北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (5): 860-867. doi: 10.19723/j.issn.1671-167X.2024.05.017
miR-125b-5p修饰脐带间充质干细胞对系统性红斑狼疮的免疫调控机制
武志慧1, 胡明智1, 赵巧英1, 吕凤凤1, 张晶莹2, 张伟1, 王永福2, 孙晓林1,*( ), 王慧2,*(
), 王慧2,*( )
)
- 1. 包头医学院第一附属医院中心实验室(内蒙古自治区自体免疫学重点实验室),内蒙古自治区包头 014010
2. 包头医学院第一附属医院风湿免疫科,内蒙古自治区包头 014010
Immunomodulatory mechanism of umbilical cord mesenchymal stem cells modified by miR-125b-5p in systemic lupus erythematosus
Zhihui WU1, Mingzhi HU1, Qiaoying ZHAO1, Fengfeng LV1, Jingying ZHANG2, Wei ZHANG1, Yongfu WANG2, Xiaolin SUN1,*( ), Hui WANG2,*(
), Hui WANG2,*( )
)
- 1. Central Laboratory, First Affiliated Hospital of Baotou Medical College (Inner Mongolia Key Laboratory of Autoimmunology), Baotou 014010, Inner Mongolia Autonomous Region, China
2. Department of Rheumatism and Immunology, First Affiliated Hospital of Baotou Medical College, Baotou 014010, Inner Mongolia Autonomous Region, China
摘要:
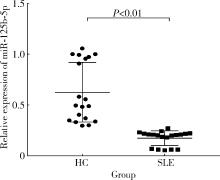
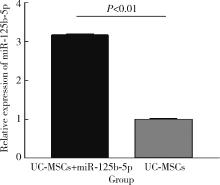
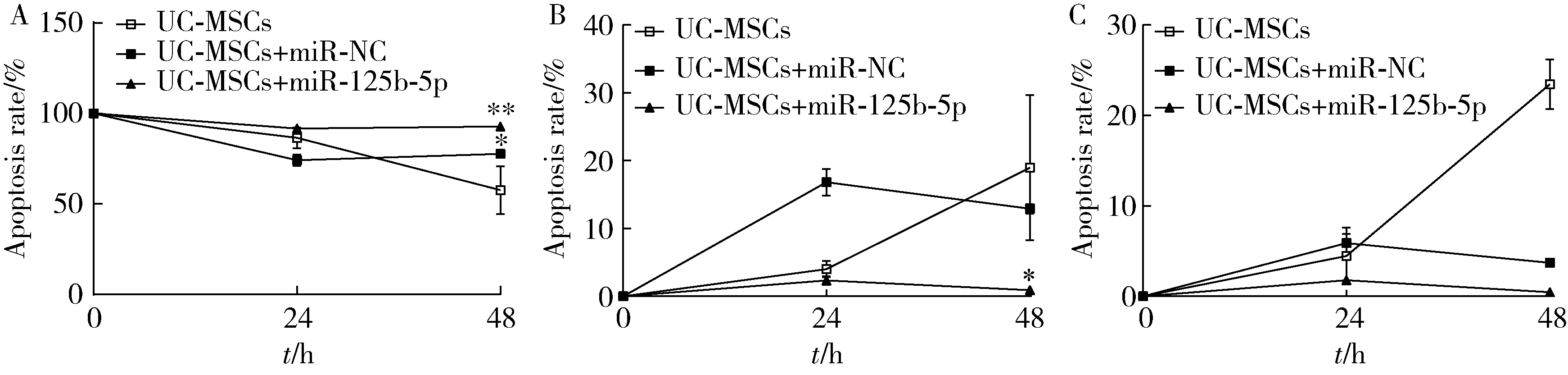
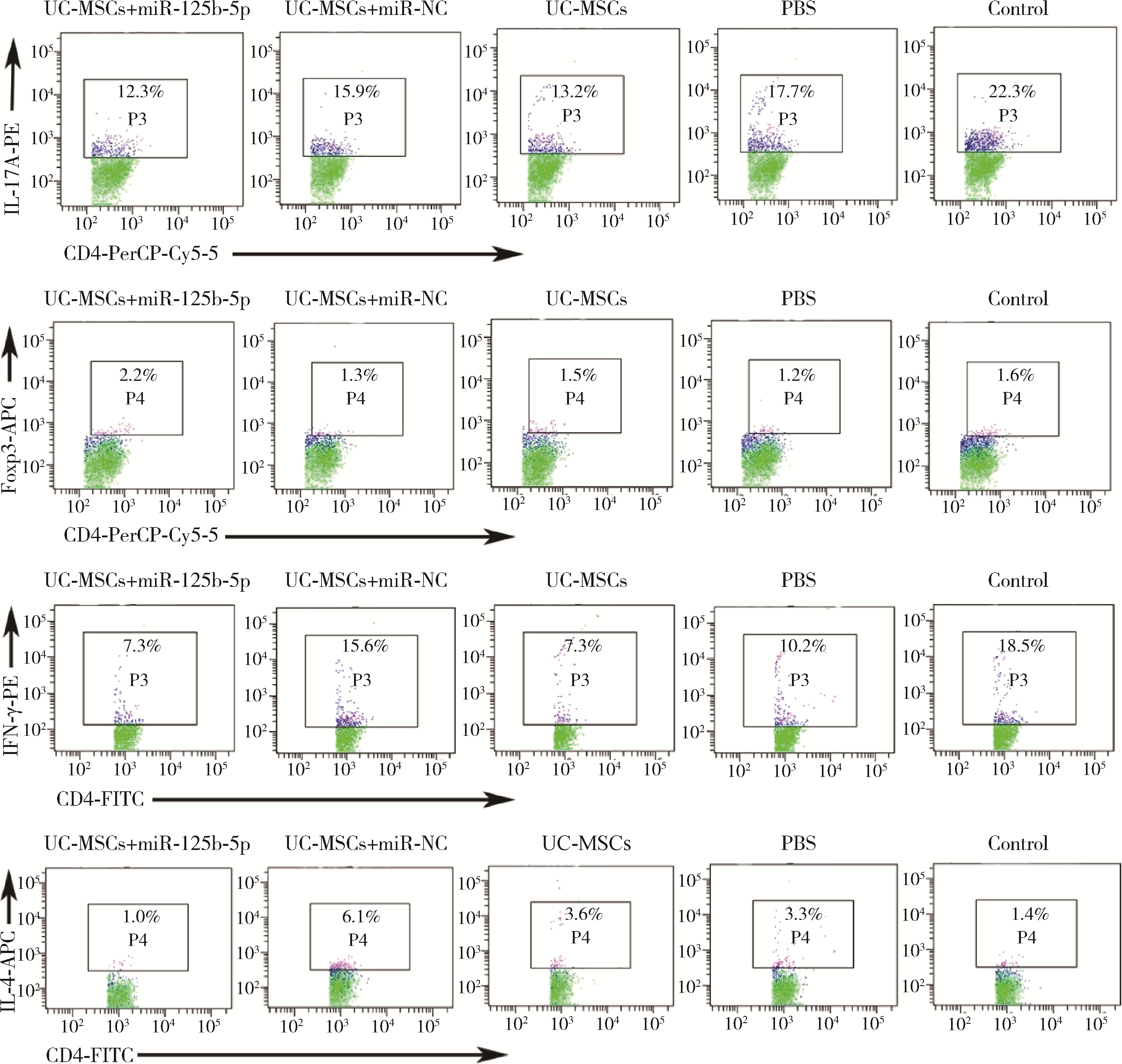
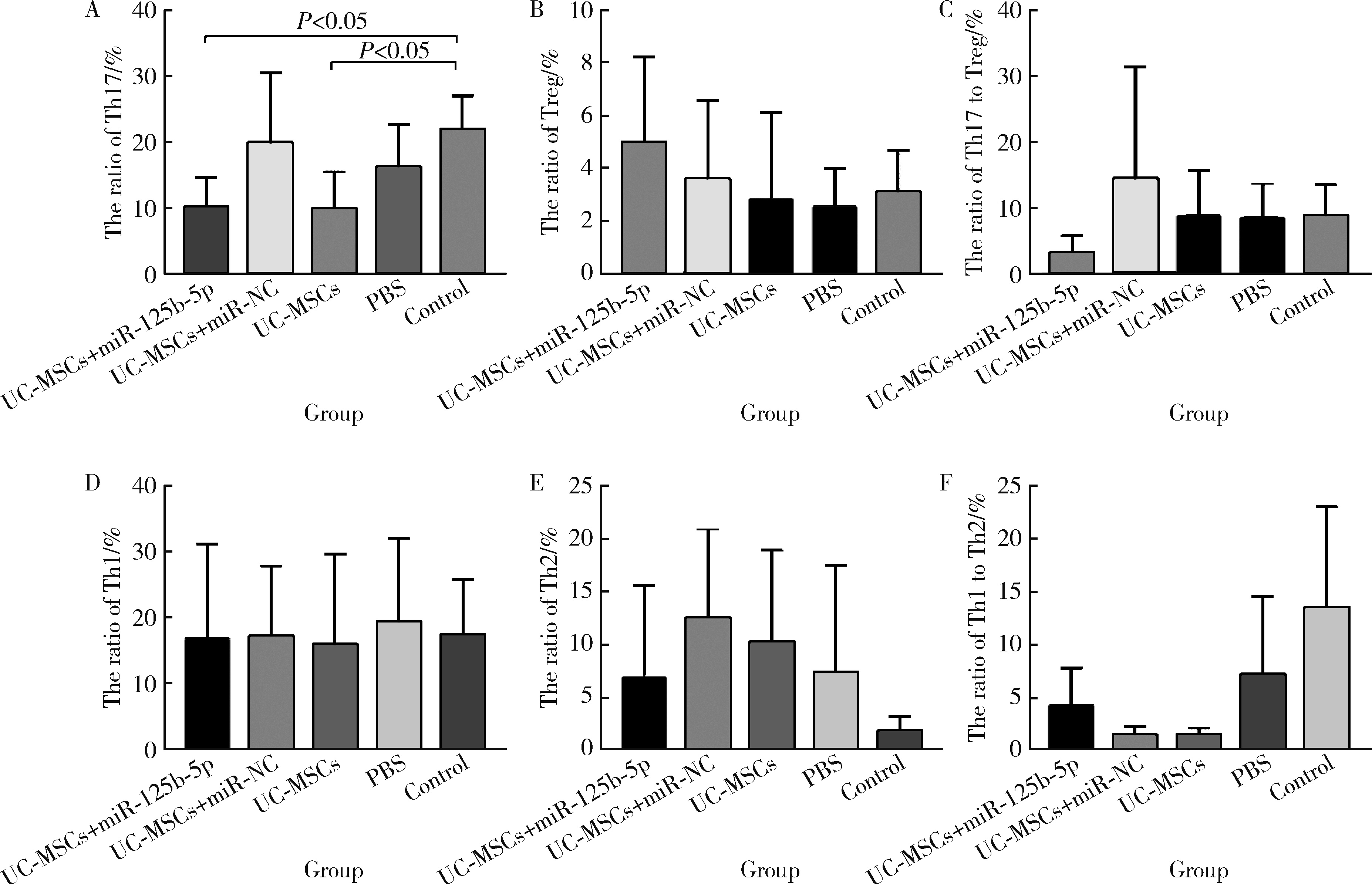
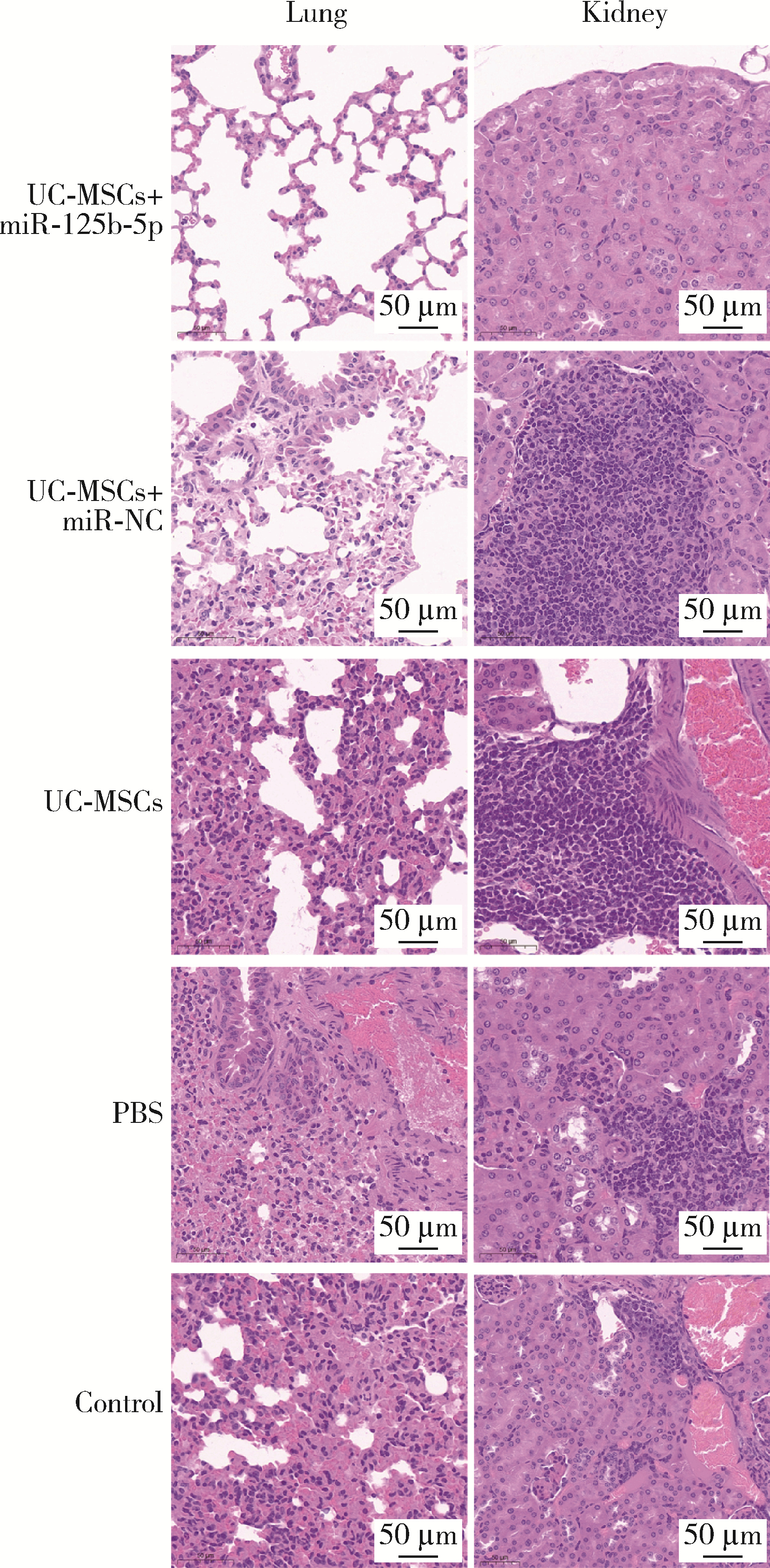
目的: 研究miR-125b-5p修饰脐带间充质干细胞(umbilical cord mesenchymal stem cells,UC-MSCs)对系统性红斑狼疮(systemic lupus erythematosus,SLE)的免疫调控作用机制。方法: 实时荧光定量PCR检测miR-125b-5p在UC-MSCs和SLE患者、健康体检者外周血单个核细胞中的表达水平;Annexin V-FITC/PI凋亡检测试剂盒检测miR-125b-5p对UC-MSCs的凋亡影响;每周对MRL/lpr小鼠进行尾静脉注射UC-MSCs,5周后流式细胞术检测各组小鼠脾细胞T淋巴细胞亚群分化情况;ELISA法检测各组MRL/lpr小鼠血清中白细胞介素(interleukin,IL)-4和IL-17A表达水平;苏木精-伊红染色法观察MRL/lpr小鼠肺和肾组织病理变化。结果: 与健康对照组相比,SLE患者外周血单个核细胞中miR-125b-5p的表达水平显著下调(P < 0.01);与UC-MSCs相比,miR-125b-5p转染UC-MSCs组miR-125b-5p的表达水平显著上调(P < 0.01)。miR-125b-5p转染UC-MSCs 48 h可显著提高细胞存活率(P < 0.01);与未处理的MRL/lpr小鼠组相比,miR-125b-5p修饰UC-MSCs对MRL/lpr小鼠脾脏Th17细胞分化具有明显的下调作用(P < 0.05),且在小鼠血清中IL-4表达水平明显升高(P < 0.05),IL-17A表达水平明显减低(P < 0.05)。经miR-125b-5p修饰的UC-MSCs治疗后,MRL/lpr小鼠肺和肾组织内炎性细胞浸润和微血栓减少。结论: miR-125b-5p修饰UC-MSCs对SLE具有免疫调控作用。
中图分类号:
- R593.2
| 1 |
Tsokos GC . Systemic lupus erythematosus[J]. N Engl J Med, 2011, 365 (22): 2110- 2121.
doi: 10.1056/NEJMra1100359 |
| 2 |
Relle M , Foehr B , Schwarting A . Epigenetic aspects of systemic lupus erythematosus[J]. Rheumatol Ther, 2015, 2 (1): 33- 46.
doi: 10.1007/s40744-015-0014-y |
| 3 |
Basta F , Fasola F , Triantafyllias K , et al. Systemic lupus erythematosus (SLE) therapy: The old and the new[J]. Rheumatol Ther, 2020, 7 (3): 433- 446.
doi: 10.1007/s40744-020-00212-9 |
| 4 |
Sharabi A , Tsokos GC . T cell metabolism: New insights in systemic lupus erythematosus pathogenesis and therapy[J]. Nat Rev Rheumatol, 2020, 16 (2): 100- 112.
doi: 10.1038/s41584-019-0356-x |
| 5 |
Muhammad Yusoff F , Wong KK , Mohd Redzwan N . Th1, Th2, and Th17 cytokines in systemic lupus erythematosus[J]. Autoimmunity, 2020, 53 (1): 8- 20.
doi: 10.1080/08916934.2019.1693545 |
| 6 |
Serakinci N , Fahrioglu U , Christensen R . Mesenchymal stem cells, cancer challenges and new directions[J]. Eur J Cancer, 2014, 50 (8): 1522- 1530.
doi: 10.1016/j.ejca.2014.02.011 |
| 7 |
Drela K , Lech W , Figiel-Dabrowska A , et al. Enhanced neuro-therapeutic potential of Wharton' s jelly-derived mesenchymal stem cells in comparison with bone marrow mesenchymal stem cells culture[J]. Cytotherapy, 2016, 18 (4): 497- 509.
doi: 10.1016/j.jcyt.2016.01.006 |
| 8 |
Liu L , Wong CW , Han M , et al. Meta-analysis of preclinical studies of mesenchymal stromal cells to treat rheumatoid arthritis[J]. EBioMedicine, 2019, 47, 563- 577.
doi: 10.1016/j.ebiom.2019.08.073 |
| 9 |
Qi J , Tang X , Li W , et al. Mesenchymal stem cells inhibited the differentiation of MDSCs via COX2/PGE2 in experimental sialadenitis[J]. Stem Cell Res Ther, 2020, 11 (1): 325.
doi: 10.1186/s13287-020-01837-x |
| 10 | Liu C , Zhang H , Tang X , et al. Mesenchymal stem cells promote the osteogenesis in collagen-induced arthritic mice through the inhibition of TNF-α[J]. Stem Cells Int, 2018, 2018, 4069032. |
| 11 |
Choudhery MS , Badowski M , Muise A , et al. Donor age negatively impacts adipose tissue-derived mesenchymal stem cell expansion and differentiation[J]. J Transl Med, 2014, 12, 8.
doi: 10.1186/1479-5876-12-8 |
| 12 | Escacena N , Quesada-Hernández E , Capilla-Gonzalez V , et al. Bottlenecks in the efficient use of advanced therapy medicinal products based on mesenchymal stromal cells[J]. Stem Cells Int, 2015, 2015, 895714. |
| 13 |
Fischer UM , Harting MT , Jimenez F , et al. Pulmonary passage is a major obstacle for intravenous stem cell delivery: The pulmonary first-pass effect[J]. Stem Cells Dev, 2009, 18 (5): 683- 692.
doi: 10.1089/scd.2008.0253 |
| 14 |
Abdelmohsen K , Gorospe M . Noncoding RNA control of cellular senescence[J]. Wiley Interdiscip Rev RNA, 2015, 6 (6): 615- 629.
doi: 10.1002/wrna.1297 |
| 15 | Su T , Xiao Y , Xiao Y , et al. Bone marrow mesenchymal stem cells-derived exosomal MiR-29b-3p regulates aging-associated insulin resistance[J]. ACS Nano, 2019, 13 (2): 2450- 2462. |
| 16 |
Meng Y , Eirin A , Zhu XY , et al. Micro-RNAs regulate metabolic syndrome-induced senescence in porcine adipose tissue-derived mesenchymal stem cells through the P16/MAPK pathway[J]. Cell Transplant, 2018, 27 (10): 1495- 1503.
doi: 10.1177/0963689718795692 |
| 17 | Vishnoi A , Rani S . MiRNA biogenesis and regulation of diseases: An overview[J]. Methods Mol Biol, 2017, 1509, 1- 10. |
| 18 | Gong B , Zheng L , Lu Z , et al. Mesenchymal stem cells negatively regulate CD4+ T cell activation in patients with primary Sjögren syndrome through the miRNA-125b and miRNA-155 TCR pathway[J]. Mol Med Rep, 2021, 23 (1): 43. |
| 19 |
Xiu L , Xing Q , Mao J , et al. miRNA-125b-5p suppresses hypo-thyroidism development by targeting signal transducer and activator of transcription 3[J]. Med Sci Monit, 2018, 24, 5041- 5049.
doi: 10.12659/MSM.907510 |
| 20 |
胡明智, 张晶莹, 杨国安, 等. miR-1-5p修饰脐带间充质干细胞对系统性红斑狼疮T淋巴细胞亚群的免疫调节[J]. 中国组织工程研究, 2021, 25 (31): 4928- 4938.
doi: 10.12307/2021.132 |
| 21 |
Gentile P , Sterodimas A . Adipose-derived stromal stem cells (ASCs) as a new regenerative immediate therapy combating coronavirus (COVID-19)-induced pneumonia[J]. Expert Opin Biol Ther, 2020, 20 (7): 711- 716.
doi: 10.1080/14712598.2020.1761322 |
| 22 |
Toyserkani NM , Jørgensen MG , Tabatabaeifar S , et al. Concise review: A safety assessment of adipose-derived cell therapy in cli-nical trials: A systematic review of reported adverse events[J]. Stem Cells Transl Med, 2017, 6 (9): 1786- 1794.
doi: 10.1002/sctm.17-0031 |
| 23 |
Chen C , Liang J , Yao G , et al. Mesenchymal stem cells upregulate Treg cells via sHLA-G in SLE patients[J]. Int Immuno-pharmacol, 2017, 44, 234- 241.
doi: 10.1016/j.intimp.2017.01.024 |
| 24 | 张立民. 系统性红斑狼疮microRNA表达谱和功能的初步研究[D]. 北京: 中国协和医科大学, 2010. |
| 25 |
Wang D , Huang S , Yuan X , et al. The regulation of the Treg/Th17 balance by mesenchymal stem cells in human systemic lupus erythematosus[J]. Mol Immunol, 2017, 14 (5): 423- 431.
doi: 10.1038/cmi.2015.89 |
| 26 |
Golpanian S , DiFede DL , Pujol MV , et al. Rationale and design of the allogeneiC human mesenchymal stem cells (hMSC) in patients with aging fRAilTy via intravenoUS delivery (CRATUS) study: A phase Ⅰ/Ⅱ, randomized, blinded and placebo controlled trial to evaluate the safety and potential efficacy of allogeneic human mesenchymal stem cell infusion in patients with aging frailty[J]. Oncotarget, 2016, 7 (11): 11899- 11912.
doi: 10.18632/oncotarget.7727 |
| 27 |
Yang J , Yang X , Zou H , et al. Oxidative stress and Treg and Th17 dysfunction in systemic lupus erythematosus[J]. Oxid Med Cell Longev, 2016, 2016, 2526174.
doi: 10.1155/2016/2526174 |
| 28 |
Li D , Guo B , Wu H , et al. Interleukin-17 in systemic lupus erythematosus: A comprehensive review[J]. Autoimmunity, 2015, 48 (6): 353- 361.
doi: 10.3109/08916934.2015.1037441 |
| 29 |
Chen DY , Chen YM , Wen MC , et al. The potential role of Th17 cells and Th17-related cytokines in the pathogenesis of lupus nephritis[J]. Lupus, 2012, 21 (13): 1385- 1396.
doi: 10.1177/0961203312457718 |
| 30 |
La Cava A . Tregs in SLE: An Update[J]. Curr Rheumatol Rep, 2018, 20 (2): 6.
doi: 10.1007/s11926-018-0714-8 |
| 31 |
Beringer A , Noack M , Miossec P . IL-17 in chronic inflammation: From discovery to targeting[J]. Trends Mol Med, 2016, 22 (3): 230- 241.
doi: 10.1016/j.molmed.2016.01.001 |
| 32 |
Dolff S , Bijl M , Huitema MG , et al. Disturbed Th1, Th2, Th17 and T(reg) balance in patients with systemic lupus erythematosus[J]. Clin Immunol, 2011, 141 (2): 197- 204.
doi: 10.1016/j.clim.2011.08.005 |
| 33 |
Moseley TA , Haudenschild DR , Rose L , et al. Interleukin-17 family and IL-17 receptors[J]. Cytokine Growth Factor Rev, 2003, 14 (2): 155- 174.
doi: 10.1016/S1359-6101(03)00002-9 |
| 34 | Qu N , Xu M , Mizoguchi I , et al. Pivotal roles of T-helper 17-related cytokines, IL-17, IL-22, and IL-23, in inflammatory diseases[J]. Clin Dev Immunol, 2013, 2013, 968549. |
| 35 |
Ghali JR , Holdsworth SR , Kitching AR . Targeting IL-17 and IL-23 in immune mediated renal disease[J]. Curr Med Chem, 2015, 22 (38): 4341- 4365.
doi: 10.2174/0929867322666151030163022 |
| 36 |
Talaat RM , Mohamed SF , Bassyouni IH , et al. Th1/Th2/Th17/Treg cytokine imbalance in systemic lupus erythematosus (SLE) patients: Correlation with disease activity[J]. Cytokine, 2015, 72 (2): 146- 153.
doi: 10.1016/j.cyto.2014.12.027 |
| 37 |
Zickert A , Amoudruz P , Sundström Y , et al. IL-17 and IL-23 in lupus nephritis: Association to histopathology and response to treatment[J]. BMC immunol, 2015, 16 (1): 7.
doi: 10.1186/s12865-015-0070-7 |
| 38 |
Jha AN , Singh VK , Kumari N , et al. IL-4 haplotype -590T, -34T and intron-3 VNTR R2 is associated with reduced malaria risk among ancestral indian tribal populations[J]. PLoS One, 2012, 7 (10): e48136.
doi: 10.1371/journal.pone.0048136 |
| 39 |
Patterson D , Jones C , Hart I , et al. The human interleukin-1 receptor antagonist (IL1RN) gene is located in the chromosome 2q14 region[J]. Genomics, 1993, 15 (1): 173- 176.
doi: 10.1006/geno.1993.1025 |
| 40 | Rapoport M , Bloch O . Systemic lupus erythematosus[J]. N Engl J Med, 2012, 366 (6): 574. |
| 41 |
Tsokos GC , Lo MS , Costa Reis P , et al. New insights into the immunopathogenesis of systemic lupus erythematosus[J]. Nat Rev Rheumatol, 2016, 12 (12): 716- 730.
doi: 10.1038/nrrheum.2016.186 |
| [1] | 王红彦, 李鑫铭, 房柯池, 朱华群, 贾汝琳, 王晶. 系统性红斑狼疮疾病活动度相关特征分析及评估模型的构建[J]. 北京大学学报(医学版), 2024, 56(6): 1017-1022. |
| [2] | 陈丹丹, 李云, 卢情怡, 相晓红, 孙峰, 李英妮, 赵静, 王红彦, 李春. 育龄期系统性红斑狼疮患者卵巢功能的评价及其影响因素[J]. 北京大学学报(医学版), 2024, 56(6): 1023-1028. |
| [3] | 王莉, 高超, 任欢欢, 沈艳平, 黄晓玮, 姚鸿, 韩丹丹. 系统性红斑狼疮患者自我管理能力现状及相关因素分析[J]. 北京大学学报(医学版), 2024, 56(6): 1029-1035. |
| [4] | 柴静, 王钥, 穆荣, 赵金霞. 系统性红斑狼疮累及穹窿柱导致低钠血症1例[J]. 北京大学学报(医学版), 2024, 56(6): 1115-1118. |
| [5] | 王明霞, 丁菱, 王敏, 邹婵娟, 颜丝语, 梁颖文, 王伟佳, 何善智. 双靶点嵌合抗原受体T细胞治疗系统性红斑狼疮患者停药后安全孕产1例[J]. 北京大学学报(医学版), 2024, 56(6): 1119-1125. |
| [6] | 乔佳佳,田聪,黄晓波,刘军. 肾结石合并系统性红斑狼疮行经皮肾镜碎石取石术的安全性和有效性评估[J]. 北京大学学报(医学版), 2024, 56(4): 745-749. |
| [7] | 任立敏,赵楚楚,赵义,周惠琼,张莉芸,王友莲,沈凌汛,范文强,李洋,厉小梅,王吉波,程永静,彭嘉婧,赵晓珍,邵苗,李茹. 系统性红斑狼疮低疾病活动度及缓解状况的真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 273-278. |
| [8] | 罗芷筠,吴佳佳,宋优,梅春丽,杜戎. 伴神经精神系统病变的系统性红斑狼疮相关巨噬细胞活化综合征2例[J]. 北京大学学报(医学版), 2023, 55(6): 1111-1117. |
| [9] | 姚海红,杨帆,唐素玫,张霞,何菁,贾园. 系统性红斑狼疮及成人Still病合并巨噬细胞活化综合征的临床特点及诊断指标[J]. 北京大学学报(医学版), 2023, 55(6): 966-974. |
| [10] | 赵祥格,刘佳庆,黄会娜,陆智敏,白自然,李霞,祁荆荆. 干扰素-α介导系统性红斑狼疮外周血CD56dimCD57+自然杀伤细胞功能的损伤[J]. 北京大学学报(医学版), 2023, 55(6): 975-981. |
| [11] | 张琳崎,赵静,王红彦,王宗沂,李英妮,汤稷旸,李思莹,曲进锋,赵明威. 抗ENO1抗体与狼疮性视网膜病变的相关性[J]. 北京大学学报(医学版), 2022, 54(6): 1099-1105. |
| [12] | 李敏,侯林卿,金月波,何菁. 系统性红斑狼疮合并视网膜病变的临床及免疫学特点[J]. 北京大学学报(医学版), 2022, 54(6): 1106-1111. |
| [13] | 邵苗,郭惠芳,雷玲彦,赵清,丁艳杰,林进,吴锐,于峰,李玉翠,苗华丽,张莉芸,杜燕,焦瑞英,庞丽霞,龙丽,栗占国,李茹. 短间期小剂量环磷酰胺治疗系统性红斑狼疮耐受性的多中心对照研究[J]. 北京大学学报(医学版), 2022, 54(6): 1112-1116. |
| [14] | 韩超,周祝兴,陈有荣,董子慧,余家阔. 绵羊外周血间充质干细胞的生物学特性[J]. 北京大学学报(医学版), 2022, 54(6): 1151-1157. |
| [15] | 帅婷,刘娟,郭艳艳,金婵媛. 敲减长链非编码RNA MIR4697HG抑制骨髓间充质干细胞成脂向分化[J]. 北京大学学报(医学版), 2022, 54(2): 320-326. |
|
||