北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (5): 836-840. doi: 10.19723/j.issn.1671-167X.2025.05.004
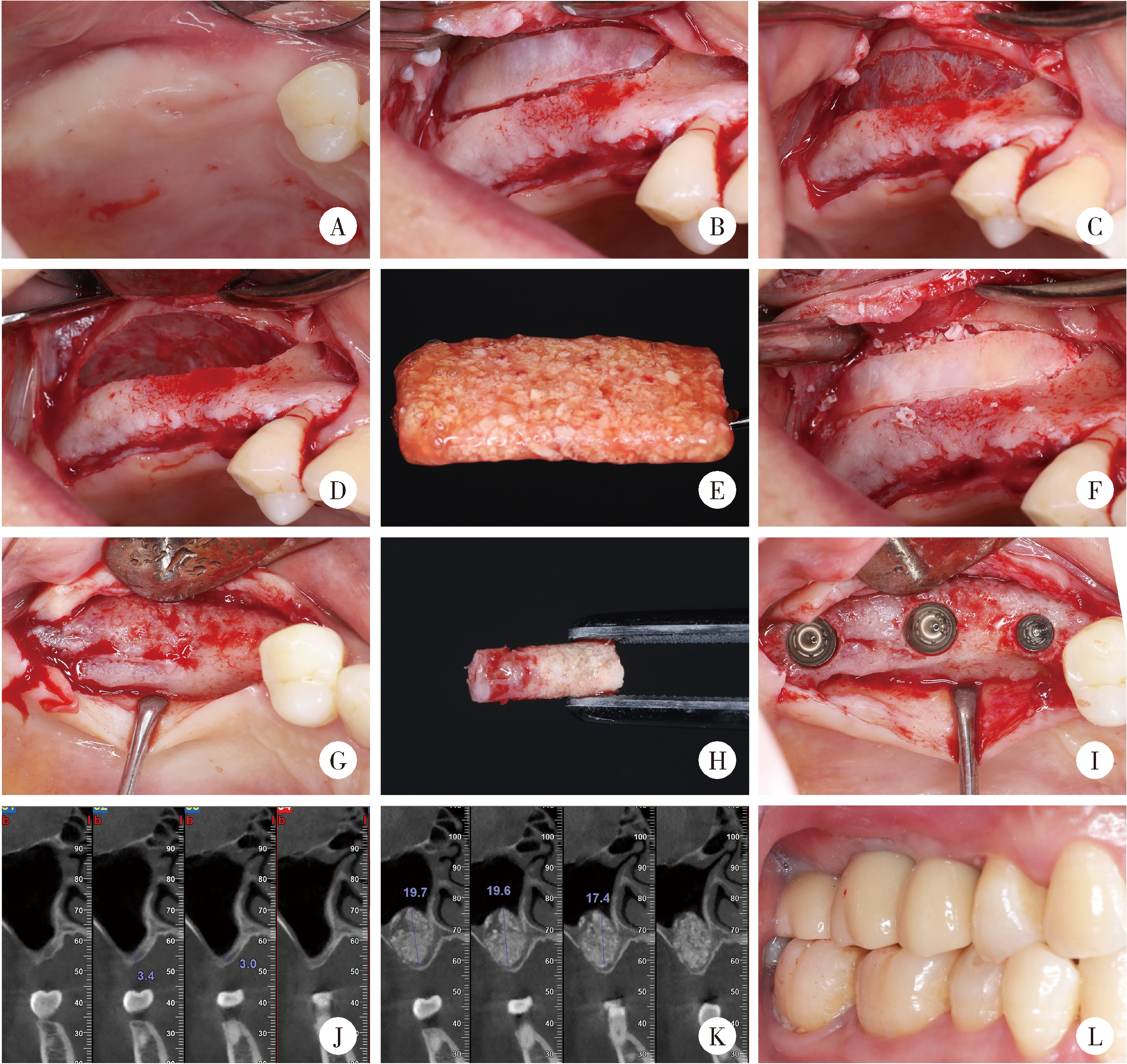
口腔种植中血浆基质的临床转化现状与前沿探索
- 武汉大学口腔医(学)院种植科, 武汉 430079
Current situation and exploration of clinical transformation of plasmatrix in oral implantology
Yulan WANG, Hao ZENG, Yufeng ZHANG*( )
)
- Department of Implantology, School and Hospital of Stomatology, Wuhan University, Wuhan 430079, China
摘要: 随着口腔种植学的快速发展,种植体的长期稳定性与美学效果日益受到重视,而充足、健康的软硬组织被认为是其关键保障因素之一。在众多组织再生策略中,血浆基质作为一种源自患者自体血液的生物衍生材料,因其富含多种生长因子、活细胞和纤维蛋白,具有良好的生物相容性、可控的降解性能及简便的制备流程,近年来在口腔种植相关的软硬组织修复中展现出独特而显著的临床价值,应用范围持续扩大。本文在系统梳理相关文献和现有研究证据的基础上,全面综述了血浆基质在口腔种植领域的基础研究与临床应用进展,重点探讨了其材料学分类、分子作用机制、促进组织再生的生物学效应及其在不同临床适应证中的应用策略。同时,本文还对当前研究中存在的技术瓶颈与争议问题进行了深入分析,并提出了未来可能的研究方向与技术发展趋势,旨在为临床实践提供循证支持,为后续科学研究提供理论依据与方法参考。
中图分类号:
- R783.6
| 1 |
|
| 2 |
doi: 10.1002/JPER.22-0196 |
| 3 |
|
| 4 |
|
| 5 |
doi: 10.1111/cid.12343 |
| 6 |
|
| 7 |
Farshidfar N, Apaza Alccayhuaman KA, Estrin NE, et al. Advantages of horizontal centrifugation of platelet-rich fibrin in regenerative medicine and dentistry[J/OL]. Periodontol 2000, 2025. [2025-03-25]. http://doi.org/10.1111/prd.12625.
|
| 8 |
张玉峰. 血浆基质制品的前世今生[J]. 中华口腔医学杂志, 2021, 56 (8): 740- 746.
|
| 9 |
doi: 10.1089/ten.teb.2016.0233 |
| 10 |
Farshidfar N, Amiri MA, Estrin NE, et al. Platelet-rich plasma (PRP) versus injectable platelet-rich fibrin (i-PRF): A syste-matic review across all fields of medicine[J/OL]. Periodontol 2000, 2025. [2025-03-24]. http://doi.org/10.1111/prd.12626.
|
| 11 |
doi: 10.1016/j.biopha.2023.115795 |
| 12 |
doi: 10.1002/jper.11364.Onlineaheadofprint |
| 13 |
doi: 10.1016/j.acthis.2023.152059 |
| 14 |
doi: 10.1002/jbm.a.36792 |
| 15 |
doi: 10.1111/prd.12538 |
| 16 |
doi: 10.1007/s00784-023-05108-w |
| 17 |
|
| 18 |
张玉峰, 王宇蓝. 血浆基质在口腔种植垂直骨增量中的应用[J]. 口腔疾病防治, 2022, 30 (12): 837- 843.
|
| 19 |
张玉峰, 王宇蓝. 血浆基质在口腔种植水平骨增量中的应用[J]. 口腔疾病防治, 2022, 30 (3): 153- 159.
|
| 20 |
doi: 10.12998/wjcc.v11.i11.2396 |
| 21 |
doi: 10.1186/s12903-020-1023-y |
| 22 |
张玉峰, 张晓欣. 血浆基质在牙槽嵴保存术中的应用[J]. 口腔疾病防治, 2024, 32 (3): 161- 168.
|
| 23 |
|
| 24 |
doi: 10.1111/prd.12609 |
| 25 |
王宇蓝, 曾浩, 夏婷, 等. 骨致密化技术联合血浆基质在穿牙槽嵴上颌窦底提升中的应用[J]. 中国口腔种植学杂志, 2025, 30 (2): 106- 110.
|
| 26 |
张晓欣, 张玉峰. 上颌窦底骨量不足新分类及血浆基质治疗策略[J]. 口腔生物医学, 2021, 12 (4): 215- 218.
|
| 27 |
doi: 10.1007/s00784-025-06198-4 |
| 28 |
doi: 10.1111/clr.14053 |
| 29 |
doi: 10.1186/s12903-023-03228-z |
| 30 |
doi: 10.1002/cap.10202 |
| 31 |
doi: 10.12998/wjcc.v9.i4.960 |
| 32 |
doi: 10.11607/prd.2505 |
| 33 |
doi: 10.1111/jre.12568 |
| 34 |
doi: 10.1016/j.joms.2020.02.019 |
| 35 |
doi: 10.1111/cid.12661 |
| 36 |
|
| 37 |
doi: 10.1590/1678-7757-2023-0294 |
| 38 |
doi: 10.1088/1748-605X/acbad5 |
| 39 |
doi: 10.1007/s00784-022-04510-0 |
| 40 |
|
| 41 |
张玉峰. 数字化骨块在骨增量中的应用[J]. 中华口腔医学杂志, 2023, 58 (4): 312- 317.
|
| [1] | 于子杨, 郭厚佐, 蒋析, 韩玮华, 林野. 穿颧种植体上颌窦段成骨的影像学研究[J]. 北京大学学报(医学版), 2025, 57(5): 967-974. |
| [2] | 王鹃, 邱立新, 尉华杰. 下颌磨牙穿龈形态设计对种植体周围软组织影响的随机对照临床研究[J]. 北京大学学报(医学版), 2025, 57(1): 65-72. |
| [3] | 王聪伟,高敏,于尧,章文博,彭歆. 游离腓骨瓣修复下颌骨缺损术后义齿修复的临床分析[J]. 北京大学学报(医学版), 2024, 56(1): 66-73. |
| [4] | 丁茜,李文锦,孙丰博,谷景华,林元华,张磊. 表面处理对氧化钇和氧化镁稳定的氧化锆种植体晶相及断裂强度的影响[J]. 北京大学学报(医学版), 2023, 55(4): 721-728. |
| [5] | 孙菲,刘建,李思琪,危伊萍,胡文杰,王翠. 种植体黏膜下微生物在健康种植体和种植体周炎中的构成与差异:一项横断面研究[J]. 北京大学学报(医学版), 2023, 55(1): 30-37. |
| [6] | 梁峰,吴敏节,邹立东. 后牙区单牙种植修复5年后的临床修复疗效观察[J]. 北京大学学报(医学版), 2021, 53(5): 970-976. |
| [7] | 释栋,曹婕,戴世爱,孟焕新. 植体周炎再生治疗短期疗效观察[J]. 北京大学学报(医学版), 2020, 52(1): 58-63. |
| [8] | 林春平,卢松鹤,朱浚鑫,胡洪成,岳兆国,唐志辉. 个性化根形种植体的螺纹形态对周围牙槽骨应力分布影响的三维有限元分析[J]. 北京大学学报(医学版), 2019, 51(6): 1130-1137. |
| [9] | 刘潇倩,陈秋雯,冯海兰,王兵,屈健,孙振,衡墨迪,潘韶霞. 无牙颌患者locator附着体种植覆盖义齿修复后口腔卫生维护的纵向研究[J]. 北京大学学报(医学版), 2019, 51(1): 136-144. |
| [10] | 吴敏节,邹立东,梁峰. 上前牙即刻种植即刻修复负载3年后软、硬组织变化的临床观察[J]. 北京大学学报(医学版), 2018, 50(4): 694-699. |
| [11] | 刘婧寅,陈飞,葛严军,魏菱,潘韶霞,冯海兰. 选择性激光熔化种植体对早期骨矿化沉积率的影响[J]. 北京大学学报(医学版), 2018, 50(1): 117-122. |
| [12] | 梁乃文,石磊,黄颖,邓旭亮. 不同形貌纯钛表面对人脐静脉内皮细胞生物学行为的影响[J]. 北京大学学报(医学版), 2017, 49(1): 43-048. |
| [13] | 李贝贝, 林野, 崔宏燕, 郝强, 胥加斌, 邸萍. 碳纤维增强“All-on-4”即刻修复体的临床评价[J]. 北京大学学报(医学版), 2016, 48(1): 133-137. |
| [14] | 崔宏燕, 邸萍, 李健慧, 林野, 刘蓉蓉. 电火花蚀刻技术在种植修复体制作中的应用[J]. 北京大学学报(医学版), 2015, 47(2): 336-339. |
| [15] | 韩劼, 陈智滨, 李玮, 孟焕新. 早期愈合阶段牙种植体周沟液骨代谢相关因子的检测和种植体稳定性共振频率分析[J]. 北京大学学报(医学版), 2015, 47(1): 37-41. |
|
||