北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 850-856. doi: 10.19723/j.issn.1671-167X.2021.05.007
前交叉韧带重建术后膝关节感染的诊断和治疗策略
王成1,孟令宇2,陈拿云1,李玳1,王健全1,敖英芳1,△( )
)
- 1.北京大学第三医院运动医学科,北京大学运动医学研究所,运动医学关节伤病北京市重点实验室,北京 100191
2.北京大学基础医学院,北京 100191
Management algorithm for septic arthritis after anterior cruciate ligament reconstruction
WANG Cheng1,MENG Ling-yu2,CHEN Na-yun1,LI Dai1,WANG Jian-quan1,AO Ying-fang1,△( )
)
- 1. Department of Sports Medicine, Peking University Third Hospital, Institute of Sports Medicine of Peking University, Beijing Key Laboratory of Sports Injuries, Beijing 100191, China
2. Peking University School of Basic Medical Sciences, Beijing 100191, China
摘要:
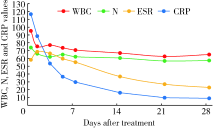
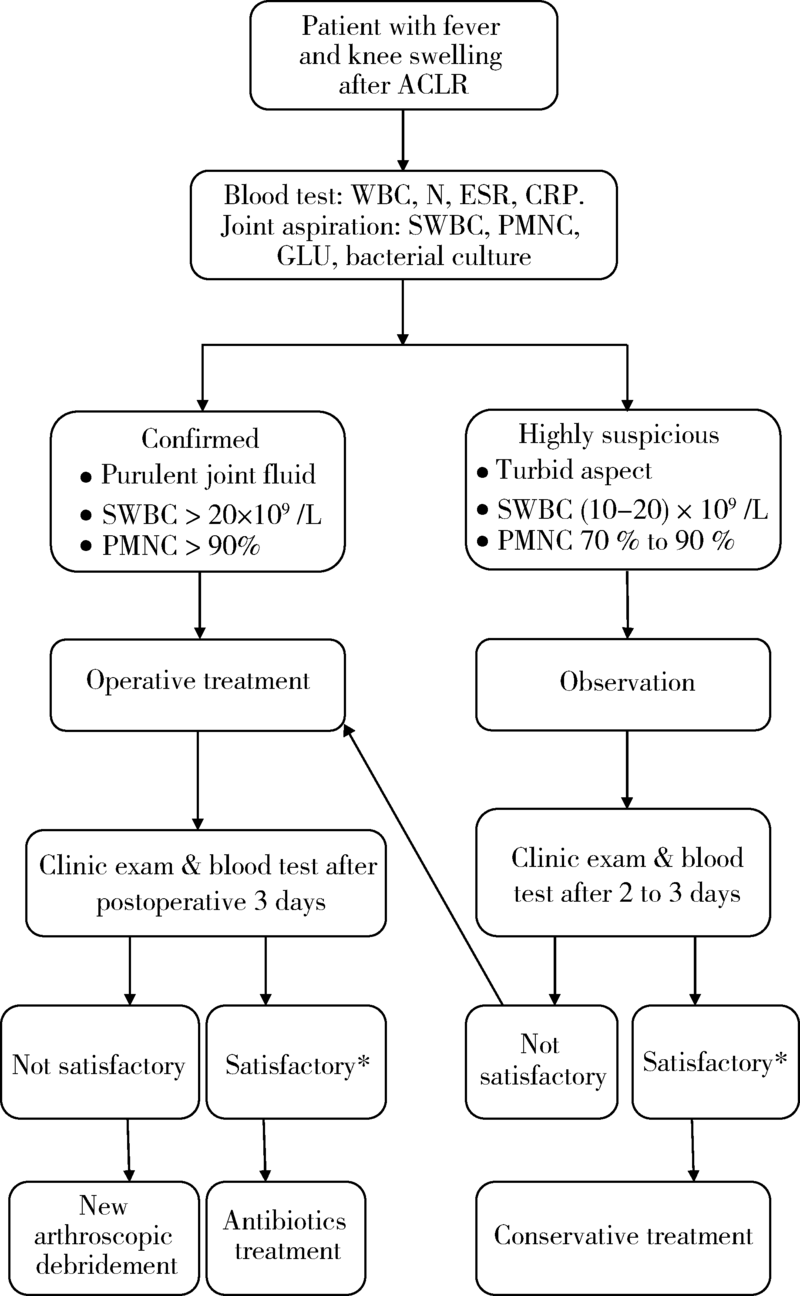
目的: 探讨关节镜下前交叉韧带重建术后膝关节感染的临床诊断和治疗策略。方法: 选择2001年1月至2020年12月在北京大学第三医院运动医学科行关节镜下前交叉韧带重建手术且术后发生膝关节感染的病例进行回顾性分析。通过对患者术后关节感染的发病过程、临床特征、试验室检查、治疗方法及随访结果进行分析,探讨最佳的临床诊断和治疗策略。结果: 20年间关节镜下前交叉韧带重建手术共27 867例,术后膝关节感染65例,感染率0.23%。临床表现有体温增高[(38.7±0.5) ℃]、膝关节肿痛、关节活动度受限。细菌培养阳性率 69.2%,其中凝固酶阴性葡萄球菌(占75.6%)、金黄色葡萄球菌(占15.6%)最常见。保守治疗组(16例)和手术治疗组(49例)均能有效控制感染,但保守治疗组体温恢复较慢(保守治疗组5.6 d,手术治疗组1.6 d,P=0.042)。结论: 前交叉韧带重建术后膝关节感染是一种发生率低,但后果严重的并发症,临床诊断建议及早进行关节腔穿刺和病原学检查,一旦确诊,建议尽早进行关节镜清理手术,并给予有效抗生素治疗。
中图分类号:
- R687
| [1] |
Murawski CD, Wolf MR, Araki D, et al. Anatomic anterior cruciate ligament reconstruction: current concepts and future perspective [J]. Cartilage, 2013, 4(3):27S-37S.
doi: 10.1177/1947603513486557 |
| [2] |
Williams RJ, Laurencin CT, Warren RF, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction. Diagnosis and management [J]. Am J Sports Med, 1997, 25(2):261-267.
doi: 10.1177/036354659702500222 |
| [3] |
McAllister DR, Parker RD, Cooper AE, et al. Outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction [J]. Am J Sports Med, 1999, 27(5):562-570.
doi: 10.1177/03635465990270050301 |
| [4] |
Viola R, Marzano N, Vianello R. An unusual epidemic of Staphylococcus-negative infections involving anterior cruciate ligament reconstruction with salvage of the graft and function [J]. Arthroscopy, 2000, 16(2):173-177.
pmid: 10705329 |
| [5] |
Indelli PF, Dillingham M, Fanton G, et al. Septic arthritis in postoperative anterior cruciate ligament reconstruction [J]. Clin Orthop Relat Res, 2002, 398:182-188.
doi: 10.1097/00003086-200205000-00026 |
| [6] |
Schollin-Borg M, Michaёlsson K, Rahme H. Presentation, outcome, and cause of septic arthritis after anterior cruciate ligament reconstruction: a case control study [J]. Arthroscopy, 2003, 19(9):941-947.
pmid: 14608312 |
| [7] |
Burks RT, Friederichs MG, Fink B, et al. Treatment of post-operative anterior cruciate ligament infections with graft removal and early reimplantation [J]. Am J Sports Med, 2003, 31(3):414-418.
doi: 10.1177/03635465030310031501 |
| [8] |
Fong SY, Tan JL. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction [J]. Ann Acad Med Singap, 2004, 33(2):228-234.
pmid: 15098639 |
| [9] |
Musso AD, McCormack RG. Infection after ACL reconstruction: what happens when cultures are negative [J]. Clin J Sport Med, 2005, 15(5):381-384.
pmid: 16162999 |
| [10] |
Zalavras CG, Patzakis MJ, Tibone J, et al. Treatment of persistent infection after anterior cruciate ligament surgery [J]. Clin Orthop Relat Res, 2005, 439:52-55.
doi: 10.1097/01.blo.0000181499.49740.e5 |
| [11] |
Judd D, Bottoni C, Kim D, et al. Infections following arthroscopic anterior cruciate ligament reconstruction [J]. Arthroscopy, 2006, 22(4):375-384.
doi: 10.1016/j.arthro.2005.12.002 |
| [12] |
Binnet MS, Basarir K. Risk and outcome of infection after different arthroscopic anterior cruciate ligament reconstruction techniques [J]. Arthroscopy, 2007, 23(8):862-868.
doi: 10.1016/j.arthro.2007.02.008 |
| [13] |
Van Tongel A, Stuyck J, Bellemans J, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, management and outcome [J]. Am J Sports Med, 2007, 35(7):1059-1063.
doi: 10.1177/0363546507299443 |
| [14] |
Schulz AP, Götze S, Schmidt HG, et al. Septic arthritis of the knee after anterior cruciate ligament surgery: a stage-adapted treatment regimen [J]. Am J Sports Med, 2007, 35(7):1064-1069.
doi: 10.1177/0363546507299744 |
| [15] |
Katz LM, Battaglia TC, Patino P, et al. A retrospective comparison of the incidence of bacterial infection following anterior cruciate ligament reconstruction with autograft versus allograft [J]. Arthroscopy, 2008, 24(12):1330-1335.
doi: 10.1016/j.arthro.2008.07.015 |
| [16] |
Iorio R, Vadalà A, Di VI, et al. Tunnel enlargement after anterior cruciate ligament reconstruction in patients with post-operative septic arthritis [J]. Knee Surg Sports Traumatol Arthrosc, 2008, 16(10):921-927.
doi: 10.1007/s00167-008-0575-1 |
| [17] |
Wang C, Ao Y, Wang J, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, presentation, treatment, and cause [J]. Arthroscopy, 2009, 25(3):243-249.
doi: 10.1016/j.arthro.2008.10.002 |
| [18] | Sajovic M, NiCAGL , Dernovš EMZ. Septic arthritis of the knee following anterior cruciate ligament reconstruction [J]. Orthop Rev (Pavia), 2009, 1(1):e3. |
| [19] |
Nag HL, Neogi DS, Nataraj AR, et al. Tubercular infection after arthroscopic anterior cruciate ligament reconstruction [J]. Arthroscopy, 2009, 25(2):131-136.
doi: 10.1016/j.arthro.2008.09.009 |
| [20] |
Monaco E, Maestri B, Labianca L, et al. Clinical and radiological outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction [J]. J Orthop Sci, 2010, 15(2):198-203.
doi: 10.1007/s00776-009-1447-3 |
| [21] |
Barker JU, Drakos MC, Maak TG, et al. Effect of graft selection on the incidence of postoperative infection in anterior cruciate ligament reconstruction [J]. Am J Sports Med, 2010, 38(2):281-286.
doi: 10.1177/0363546509346414 |
| [22] |
Benner RW, Shelbourne KD, Freeman H. Infections and patellar tendon ruptures after anterior cruciate ligament reconstruction: a comparison of ipsilateral and contralateral patellar tendon autografts [J]. Am J Sports Med, 2011, 39(3):519-525.
doi: 10.1177/0363546510388163 |
| [23] |
Sonnery-Cottet B, Archbold P, Zayni R, et al. Prevalence of septic arthritis after anterior cruciate ligament reconstruction among professional athletes [J]. Am J Sports Med, 2011, 39(11):2371-2376.
doi: 10.1177/0363546511417567 pmid: 21856928 |
| [24] |
Vertullo CJ, Quick M, Jones A, et al. A surgical technique using presoaked vancomycin hamstring grafts to decrease the risk of infection after anterior cruciate ligament reconstruction [J]. Arthroscopy, 2012, 28(3):337-342.
doi: 10.1016/j.arthro.2011.08.301 |
| [25] |
Schub DL, Schmitz LM, Sakamoto FA, et al. Long-term outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction [J]. Am J Sports Med, 2012, 40(12):2764-2770.
doi: 10.1177/0363546512461903 |
| [26] |
Torres-Claramunt R, Pelfort X, Erquicia J, et al. Knee joint infection after ACL reconstruction: prevalence, management and functional outcomes [J]. Knee Surg Sports Traumatol Arthrosc, 2013, 21(12):2844-2849.
doi: 10.1007/s00167-012-2264-3 |
| [27] |
RisticV , Maljanovic M, Harhaji V, et al. Infections after reconstructions of anterior cruciate ligament [J]. Med Pregl, 2014, 67(1/2):11-15.
doi: 10.2298/MPNS1402011R |
| [28] |
Abdel-Aziz A, Radwan YA, Rizk A. Multiple arthroscopic debridement and graft retention in septic knee arthritis after ACL reconstruction: a prospective case-control study [J]. Int Orthop, 2014, 38(1):73-82.
doi: 10.1007/s00264-013-2123-y pmid: 24100920 |
| [29] |
Boström WH, Mikkelsen C, Forssblad M, et al. Postoperative septic arthritis after anterior cruciate ligament reconstruction: does it affect the outcome? a retrospective controlled study [J]. Arthroscopy, 2014, 30(9):1100-1109.
doi: 10.1016/j.arthro.2014.03.019 |
| [30] |
Calvo R, Figueroa D, Anastasiadis Z, et al. Septic arthritis in ACL reconstruction surgery with hamstring autografts. eleven years of experience [J]. Knee, 2014, 21(3):717-720.
doi: 10.1016/j.knee.2014.01.007 |
| [31] |
Schuster P, Schulz M, Immendoerfer M, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: evaluation of an arthroscopic graft-retaining treatment protocol [J]. Am J Sports Med, 2015, 43(12):3005-3012.
doi: 10.1177/0363546515603054 pmid: 26403209 |
| [32] |
Pérez-Prieto D, Trampuz A, Torres-Claramunt R, et al. Infections after anterior cruciate ligament reconstruction: which antibiotic after arthroscopic debridement? [J]. J Knee Surg, 2017, 30(4):309-313.
doi: 10.1055/s-0036-1584559 pmid: 27367205 |
| [33] |
Hantes ME, Raoulis VA, Doxariotis N, et al. Management of septic arthritis after arthroscopic anterior cruciate ligament reconstruction using a standard surgical protocol [J]. Knee, 2017, 24(3):588-593.
doi: 10.1016/j.knee.2017.02.007 |
| [34] |
Torres-Claramunt R, Gelber P, Pelfort X, et al. Managing septic arthritis after knee ligament reconstruction [J]. Int Orthop, 2016, 40(3):607-614.
doi: 10.1007/s00264-015-2884-6 pmid: 26239533 |
| [35] |
Wang C, Lee YH, Siebold R. Recommendations for the management of septic arthritis after ACL reconstruction [J]. Knee Surg Sports Traumatol Arthrosc, 2014, 22(9):2136-2144.
doi: 10.1007/s00167-013-2648-z |
| [36] |
Muscolo DL, Carbo L, Aponte-Tinao LA, et al. Massive bone loss from fungal infection after anterior cruciate ligament arthroscopic reconstruction [J]. Clin Orthop Relat Res, 2009, 467(9):2420-2425.
doi: 10.1007/s11999-009-0714-0 |
| [37] |
Wang C, Ao Y, Fan X, et al. C-reactive protein and erythrocyte sedimentation rate changes after arthroscopic anterior cruciate ligament reconstruction: guideline to diagnose and monitor postoperative infection [J]. Arthroscopy, 2014, 30(9):1110-1115.
doi: 10.1016/j.arthro.2014.03.025 |
| [38] |
Paci JM, Schweizer SK, Wilbur DM, et al. Results of laboratory evaluation of acute knee effusion after anterior cruciate ligament reconstruction: what is found in patients with a noninfected, painful postoperative knee [J]. Am J Sports Med, 2010, 38(11):2267-2272.
doi: 10.1177/0363546510374573 |
| [1] | 任爽, 时会娟, 梁子轩, 张思, 胡晓青, 黄红拾, 敖英芳. 前交叉韧带重建术后侧切动作的生物力学特征[J]. 北京大学学报(医学版), 2024, 56(5): 868-873. |
| [2] | 万利, 张周沧, 丁嘉祥, 王梅. 中心静脉导管拔除后静脉空气栓塞1例[J]. 北京大学学报(医学版), 2024, 56(5): 938-941. |
| [3] | 王江静,魏顺依,敖英芳,杨渝平. 前交叉韧带重建术后三种不同药物镇痛早期疗效的对比[J]. 北京大学学报(医学版), 2024, 56(2): 293-298. |
| [4] | 董佳芸,李雪芬,路瑞芳,胡文杰,孟焕新. 血管化骨瓣重建颌骨种植体周软组织病理学特点[J]. 北京大学学报(医学版), 2024, 56(1): 25-31. |
| [5] | 王聪伟,高敏,于尧,章文博,彭歆. 游离腓骨瓣修复下颌骨缺损术后义齿修复的临床分析[J]. 北京大学学报(医学版), 2024, 56(1): 66-73. |
| [6] | 许素环,王蓓蓓,庞秋颖,钟丽君,丁炎明,黄燕波,车新艳. 等体温膀胱冲洗对经尿道前列腺电切术患者干预效果的meta分析[J]. 北京大学学报(医学版), 2023, 55(4): 676-683. |
| [7] | 吴超,刘彬,谢京城,王振宇,马长城,杨军,孙建军,陈晓东,于涛,林国中,司雨,韩芸峰,陈素华,尹晓亮,马千权,郑穆天,曾琳. 神经根袖加固重建术治疗症状性骶管Tarlov囊肿71例临床分析[J]. 北京大学学报(医学版), 2023, 55(1): 133-138. |
| [8] | 李辉,高阳旭,王书磊,姚红新. 恶性肿瘤患儿完全植入式静脉输液港手术并发症[J]. 北京大学学报(医学版), 2022, 54(6): 1167-1171. |
| [9] | 姜保国,张培训. 老年髋部骨折的围手术期风险评估[J]. 北京大学学报(医学版), 2022, 54(5): 803-809. |
| [10] | 于博,赵扬玉,张喆,王永清. 妊娠合并感染性心内膜炎1例[J]. 北京大学学报(医学版), 2022, 54(3): 578-580. |
| [11] | 吴俊慧,武轶群,吴瑶,王紫荆,吴涛,秦雪英,王梦莹,王小文,王伽婷,胡永华. 北京城镇职工2型糖尿病患者缺血性脑卒中发病率及主要危险因素[J]. 北京大学学报(医学版), 2022, 54(2): 249-254. |
| [12] | 李伟浩,李伟,张学民,李清乐,焦洋,张韬,蒋京军,张小明. 去分支杂交手术和传统手术治疗胸腹主动脉瘤的结果比较[J]. 北京大学学报(医学版), 2022, 54(1): 177-181. |
| [13] | 蒋艳芳,王健,王永健,刘佳,裴殷,刘晓鹏,敖英芳,马勇. 前交叉韧带翻修重建术后中长期临床疗效及影响因素[J]. 北京大学学报(医学版), 2021, 53(5): 857-863. |
| [14] | 任爽,时会娟,张家豪,刘振龙,邵嘉艺,朱敬先,胡晓青,黄红拾,敖英芳. 前交叉韧带重建术后移植物应力的有限元分析[J]. 北京大学学报(医学版), 2021, 53(5): 865-870. |
| [15] | 苗欣,黄红拾,胡晓青,时会娟,任爽,敖英芳. 膝关节前交叉韧带断裂后单腿位置觉测试时脑电功率谱的变化特征[J]. 北京大学学报(医学版), 2021, 53(5): 871-876. |
|
||