北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (1): 167-174. doi: 10.19723/j.issn.1671-167X.2021.01.025
后路短节段跨伤椎椎弓根螺钉固定治疗胸腰段爆裂骨折术后再发后凸的危险因素
侯国进,周方( ),田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮,张雅文
),田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮,张雅文
- 北京大学第三医院骨科, 北京 100191
Risk factors of recurrent kyphosis in thoracolumbar burst fracture patients treated by short segmental pedicle screw fixation
HOU Guo-jin,ZHOU Fang( ),TIAN Yun,JI Hong-quan,ZHANG Zhi-shan,GUO Yan,LV Yang,YANG Zhong-wei,ZHANG Ya-wen
),TIAN Yun,JI Hong-quan,ZHANG Zhi-shan,GUO Yan,LV Yang,YANG Zhong-wei,ZHANG Ya-wen
- Department of Orthopaedic Surgery, Peking University Third Hospital, Beijing 100191, China
摘要:
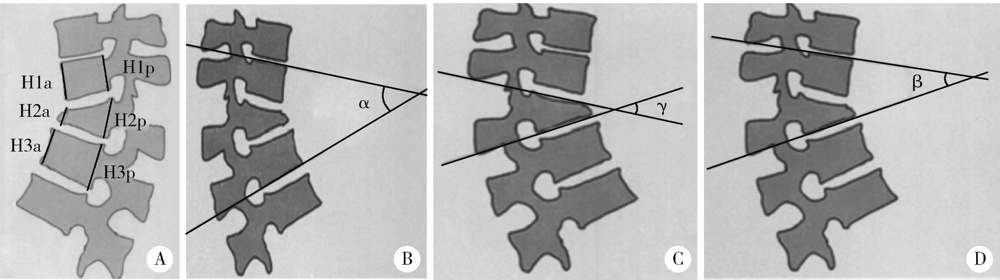
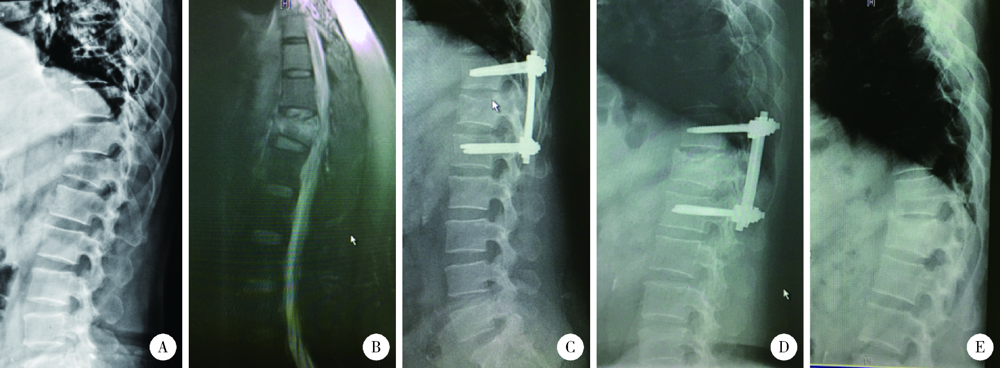
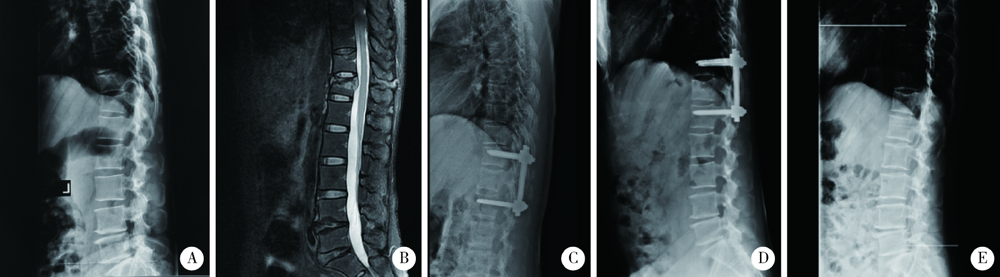
目的: 探索后路短节段跨伤椎椎弓根螺钉固定治疗胸腰段爆裂骨折内固定物取出术后再发后凸的危险因素。方法: 回顾性分析北京大学第三医院2010年1月至2017年12月诊治的无神经功能损害的单节段胸腰段爆裂骨折患者的临床资料,共有144例患者纳入该研究。所有患者均采用跨伤椎椎弓根螺钉固定,其中男性74例,女性70例;平均年龄(39.1±13.2)岁。伤椎分布在T12(42例)、L1(72例)和L2(30例),骨折类型为A3(90例)、B1(25例)和B2(29例)。根据取出内固定物后末次随访矫正度丢失是否>5°,将患者分为再发后凸组和无再发后凸组,再发后凸组共纳入92例,无再发后凸组共纳入52例。利用SPSS 26.0软件进行单因素组间比较及Logistic回归分析。结果: 平均随访时间28(20~113)个月,分别于术前、术后3 d、术后12个月及末次随访对患者影像学指标进行测量并对比分析。伤椎前缘高度、局部后凸角、伤椎楔形角、Gardner畸形等指标术后较术前均有明显改善(P<0.05),但在术后1年随访时均有不同程度的丢失;伤椎前缘高度和伤椎楔形角不再因取钉发生变化,而局部后凸角和Gardner畸形在取钉术后仍出现后凸加重(P<0.05);伤椎上、下椎间盘高度随访过程中出现不同程度的塌陷。单因素分析可见,再发后凸组和无再发后凸组患者的性别、年龄(36.9岁 vs. 43.0岁)、上位椎间盘损伤与否、CT值(174 vs. 160)、术前节段后凸角(16.6° vs. 13.3°)、术前伤椎楔形角(16.7° vs. 13.6°)、术前Gardner畸形(19.1° vs. 15.2°)及术前椎体前缘的高度比(0.65 vs. 0.71)差异具有统计学意义(P<0.05)。Logistics回归分析提示,男性(OR: 2.88,95%CI:1.196~6.933)、上位椎间盘损伤(OR: 2.962,95%CI:1.062~8.258)及术前伤椎楔形角是短节段跨伤椎椎弓根螺钉固定治疗胸腰段爆裂骨折取出内固定物后再发后凸的危险因素(P<0.05)。结论: 胸腰段骨折患者经后路短节段跨伤椎内固定能取得满意的术后即刻效果,但随访过程中可能会发生一定程度的矫正角度丢失,男性、上位椎间盘损伤及术前伤椎楔形角是内固定物取出后再发后凸的危险因素。
中图分类号:
- R683.2
| [1] |
Wood KB, Bohn D, Mehbod A. Anterior versus posterior treatment of stable thoracolumbar burst fractures without neurologic deficit: A prospective, randomized study[J]. J Spinal Disord Tech, 2005,18:S15-S23.
doi: 10.1097/01.bsd.0000132287.65702.8a pmid: 15699801 |
| [2] |
Rajasekaran S, Kanna RM, Shetty AP. Management of thoracolumbar spine trauma: An overview[J]. Indian J Orthop, 2015,49(1):72-82.
doi: 10.4103/0019-5413.143914 pmid: 25593358 |
| [3] | 伍骥, 郑超, 黄蓉蓉. 重新认识胸腰段脊柱骨折的诊断和治疗[J]. 中国骨与关节杂志, 2016,5(6):401-404. |
| [4] |
Pellise F, Barastegui D, Hernandez-Fernandez A, et al. Viability and long-term survival of short-segment posterior fixation in thoracolumbar burst fractures[J]. Spine J, 2015,15(8):1796-1803.
doi: 10.1016/j.spinee.2014.03.012 pmid: 24642054 |
| [5] |
Lee MC, Solomito M, Patel A. Supine magnetic resonance imaging Cobb measurements for idiopathic scoliosis are linearly related to measurements from standing plain radiographs[J]. Spine(Phila Pa 1976), 2013,38(11):E656-E661.
doi: 10.1097/BRS.0b013e31828d255d |
| [6] |
Wang XY, Dai LY, Xu HZ, et al. Kyphosis recurrence after posterior short-segment fixation in thoracolumbar burst fractures[J]. J Neurosurg Spine, 2008,8(3):246-254.
doi: 10.3171/SPI/2008/8/3/246 pmid: 18312076 |
| [7] |
Zou D, Li WS, Deng C, et al. The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases[J]. Eur Spine J, 2019,28(8):1758-1766.
doi: 10.1007/s00586-018-5776-9 pmid: 30306332 |
| [8] |
Sander AL, Laurer H, Lehnert T, et al. A clinically useful classification of traumatic intervertebral disk lesions[J]. AJR Am J Roentgenol, 2013,200(3):618-623.
doi: 10.2214/AJR.12.8748 pmid: 23436852 |
| [9] |
McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures[J]. Spine, 1994,19(15):1741-1744.
doi: 10.1097/00007632-199408000-00014 pmid: 7973969 |
| [10] |
Roy-Camille R, Saillant G, Mazel C. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates[J]. Orthop Clin North Am, 1986,17(1):147-159.
pmid: 3945476 |
| [11] |
Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation[J]. Neurosurgery, 2003,53(6):1354-1361.
doi: 10.1227/01.neu.0000093200.74828.2f pmid: 14633301 |
| [12] |
Kim JY, Ryu DS, Paik HK, et al. Paraspinal muscle, facet joint, and disc problems: Risk factors for adjacent segment degeneration after lumbar fusion[J]. Spine J, 2016,16(7):867-875.
doi: 10.1016/j.spinee.2016.03.010 pmid: 26970600 |
| [13] |
Furderer S, Wenda K, Thiem N, et al. Traumatic intervertebral disc lesion: Magnetic resonance imaging as a criterion for or against intervertebral fusion[J]. Eur Spine J, 2001,10(2):154-163.
doi: 10.1007/s005860000238 pmid: 11345638 |
| [14] |
Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures: A five to seven years prospective randomized study[J]. J Bone Joint Surg Am, 2009,91(5):1033-1041.
doi: 10.2106/JBJS.H.00510 pmid: 19411450 |
| [15] |
Kerttula LI, Serlo WS, Tervonen OA, et al. Post-traumatic findings of the spine after earlier vertebral fracture in young patients: clinical and MRI study[J]. Spine, 2000,25(9):1104-1108.
doi: 10.1097/00007632-200005010-00011 pmid: 10788855 |
| [16] |
Chen JX, Xu DL, Sheng SR, et al. Risk factors of kyphosis recurrence after implant removal in thoracolumbar burst fractures following posterior short-segment fixation[J]. Int Orthop, 2016,40(6):1253-1260.
doi: 10.1007/s00264-016-3180-9 pmid: 27116190 |
| [17] |
Alanay A, Acaroglu E, Yazici M, et al. Short-segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure?[J]. Spine, 2001,26(2):213-217.
doi: 10.1097/00007632-200101150-00017 pmid: 11154543 |
| [18] |
Jun DS, Shin WJ, An BK, et al. The relationship between the progression of kyphosis in stable thoracolumbar fractures and magnetic resonance imaging findings[J]. Asian Spine J, 2015,9(2):170-177.
doi: 10.4184/asj.2015.9.2.170 pmid: 25901226 |
| [19] |
Mahar A, Kim C, Wedemeyer M, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture[J]. Spine, 2007,32(14):1503-1507.
doi: 10.1097/BRS.0b013e318067dd24 pmid: 17572619 |
| [20] | 魏富鑫, 刘少喻, 赵卫东, 等. 胸腰椎爆裂性骨折伤椎固定的生物力学研究[J]. 中华创伤骨科杂志, 2006,8(9):857-860. |
| [21] |
Li K, Zhang W, Liu D, et al. Pedicle screw fixation combined with intermediate screw at the fracture level for treatment of thoracolumbar fractures: A meta-analysis[J]. Medicine (Baltimore), 2016,95(33):e4574.
doi: 10.1097/MD.0000000000004574 |
| [22] |
Rajasekaran S, Maheswaran A, Aiyer SN, et al. Prediction of posterior ligamentous complex injury in thoracolumbar fractures using non-MRI imaging techniques[J]. Int Orthop, 2016,40(6):1075-1081.
doi: 10.1007/s00264-016-3151-1 pmid: 26983409 |
| [23] | 唐一村, 林本丹, 林慰光, 等. X线片和CT影像对胸腰椎后方韧带复合体损伤的诊断意义[J]. 中国脊柱脊髓杂志, 2016,26(9):801-806. |
| [24] |
Machino M, Yukawa Y, Ito K, et al. Posterior ligamentous complex injuries are related to fracture severity and neurological damage in patients with acute thoracic and lumbar burst fractures[J]. Yonsei Med J, 2013,54(4):1020-1025.
doi: 10.3349/ymj.2013.54.4.1020 pmid: 23709440 |
| [25] |
McLain RF. The biomechanics of long versus short fixation for thoracolumbar spine fractures[J]. Spine(Phila Pa 1976), 2006,31(11 Suppl):S70-S79.
doi: 10.1097/01.brs.0000218221.47230.dd |
| [26] | 张阳, 张志成, 李放, 等. 后方韧带复合体损伤在胸腰段骨折患者评估中的意义[J]. 中国骨与关节杂志, 2016,5(6):425-428. |
| [27] | 张亚军, 方礼明, 张军, 等. 经椎旁肌间隙短节段椎弓根钉固定治疗伴后方韧带复合体损伤的胸腰椎骨折[J]. 中华创伤骨科杂志, 2013,15(12):1049-1053. |
| [28] |
何海潮, 吕晓强, 张永进. 短节段经皮微创与传统椎弓根螺钉内固定治疗伴后方韧带复合体损伤的胸腰椎骨折的比较[J]. 中国骨伤, 2016,29(4):329-334.
doi: 10.3969/j.issn.1003-0034.2016.04.009 |
| [29] |
Parker JW, Lane JR, Karaikovic EE, et al. Successful shortsegment instrumentation and fusion for thoracolumbar spine fractures: A consecutive 41/ 2-year series[J]. Spine, 2000,25(9):1157-1170.
doi: 10.1097/00007632-200005010-00018 pmid: 10788862 |
| [30] |
Rihn JA, Anderson DT, Harris E, et al. A review of the TLICS system: A novel, user-friendly thoracolumbar trauma classification system[J]. Acta Orthop, 2008,79(4):461-466.
doi: 10.1080/17453670710015436 pmid: 18766477 |
| [31] |
Kaul R, Chhabra HS, Vaccaro AR, et al. Reliability assessment of AOSpine thoracolumbar spine injury classification system and thoracolumbar injury classification and severity score (TLICS) for thoracolumbar spine injuries: results of a multicentre study[J]. Eur Spine J, 2017,26(5):1470-1476.
doi: 10.1007/s00586-016-4663-5 pmid: 27334493 |
| [1] | 汪琪伟, 包鹏宇, 洪士皓, 杨昕, 王宇, 曹永平. 改良股骨颈截骨术在伴严重屈曲畸形强直性脊柱炎患者手术治疗过程中的疗效[J]. 北京大学学报(医学版), 2024, 56(5): 884-889. |
| [2] | 王军, 姚兰, 张宁, 索利斌, 李红培, 魏越, 查鹏, 梁正, 刘鲲鹏. 单侧胸椎旁阻滞对实施双腔气管插管患者血流动力学和意识水平的影响[J]. 北京大学学报(医学版), 2024, 56(5): 890-895. |
| [3] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [4] | 黄教悌,胡菁,韩博. 治疗相关神经内分泌前列腺癌机制研究与靶向治疗新进展[J]. 北京大学学报(医学版), 2024, 56(4): 557-561. |
| [5] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [6] | 陈延,李况蒙,洪锴,张树栋,程建星,郑仲杰,唐文豪,赵连明,张海涛,姜辉,林浩成. 阴茎海绵体注射试验对阴茎血管功能影响的回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 680-686. |
| [7] | 庞博,郭桐君,陈曦,郭华棋,石嘉章,陈娟,王欣梅,李耀妍,单安琪,余恒意,黄婧,汤乃军,王艳,郭新彪,李国星,吴少伟. 天津与上海35岁以上人群氮氧化物个体暴露水平及其影响因素[J]. 北京大学学报(医学版), 2024, 56(4): 700-707. |
| [8] | 和静,房中则,杨颖,刘静,马文瑶,霍勇,高炜,武阳丰,谢高强. 血浆中脂质代谢分子与颈动脉粥样硬化斑块、传统心血管危险因素及膳食因素的关系[J]. 北京大学学报(医学版), 2024, 56(4): 722-728. |
| [9] | 蔡珊,张依航,陈子玥,刘云飞,党佳佳,师嫡,李佳欣,黄天彧,马军,宋逸. 北京市中小学生身体活动时间现状及影响因素的路径[J]. 北京大学学报(医学版), 2024, 56(3): 403-410. |
| [10] | 张祖洪,陈天娇,马军. 中小学生青春发动时相与心血管代谢危险因素的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 418-423. |
| [11] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [12] | 朱金荣,赵亚娜,黄巍,赵微微,王悦,王松,苏春燕. 感染新型冠状病毒的血液透析患者的临床特征[J]. 北京大学学报(医学版), 2024, 56(2): 267-272. |
| [13] | 赖展鸿,李嘉辰,贠泽霖,张永刚,张昊,邢晓燕,邵苗,金月波,王乃迪,李依敏,李玉慧,栗占国. 特发性炎性肌病完全临床应答相关因素的单中心真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 284-292. |
| [14] | 司筱芊,赵秀娟,朱凤雪,王天兵. 创伤出血性休克后急性呼吸窘迫综合征的危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 307-312. |
| [15] | 李洋洋,侯林,马紫君,黄山雅美,刘捷,曾超美,秦炯. 孕期因素与婴儿牛奶蛋白过敏的关系[J]. 北京大学学报(医学版), 2024, 56(1): 144-149. |
|
||