 |
| 16 |
Liu Z , Li Y , Zhang Y , et al. PUTH grading system for urinary tumor with supradiaphragmatic tumor thrombus: Different surgical techniques for different tumor characteristics[J]. Front Oncol, 2022, 11, 735145.
doi: 10.3389/fonc.2021.735145 |
| 17 |
Blute ML , Leibovich BC , Lohse CM , et al. The Mayo clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus[J]. BJU Int, 2004, 94 (1): 33- 41.
doi: 10.1111/j.1464-410X.2004.04897.x |
| 18 |
Laan DV , Thiels CA , Glasgow A , et al. Adrenocortical carcinoma with inferior vena cava tumor thrombus[J]. Surgery, 2017, 161 (1): 240- 248.
doi: 10.1016/j.surg.2016.07.040 |
| 19 |
Piardi T , Lhuaire M , Memeo R , et al. Laparoscopic Pringle maneuver: How we do it?[J]. Hepatobiliary Surg Nutr, 2016, 5 (4): 345- 349.
doi: 10.21037/hbsn.2015.11.01 |
| 20 |
Fiore M , Colombo C , Locati P , et al. Surgical technique, morbi-dity, and outcome of primary retroperitoneal sarcoma involving inferior vena cava[J]. Ann Surg Oncol, 2012, 19 (2): 511- 518.
doi: 10.1245/s10434-011-1954-2 |
| 21 | 刘磊, 王国良, 马潞林, 等. 肾上腺区巨大肿瘤合并瘤栓的诊断与治疗[J]. 北京大学学报(医学版), 2019, 51 (4): 684- 688. |
| 22 |
杨华安, 郭胜杰. 肾上腺皮质癌合并静脉癌栓的手术治疗及预后[J]. 实用医学杂志, 2020, 36 (10): 1344- 1348.
doi: 10.3969/j.issn.1006-5725.2020.10.015 |
| 23 |
Zhao X , Liu Z , Zhang H , et al. PKUTHLP score: A comprehensive system to predict surgical approach in radical nephrectomy and thrombectomy[J]. Oncol Lett, 2020, 20 (1): 201- 208.
doi: 10.3892/ol.2020.11571 |
| 24 | Vuong NS , Ferriere JM , Michiels C , et al. Robot-assisted versus open surgery for radical nephrectomy with level 1-2 vena cava tumor thrombectomy: A French monocenter experience (UroCCR study #73)[J]. Minerva Urol Nephrol, 2021, 73 (4): 498- 508. |
| 25 |
Treiger BF , Humphrey LS , Peterson CV , et al. Transesophageal echocardiography in renal cell carcinoma: An accurate diagnostic technique for intracaval neoplastic extension[J]. J Urol, 1991, 145 (6): 1138- 1140.
doi: 10.1016/S0022-5347(17)38556-7 |
| [1] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [2] | Kewei CHEN,Zhuo LIU,Shaohui DENG,Fan ZHANG,Jianfei YE,Guoliang WANG,Shudong ZHANG. Clinical diagnosis and treatment of renal angiomyolipoma with inferior vena cava tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 617-623. |
| [3] | Jie YANG,Jieli FENG,Shudong ZHANG,Lulin MA,Qing ZHENG. Clinical effects of transesophageal echocardiography in different surgical methods for nephrectomy combined with Mayo Ⅲ-Ⅳ vena tumor thrombectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 631-635. |
| [4] | Binshuai WANG,Min QIU,Qianjin ZHANG,Maofeng TIAN,Lei LIU,Guoliang WANG,Min LU,Xiaojun TIAN,Shudong ZHANG. Experience in diagnosis and treatment of 6 cases of renal Ewing's sarcoma with venous thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 636-639. |
| [5] | Le YU,Shaohui DENG,Fan ZHANG,Ye YAN,Jianfei YE,Shudong ZHANG. Clinicopathological characteristics and prognosis of multilocular cystic renal neoplasm of low malignant potential [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 661-666. |
| [6] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [7] | Yangyi FANG,Qiang LI,Zhigao HUANG,Min LU,Kai HONG,Shudong ZHANG. Well-differentiated papillary mesothelial tumour of the tunica vaginalis: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 741-744. |
| [8] | Yuanyuan ZENG,Yun XIE,Daonan CHEN,Ruilan WANG. Related factors of euthyroid sick syndrome in patients with sepsis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 526-532. |
| [9] | Jian-bin LI,Meng-na LYU,Qiang CHI,Yi-lin PENG,Peng-cheng LIU,Rui WU. Early prediction of severe COVID-19 in patients with Sjögren’s syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1007-1012. |
| [10] | Huan-rui LIU,Xiang PENG,Sen-lin LI,Xin GOU. Risk modeling based on HER-2 related genes for bladder cancer survival prognosis assessment [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 793-801. |
| [11] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [12] | Dong LAN,Zhuo LIU,Yu-xuan LI,Guo-liang WANG,Xiao-jun TIAN,Lu-lin MA,Shu-dong ZHANG,Hong-xian ZHANG. Risk factors for massive hemorrhage after radical nephrectomy and removal of venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 825-832. |
| [13] | Han LU,Jian-yun ZHANG,Rong YANG,Le XU,Qing-xiang LI,Yu-xing GUO,Chuan-bin GUO. Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 702-707. |
| [14] | Yun-fei SHI,Hao-jie WANG,Wei-ping LIU,Lan MI,Meng-ping LONG,Yan-fei LIU,Yu-mei LAI,Li-xin ZHOU,Xin-ting DIAO,Xiang-hong LI. Analysis of clinicopathological and molecular abnormalities of angioimmunoblastic T-cell lymphoma [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 521-529. |
| [15] | Xiao-juan ZHU,Hong ZHANG,Shuang ZHANG,Dong LI,Xin LI,Ling XU,Ting LI. Clinicopathological features and prognosis of breast cancer with human epidermal growth factor receptor 2 low expression [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 243-253. |
|
||