北京大学学报(医学版) ›› 2018, Vol. 50 ›› Issue (6): 1009-1013. doi: 10.19723/j.issn.1671-167X.2018.06.012
多学科协作对神经精神狼疮磁共振成像特点的分类
常军英1,郑梅2,刘颖3,刘蕊4,张警丰4,邓晓莉4,△( )
)
- 1. 邯郸市中医院风湿免疫科, 河北邯郸 056001
2. 北京大学第三医院神经内科, 北京 100191
3. 北京大学第三医院放射科, 北京 100191
4. 北京大学第三医院风湿免疫科, 北京 100191
Multidisciplinary classification of magnetic resonance imaging features of neuropsychiatric lupus
Jun-ying CHANG1,Mei ZHENG2,Ying LIU3,Rui LIU4,Jing-feng ZHANG4,Xiao-li DENG4,△( )
)
- 1. Department of Rheumatology and Immunology,Handan Hospital of Traditional Chinese Medicine, Handan 056001, Hebei, China
2. Department of Neurology
3. Department of Radiology
4. Department of Rheumatology and Immunology, Peking University Third Hospital, Beijing 100191, China
摘要:
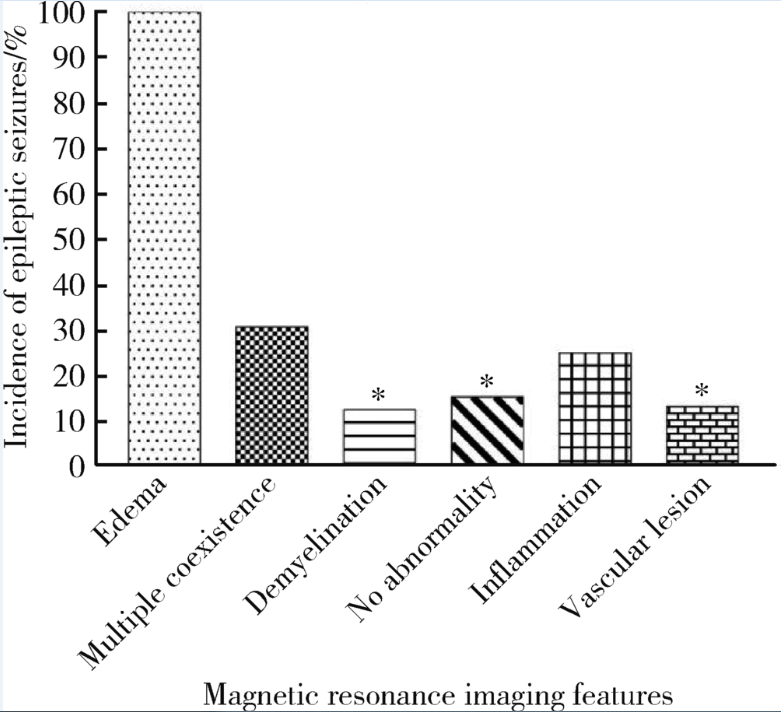
目的: 探讨神经精神狼疮(neuropsychiatric lupus,NPSLE)的头颅磁共振成像(magnetic resonance imaging,MRI)表现特点与临床的相关性。方法: 回顾性分析2006年1月—2016年10月北京大学第三医院收治的65例NPSLE患者头颅MRI表现和临床资料,由风湿免疫科、神经内科以及放射科医生对其头颅MRI表现进行综合分类,分析头颅MRI表现与临床表现的相关性。结果: 65例NPSLE患者头颅MRI表现特点被分为6类:脑白质脱髓鞘改变16例(25%)、血管病变15例(23%)[包括大血管病4例(6%)、小血管病11例(17%)]、炎症4例(6%)、水肿4例(6%)、多种病变共存13例(20%)、无异常13例(20%)。除4例头颅MRI表现为水肿患者的临床表现只有癫痫大发作外,其他患者临床表现复杂多样,包括癫痫大发作、狼疮样头痛、精神症状、视物模糊、周围神经病变和意识障碍。头颅MRI表现为水肿的患者癫痫大发作发生率显著高于其他5类MRI表现患者,且对于治疗反应时间最短,临床症状缓解最快。结论: 多学科协作将NPSLE患者头颅MRI表现分成6类,该分类方法有助于临床医生预估并在早期干预可能出现的神经精神症状,从而指导临床治疗。
中图分类号:
- R593.24
| [1] |
Ainiala H, Loukkola J, Peltola J , et al. The prevalence of neuropsychiatric syndromes in systemic lupus erythematosus[J]. Neurology, 2001,57(3):496-500.
doi: 10.1212/WNL.58.12.1867 pmid: 12084902 |
| [2] |
Brey RL, Holliday SL, Saklad AR , et al. Neuropsychiatric syndromes in lupus: prevalence using standardized definitions[J]. Neurology, 2002,58(8):1214-1220.
doi: 10.1212/WNL.58.8.1214 |
| [3] |
Jonsen A, Bengtsson AA, Nived O , et al. Outcome of neuropsychiatric systemic lupus erythematosus within a defined Swedish population: increased morbidity but low mortality[J]. Rheumatology (Oxford), 2002,41(11):1308-1312.
doi: 10.1097/00003072-199902000-00007 pmid: 12422005 |
| [4] | Sanna G, Bertolaccini ML, Cuadrado MJ , et al. Neuropsychiatric manifestations in systemic lupus erythematosus: prevalence and association with antiphospholipid antibodies[J]. J Rheumatol, 2003,30(5):985-992. |
| [5] |
Afeltra A, Garzia P, Mitterhofer AP , et al. Neuropsychiatric lupus syndromes: relationship with antiphospholipid antibodies[J]. Neurology, 2003,61(1):108-110.
doi: 10.1212/01.WNL.0000058904.94330.A7 pmid: 12847168 |
| [6] |
Hanly JG, Mccurdy G, Fougere L , et al. Neuropsychiatric events in systemic lupus erythematosus: attribution and clinical significance[J]. J Rheumatol, 2004,31(111):2156-2162.
doi: 10.1016/j.jbspin.2004.07.009 pmid: 15517627 |
| [7] |
Mikdashi J, Handwerger B . Predictors of neuropsychiatric damage in systemic lupus erythematosus: data from the Maryland lupus cohort[J]. Rheumatology, 2004,43(12):1555-1560.
doi: 10.1093/rheumatology/keh384 pmid: 15342927 |
| [8] |
Zhou HQ, Zhang FC, Tian XP , et al. Clinical features and outcome of neuropsychiatric lupus in Chinese: analysis of 240 hospitalized patients[J]. Lupus, 2008,17(2):93-99.
doi: 10.1177/0961203307085671 pmid: 18250131 |
| [9] |
Bultink IE, Turkstra F, Dijkmans BA , et al. High prevalence of unemployment in patients with systemic lupus erythematosus: association with organ damage and health-related quality of life[J]. J Rheumatol, 2008,35(6):1053-1057.
doi: 10.1097/RHU.0b013e3181778cb5 pmid: 18381792 |
| [10] |
Hanly JG, Su L, Farewell V , et al. Prospective study of neuropsychiatric events in systemic lupus erythematosus[J]. J Rheumatol, 2009,36(71):1449-1459.
doi: 10.3899/jrheum.081133 pmid: 19447937 |
| [11] |
Briani C, Lucchetta M, Ghirardello A , et al. Neurolupus is associated with anti-ribosomal P protein antibodies: an inception cohort study[J]. J Autoimmun, 2009,32(2):79-84.
doi: 10.1016/j.jaut.2008.12.002 pmid: 19171463 |
| [12] |
Gonzalez LA, Pons-Estel GJ, Zhang J , et al. Time to neuropsychiatric damage occurrence in LUMINA: a multi-ethnic lupus cohort[J]. Lupus, 2009,18(9):822-830.
doi: 10.1177/0961203309104392 |
| [13] |
The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes[J]. Arthritis Rheum, 1999,42(4):599-608.
doi: 10.1002/(ISSN)1529-0131 |
| [14] |
Benseler SM, Silverman ED . Neuropsychiatric involvement in pe-diatric systemic lupus erythematosus[J]. Lupus, 2007,16(8):564-571.
doi: 10.1177/0961203307078971 pmid: 17711889 |
| [15] |
Ainiala H, Dastidar P, Loukkola J , et al. Cerebral MRI abnormalities and their association with neuropsychiatric manifestations in SLE: a population-based study[J]. Scand J Rheumatol, 2005,34(5):376-382.
doi: 10.1080/03009740510026643 pmid: 16234185 |
| [16] |
Peterson PL, Axford JS, Isenberg D . Imaging in CNS lupus[J]. Best Pract Res Clin Rheumatol, 2005,19(5):727-739.
doi: 10.1016/j.berh.2005.04.001 |
| [17] |
Hanly JG, Walsh NM, Sangalang V . Brain pathology in systemic lupus erythematosus[J]. J Rheumatol, 1992,19(5):732-741.
pmid: 1613703 |
| [18] |
Kiss E, Shoenfeld Y . Are anti-ribosomal P protein antibodies relevant in systemic lupus erythematosus?[J]. Clin Rev Allergy Immunol, 2007,32(1):37-46.
doi: 10.1007/BF02686080 pmid: 17426359 |
| [19] |
王元, 顾越英, 鲍春德 . 神经精神狼疮的诊断和治疗[J]. 中华风湿病学杂志, 2004,8(4):230-233.
doi: 10.3760/j:issn:1007-7480.2004.04.010 |
| [20] |
Govoni M, Castellino G, Padovan M , et al. Recent advances and perspective in neuroimaging in neuropsychiatric systemic lupus erythematosus[J]. Lupus, 2004,13(3):149-158.
doi: 10.1191/0961203304lu1000rr |
| [21] | 杨燕, 刘秀梅, 孙美珍 . 神经精神性狼疮的临床表现和MRI特点分析[J]. 中国神经免疫学和神经病学杂志, 2011,18(4):287-289. |
| [22] |
Sarbu N, Alobeidi F, Toledano P , et al. Brain abnormalities in newly diagnosed neuropsychiatric lupus: systematic MRI approach and correlation with clinical and laboratory data in a large multicenter cohort[J]. Autoimmun Rev, 2015,14(2):153-159.
doi: 10.1016/j.autrev.2014.11.001 pmid: 25461835 |
| [23] |
Luyendijk J, Steens SC, Ouwendijk WJ , et al. Neuropsychiatric systemic lupus erythematosus: lessons learned from magnetic resonance imaging[J]. Arthritis Rheum, 2011,63(3):722-732.
doi: 10.1002/art.30157 pmid: 21360502 |
| [1] | 邢念增,王明帅,杨飞亚,尹路,韩苏军. 前列腺免活检创新理念的临床实践及其应用前景[J]. 北京大学学报(医学版), 2024, 56(4): 565-566. |
| [2] | 田宇轩,阮明健,刘毅,李德润,吴静云,沈棋,范宇,金杰. 双参数MRI改良PI-RADS评分4分和5分病灶的最大径对临床有意义前列腺癌的预测效果[J]. 北京大学学报(医学版), 2024, 56(4): 567-574. |
| [3] | 刘毅,袁昌巍,吴静云,沈棋,肖江喜,赵峥,王霄英,李学松,何志嵩,周利群. 靶向穿刺+6针系统穿刺对PI-RADS 5分患者的前列腺癌诊断效能[J]. 北京大学学报(医学版), 2023, 55(5): 812-817. |
| [4] | 袁昌巍,李德润,李志华,刘毅,山刚志,李学松,周利群. 多参数磁共振成像中动态对比增强状态在诊断PI-RADS 4分前列腺癌中的应用[J]. 北京大学学报(医学版), 2023, 55(5): 838-842. |
| [5] | 刘颖,霍然,徐慧敏,王筝,王涛,袁慧书. 磁共振血管壁成像评估颈动脉中重度狭窄患者斑块特征与脑血流灌注的相关性[J]. 北京大学学报(医学版), 2023, 55(4): 646-651. |
| [6] | 傅强,高冠英,徐雁,林卓华,孙由静,崔立刚. 无症状髋关节前上盂唇撕裂超声与磁共振检查的对比研究[J]. 北京大学学报(医学版), 2023, 55(4): 665-669. |
| [7] | 叶珊,金萍萍,张楠,邬海博,石林,赵强,杨坤,袁慧书,樊东升. 肌萎缩侧索硬化患者认知功能改变与脑皮层厚度分析[J]. 北京大学学报(医学版), 2022, 54(6): 1158-1162. |
| [8] | 蔡颖,万巧琴,蔡宪杰,高亚娟,韩鸿宾. 光生物调节加速脑组织间液引流及其机制[J]. 北京大学学报(医学版), 2022, 54(5): 1000-1005. |
| [9] | 王书磊,高阳旭,张宏武,杨海波,李辉,李宇,沈笠雪,姚红新. 儿童基底节区生殖细胞瘤30例临床分析[J]. 北京大学学报(医学版), 2022, 54(2): 222-226. |
| [10] | 张帆,陈曲,郝一昌,颜野,刘承,黄毅,马潞林. 术前及术后膜性尿道长度与腹腔镜根治性前列腺切除术后控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2022, 54(2): 299-303. |
| [11] | 吴一凡,张晓圆,任爽,玉应香,常翠青. 基于磁共振的青年男性股四头肌的测量和评估[J]. 北京大学学报(医学版), 2021, 53(5): 843-849. |
| [12] | 盛荟,梁磊,周童亮,贾彦兴,王彤,袁兰,韩鸿宾. 光磁双模态探针钆-[4,7-双-羧甲基-10-(2-荧光素硫脲乙基)-1,4,7,10-四氮杂环十二烷-1-基]-乙酸络合物合成方法的改进[J]. 北京大学学报(医学版), 2020, 52(5): 959-963. |
| [13] | 赵世明,杨铁军,许春苗,郭孝峰,马永康,陈学军,李祥,何朝宏. 3.0T磁共振成像在接受过经尿道膀胱肿瘤切除术膀胱癌中诊断肌层浸润的应用[J]. 北京大学学报(医学版), 2020, 52(4): 701-704. |
| [14] | 宋宇,韩鸿宾,杨军,王艾博,和清源,李媛媛,赵国梅,高亚娟,王睿,韩易兴,刘爱连,宋清伟. 脑对流增强给药对老年大鼠脑细胞外间隙微观结构的影响[J]. 北京大学学报(医学版), 2020, 52(2): 362-367. |
| [15] | 吴静云,米悦,刘水,姚林,唐琦,何志嵩,王霄英. MRI对肾细胞癌静脉瘤栓侵犯下腔静脉壁的术前评估[J]. 北京大学学报(医学版), 2019, 51(4): 673-677. |
|
||