北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 896-901. doi: 10.19723/j.issn.1671-167X.2021.05.014
一种结合线袢固定的关节镜下“嵌入式”喙突移位术:手术技术及术后影像学分析
- 1.北京大学第三医院运动医学科,北京大学运动医学研究所,运动医学关节伤病北京市重点实验室,北京 100191
2.北京大学第三医院放射科,北京 100191
An arthroscopic “inlay” Bristow procedure with suture button fixation: Surgical technique and radiology evaluation
SHAO Zhen-xing1,SONG Qing-fa1,ZHAO Yu-qing2,CUI Guo-qing1,△( )
)
- 1. Department of Sports Medicine, Peking University Third Hospital, Institute of Sports Medicine of Peking University, Beijing Key Laboratory of Sports Injuries, Beijing 100191, China
2. Department of Radiology, Peking University Third Hospital, Beijing 100191, China
摘要:
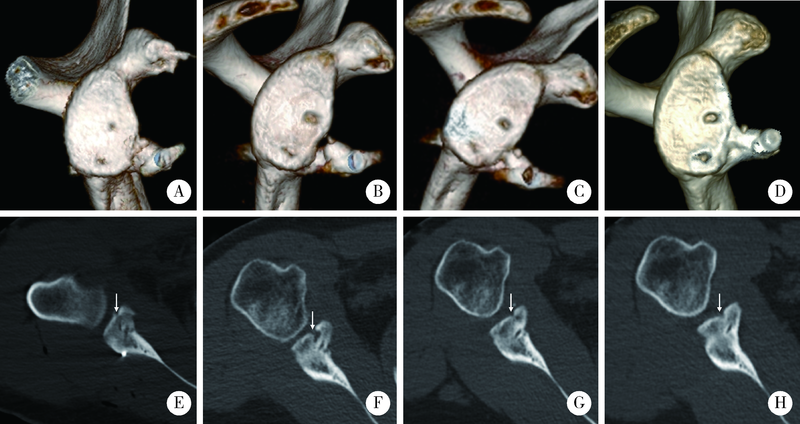
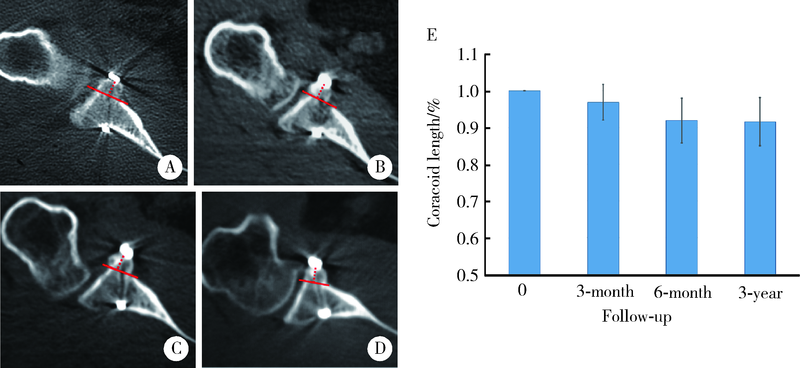
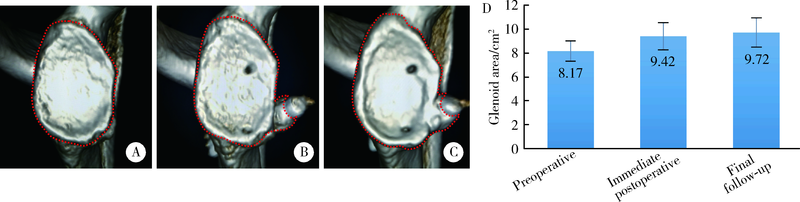
目的: 探讨一种基于榫卯结构的改良关节镜下“嵌入式”喙突移位术结合线袢固定的手术方法,并对其术后影像学结果进行分析。方法: 2015年6月至2016年6月共有56例复发性肩关节前向不稳患者接受了结合线袢固定的关节镜下“嵌入式”喙突移位手术,所有的患者均在术前及术后即刻、3个月、6个月、3年分别进行头盂分离的三维CT评估,评估内容包括骨块位置、骨愈合以及骨重塑情况,并对术后并发症进行随访和记录。结果: 56例患者平均随访时间为(36.1±3.7)个月。在三维CT扫描En-Face相上喙突骨块中点位于4点钟左右位置(123.8°±12.3°), CT轴位上喙突骨块位置优良率达到95%(53/56), 3年随访喙突骨块愈合率达到96.4%(54/56)。术后3个月、6个月及3年喙突骨块的长度分别为术后即刻长度的96.9%±4.9%、91.9%±6.2%、91.6%±6.6%,移植喙突骨块在术后3个月时长度变化并不明显(t=2.12,P>0.05),而术后6个月时缩短较为明显(t=4.98,P<0.05), 然后随着时间的推移几乎保持不变(t=-0.75,P>0.05),在3年随访时所有移植的喙突骨块都保留了90%以上的初始长度。愈合的病例中未发现明显的骨块吸收;其中25例在CT上都观察到了明显的喙突骨块与关节盂之间的新生骨重塑,术后3年随访时关节盂面积平均为(9.72±1.22) cm2,较术后即刻的(9.42±1.11) cm2有显著增加(P<0.05);最终随访时,所有的病例在CT上均未发现骨性关节炎的发生。结论: 结合线袢固定的关节镜下“嵌入式”喙突移位手术用于治疗复发性肩关节前脱位,术后喙突骨块位置良好、骨愈合率满意。基于榫卯结构以及线袢固定的方法可以提高稳定性,并促进喙突骨块的术后愈合,同时又可以避免使用传统螺钉固定造成的骨溶解以及螺钉植入相关的并发症。更重要的是,术后喙突骨块和关节盂之间的骨重塑显著增加了关节盂面积,有利于恢复肩关节的前向稳定性。
中图分类号:
- R684.73
| [1] |
Cowling PD, Akhtar MA, Liow RY. What is a Bristow-Latarjet procedure? A review of the described operative techniques and outcomes [J]. Bone Joint J, 2016, 98-B(9):1208-1214.
doi: 10.1302/0301-620X.98B9.37948 pmid: 27587522 |
| [2] |
Bhatia S, Frank RM, Ghodadra NS, et al. The outcomes and surgical techniques of the latarjet procedure [J]. Arthroscopy, 2014, 30(2):227-235.
doi: 10.1016/j.arthro.2013.10.013 |
| [3] |
Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: A systema-tic review [J]. J Shoulder Elbow Surg, 2013, 22(2):286-292.
doi: 10.1016/j.jse.2012.09.009 pmid: 23352473 |
| [4] |
van der Linde JA, van Kampen DA, Terwee CB, et al. Long-term results after arthroscopic shoulder stabilization using suture anchors: An 8- to 10-year follow-up [J]. Am J Sports Med, 2011, 39(11):2396-2403.
doi: 10.1177/0363546511415657 pmid: 21803980 |
| [5] |
Casabianca L, Gerometta A, Massein A, et al. Graft position and fusion rate following arthroscopic Latarjet [J]. Knee Surg Sports Traumatol Arthrosc, 2016, 24(2):507-512.
doi: 10.1007/s00167-015-3551-6 |
| [6] |
Kany J, Flamand O, Grimberg J, et al. Arthroscopic Latarjet procedure: Is optimal positioning of the bone block and screws possible? A prospective computed tomography scan analysis [J]. J Shoulder Elbow Surg, 2016, 25(1):69-77.
doi: 10.1016/j.jse.2015.06.010 |
| [7] |
Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder [J]. J Bone Joint Surg Am, 1998, 80(6):841-852.
pmid: 9655102 |
| [8] |
Bessiere C, Trojani C, Pelegri C, et al. Coracoid bone block versus arthroscopic Bankart repair: A comparative paired study with 5-year follow-up [J]. Orthop Traumatol Surg Res, 2013, 99(2):123-130.
doi: 10.1016/j.otsr.2012.12.010 |
| [9] | Lafosse L, Lejeune E, Bouchard A, et al. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability [J]. Arthroscopy, 2007, 23(11):1241-1245. |
| [10] |
Boileau P, Gendre P, Baba M, et al. A guided surgical approach and novel fixation method for arthroscopic Latarjet [J]. J Shoulder Elbow Surg, 2016, 25(1):78-89.
doi: 10.1016/j.jse.2015.06.001 pmid: 26256014 |
| [11] |
Butt U, Charalambous CP. Complications associated with open coracoid transfer procedures for shoulder instability [J]. J Shoulder Elbow Surg, 2012, 21(8):1110-1119.
doi: 10.1016/j.jse.2012.02.008 |
| [12] |
Boileau P, Hardy MB, McClelland WB, et al. Arthroscopic posterior bone block procedure: A new technique using suture anchor fixation [J]. Arthrosc Tech, 2013, 2(4):473-477.
doi: 10.1016/j.eats.2013.07.004 pmid: 24892011 |
| [13] |
Boileau P, Saliken D, Gendre P, et al. Arthroscopic Latarjet: Suture-button fixation is a safe and reliable alternative to screw fixation [J]. Arthroscopy, 2019, 35(4):1050-1061.
doi: S0749-8063(18)31066-1 pmid: 30857907 |
| [14] |
Giles JW, Degen RM, Johnson JA, et al. The Bristow and Latarjet procedures: Why these techniques should not be considered synonymous [J]. J Bone Joint Surg A, 2014, 96(16):1340-1348.
doi: 10.2106/JBJS.M.00627 |
| [15] |
van der Linde JA, van Wijngaarden R, Somford MP, et al. The Bristow-Latarjet procedure, a historical note on a technique in comeback [J]. Knee Surg Sports Traumatol Arthrosc, 2016, 24(2):470-478.
doi: 10.1007/s00167-015-3704-7 |
| [16] |
Boileau P, Thelu CE, Mercier N, et al. Arthroscopic Bristow-Latarjet combined with bankart repair restores shoulder stability in patients with glenoid bone loss [J]. Clin Orthop Relat Res, 2014, 472(8):2413-2424.
doi: 10.1007/s11999-014-3691-x |
| [17] |
Shao Z, Song Q, Cheng X, et al. An arthroscopic “Inlay” Bristow procedure with suture button fixation for the treatment of recurrent anterior glenohumeral instability: 3-year follow-up [J]. Am J Sports Med, 2020, 48(11):2638-2649.
doi: 10.1177/0363546520943633 |
| [18] |
Nourissat G, Delaroche C, Bouillet B, et al. Optimization of bone-block positioning in the Bristow-Latarjet procedure: A biomechanical study [J]. Orthop Traumatol Surg Res, 2014, 100(5):509-513.
doi: 10.1016/j.otsr.2014.03.023 |
| [19] |
Hovelius L, Sandstrom B, Olofsson A, et al. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study Ⅲ): Long-term follow-up in 319 shoulders [J]. J Shoulder Elbow Surg, 2012, 21(5):647-660.
doi: 10.1016/j.jse.2011.03.020 pmid: 21719316 |
| [20] |
Kee YM, Kim JY, Kim HJ, et al. Fate of coracoid grafts after the Latarjet procedure: Will be analogous to the original glenoid by remodelling [J]. Knee Surg Sports Traumatol Arthrosc, 2018, 26(3):926-932.
doi: 10.1007/s00167-017-4808-z |
| [21] |
Samilson RL, Prieto V. Dislocation arthropathy of the shoulder [J]. J Bone Joint Surg, 1983, 65(4):456-460.
doi: 10.2106/00004623-198365040-00005 |
| [22] | Garcia JC, do Amaral FM, Belchior RJ, et al. Comparative systematic review of fixation methods of the coracoid and conjoined tendon in the anterior glenoid to treat anterior shoulder instability [J]. Orthop J Sports Med, 2019, 7(1):2325-2328. |
| [23] |
Xu J, Liu H, Lu W, et al. Modified arthroscopic Latarjet procedure: Suture-button fixation achieves excellent remodeling at 3-year follow-up [J]. Am J Sports Med, 2019, 48(1):39-47.
doi: 10.1177/0363546519887959 |
| [1] | 郑佳鹏,肖棋,邓辉云,吴清泉,翟文亮,林达生. 外侧半月板腘肌腱区损伤的关节镜下分型和处理[J]. 北京大学学报(医学版), 2021, 53(5): 891-895. |
| [2] | 侯宗辰,敖英芳,胡跃林,焦晨,郭秦炜,黄红拾,任爽,张思,谢兴,陈临新,赵峰,皮彦斌,李楠,江东. 慢性踝关节不稳患者足底压力特征及相关因素分析[J]. 北京大学学报(医学版), 2021, 53(2): 279-285. |
| [3] | 江东,胡跃林,焦晨,郭秦炜,谢兴,陈临新,赵峰,皮彦斌. 慢性踝关节不稳合并后踝撞击同期手术中长期疗效及影响因素分析[J]. 北京大学学报(医学版), 2019, 51(3): 505-509. |
| [4] | 张翠平,刘佩佩,傅强,高冠英,崔立刚,徐雁,王健全. 超声引导下髋关节药物注射在关节镜盂唇修复术后康复中的应用[J]. 北京大学学报(医学版), 2019, 51(2): 265-267. |
| [5] | 荣艳波,田光磊,陈山林. 深层桡尺远侧韧带对桡尺远侧关节稳定作用的生物力学研究[J]. 北京大学学报(医学版), 2017, 49(3): 518-521. |
| [6] | 张辉,刘心,洪雷,耿向苏,冯华. 全关节镜下腘肌腱重建与切开腘腓韧带重建治疗膝关节后外旋转不稳定的对比[J]. 北京大学学报(医学版), 2016, 48(2): 237-243. |
| [7] | 刘波,陈山林,朱瑾,王志新,杨辰,沈杰,田光磊. 腕关节镜辅助微创治疗月骨周围脱位[J]. 北京大学学报(医学版), 2016, 48(2): 234-236. |
| [8] | 吴关, 姜春岩, 鲁谊, 朱以明, 李奉龙, 李旭. 改良关节镜下喙突移位Latarjet手术治疗肩关节前方不稳定[J]. 北京大学学报(医学版), 2015, 47(2): 321-325. |
| [9] | 李奉龙, 姜春岩, 鲁谊, 朱以明, 李旭. 肩关节镜下喙锁韧带重建术与切开改良Weaver-Dunn手术治疗肩锁关节脱位的疗效比较[J]. 北京大学学报(医学版), 2015, 47(2): 253-257. |
| [10] | 朱以明, 姜春岩, 鲁谊, 李奉龙, 李旭, 李岳. 切开Latarjet 手术治疗复发性肩关节前脱位的临床随访研究[J]. 北京大学学报(医学版), 2015, 47(2): 226-231. |
|
||